When does Medicare Part B coverage kick in?
After you have paid $185 out of your own pocket, your Part B coverage will kick in. Part B covers: Medicare Supplement Insurance (Medigap) Plan F and Plan C both provide full coverage for the 2019 Part B deductible. However, both plans will not be available to new Medicare beneficiaries after Jan. 1, 2020.
Why do I have to pay more for Medicare Part B?
If your income is high enough, you may pay more for your Part B premium each month. Medicare measures your modified adjusted gross income to determine your income level. Depending on how much money you make, you may have to pay an Income Related Monthly Adjustment Amount (IRMAA) on top of your Part B premium.
What is the Medicare Part A benefit period and how does it work?
What is the Medicare Part A benefit period? You might be familiar with how health insurance works when it comes to deductibles and copayments. For major medical plans, you typically have one deductible that applies for the whole calendar year of your coverage. In other words, you just pay it once.
What is a Medicare Part B premium?
Part B premiums. Most people will pay the standard premium amount. If your modified adjusted gross income is above a certain amount, you may pay an Income Related Monthly Adjustment Amount (IRMAA). Medicare uses the modified adjusted gross income reported on your IRS tax return from 2 years ago.

What does Medicare consider a calendar year?
The Medicare Part D plan year runs from January 1st through December 31st of each year, so the plan year runs for a calendar year rather than 365 days from the date of your initial enrollment (or Initial Enrollment Period).
How do Medicare benefit periods work?
A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins.
Does Part B go up every year?
Remember, Part B Costs Can Change Every Year The Part B premium is calculated every year. You may see a change in the amount of your Social Security checks or in the premium bills you receive from Medicare.
What is the benefit period for Medicare Part B deductible?
A benefit period begins the day you are admitted to a hospital as an inpatient, or to a SNF, and ends the day you have been out of the hospital or SNF for 60 days in a row. After you meet your deductible, Original Medicare pays in full for days 1 to 60 that you are in a hospital.
Does Medicare Part B run on a calendar year?
Yes, Medicare Part B does run on a calendar year. The annual deductible will reset each January 1st.
What is the difference between calendar year and benefit year?
A plan on a calendar year runs from January 1–December 31. Items like deductible, maximum out-of-pocket expense, etc. will reset every January 1. All Individual and Family plans are on a calendar year. A plan on a contract year (also called benefit year) runs for any 12-month period within the year.
What is the standard Medicare Part B premium for 2021?
$148.50Medicare Part B Premium and Deductible The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
How do I get my $144 back from Medicare?
Even though you're paying less for the monthly premium, you don't technically get money back. Instead, you just pay the reduced amount and are saving the amount you'd normally pay. If your premium comes out of your Social Security check, your payment will reflect the lower amount.
What is the Medicare Part B premium for 2022?
$170.10The standard Part B premium amount in 2022 is $170.10. Most people pay the standard Part B premium amount. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA).
What does calendar year mean for benefits?
A calendar year deductible, which is what most health plans operate on, begins on January 1st and ends on December 31st. Calendar-year deductibles reset every January 1st. A plan year deductible resets on the renewal date of your company's plan.
Does Medicare deductible start over every year?
Medicare deductibles are reset each year and the dollar amount may be subject to change. Both Medicare Parts A and B have deductibles that must be met before Medicare starts paying. Medicare Advantage, Medigap and Part D plans are all sold by private insurance companies that set their own deductibles.
What is meant by benefit period?
A benefit period is the length of time during which an insurance policyholder or their dependents may file and receive payment for a covered event. All insurance plans will include a benefit period, which can vary based on policy type, insurance provider, and policy premium.
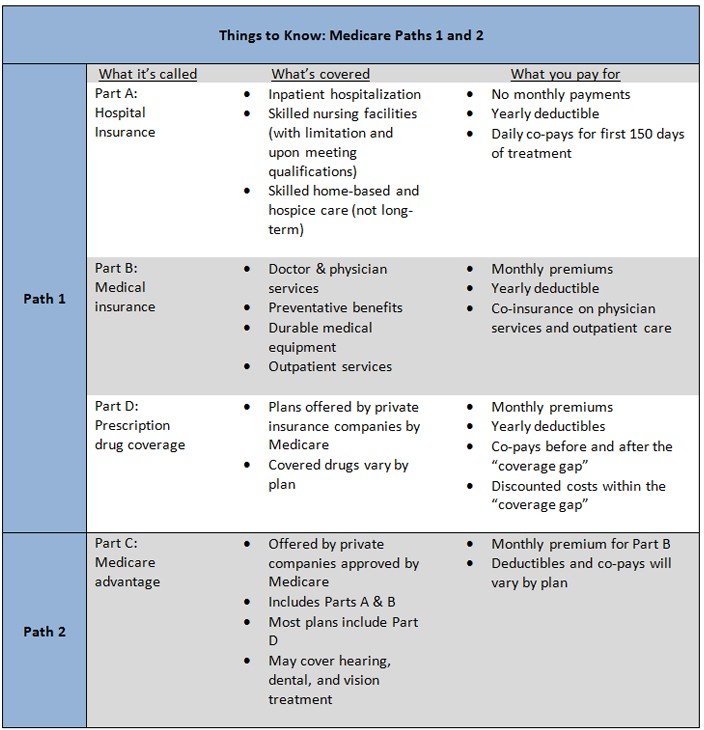
What is Part B?
Part B covers 2 types of services. Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is Medicare benefit period?
Medicare benefit periods mostly pertain to Part A , which is the part of original Medicare that covers hospital and skilled nursing facility care. Medicare defines benefit periods to help you identify your portion of the costs. This amount is based on the length of your stay.
How long does Medicare Advantage last?
Takeaway. Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of the facility for at least 60 days.
How much coinsurance do you pay for inpatient care?
Days 1 through 60. For the first 60 days that you’re an inpatient, you’ll pay $0 coinsurance during this benefit period. Days 61 through 90. During this period, you’ll pay a $371 daily coinsurance cost for your care. Day 91 and up. After 90 days, you’ll start to use your lifetime reserve days.
How long does Medicare benefit last after discharge?
Then, when you haven’t been in the hospital or a skilled nursing facility for at least 60 days after being discharged, the benefit period ends. Keep reading to learn more about Medicare benefit periods and how they affect the amount you’ll pay for inpatient care. Share on Pinterest.
What facilities does Medicare Part A cover?
Some of the facilities that Medicare Part A benefits apply to include: hospital. acute care or inpatient rehabilitation facility. skilled nursing facility. hospice. If you have Medicare Advantage (Part C) instead of original Medicare, your benefit periods may differ from those in Medicare Part A.
Why is it important to check deductibles each year?
It’s important to check each year to see if the deductible and copayments have changed, so you can know what to expect. According to a 2019 retrospective study. Trusted Source. , benefit periods are meant to reduce excessive or unnecessarily long stays in a hospital or healthcare facility.
How much is Medicare deductible for 2021?
Here’s what you’ll pay in 2021: Initial deductible. Your deductible during each benefit period is $1,484. After you pay this amount, Medicare starts covering the costs. Days 1 through 60.
What Is The Medicare Part B Give Back Benefit?
The Give Back benefit is a benefit offered by some Medicare Advantage plan carriers that can help you reduce your Medicare Part B premium. You should know, however, that the Give Back benefit is not an official Medicare program. This benefit is provided as part of some Medicare Part C plans as a way to encourage participation in a specific plan.
Who Is Eligible For The Medicare Part B Give Back Benefit?
It is pretty easy to qualify for the Medicare Give Back benefit as the eligibility criteria are straightforward. First, you must be enrolled in Original Medicare. You need to have both Medicare Part A and Medicare Part B coverage. Next, you must pay your own monthly Part B premium.
Applying For A Medicare Part B Give Back Benefit
So, what is the enrollment process for the Give Back benefit? Many people are looking to save as much money as possible when it comes to their health care costs, so they want to know how to get signed up for this program. The process is quite simple, so here is how to do it.
The Bottom Line
Since most people on Medicare are receiving Social Security benefits, finding a way to reduce the cost of your health insurance is always a plus. The Medicare Give Back program can do just that by paying for a portion or even all of your Medicare Part B premium.
What is the deadline for Medicare give back benefit?
There is no deadline to qualify for the give back benefit. You must already be enrolled in Medicare Part A and Part B, and you must pay your own monthly Part B premium. You then simply need to enroll in a Medicare Advantage plan that offers this benefit.
What happens after 90 days of Medicare?
After day 90 in a benefit period, and if the person has no more lifetime reserve days available to use, the Medicare recipient is responsible to pay all of the costs associated with their hospital stay. After you’ve spent 60 days out of the hospital, your benefit period will start all over again. At the start of each new period, you will receive ...
How long does Medicare cover in-hospital care?
After this deductible is met, Medicare will start to cover the remainder of your costs for in-hospital services, such as food, nursing and your bed, for a limit of 60 days following your date of admission. There is $0 copay or coinsurance during this period of time as well. Should you spend the entire period in the hospital, ...
How many days do you have to be out of the hospital to get Medicare?
In order to help you make better sense of this, here’s a breakdown. 60 days: How many days you are required to be out of the hospital or after-care facility to become eligible for another hospital benefit period. 60 days: The maximum number of days that Medicare will pay for all of your inpatient hospital care once you’ve paid your deductible ...
How long do you have to stay in a hospital?
In an Original Medicare plan, you have to stay for a minimum of three days, or more than two nights, to officially be admitted as a patient in a hospital. Only then will Medicare start to pay for your care in a skilled nursing center for additional treatment, like physical therapy or for regular IV injections. The amount of time you spend in the hospital as well as the skilled nursing center will be counted as part of your hospital benefit period. Furthermore, you are required to have spent 60 days out of each in order to be eligible for another benefit period.#N#However, the portion you are expected to pay for the costs of a skilled nursing center differs from the portion you pay for hospital care. In facilities like these, you must pay in any given benefit period: 1 $0 for your room, bed, food and care for all days up to day 20 2 A daily coinsurance rate of $161 for days 21 through 100 3 All costs starting on day 101
How much is Medicare coinsurance?
The Medicare recipient is charged a daily coinsurance for any lifetime reserve days used. The standard coinsurance amount is $682 per day. If you’re enrolled in a supplemental Medicare insurance program, also known as “Medigap,” you will receive another 365 days in your lifetime reserve with no additional copayments.
How much is the hospital stay deductible for Medicare?
You will be expected to pay for the initial cost of your hospital stay up to a limit of $1,364. This is your hospital deductible for Medicare Part A. As opposed to other Medicare deductibles, it begins anew with every hospital benefit period, rather than your first admission to the hospital each year. After this deductible is met, Medicare will ...
How long do you have to be hospitalized before you can be moved to a skilled nursing facility?
For instance, with most policies, you don’t have to be hospitalized for three days before you can be moved to a skilled nursing center.
How does Medicare Part B work?
How it Works Premiums & Deductibles Coverage & Enrollment FAQs. Medicare Part B provides the medical portion of your Medicare coverage . Part B has costs, including a premium, deductible and coinsurance. Together, they make up the overall cost of Medicare Part B. But the costs aren’t the same for everyone.
What is Medicare premium?
A premium is a fee you pay to your insurance company for a health plan coverage. This is usually a monthly cost. A deductible is the amount you pay out of pocket before your insurance company covers its ...
What is premium insurance?
A premium is a fee you pay to your insurance company for a health plan coverage. This is usually a monthly cost. and annual deductible. A deductible is the amount you pay out of pocket before your insurance company covers its portion of your medical bills. For example: If your deductible is $1,000, your insurance company will not cover any costs ...
Does Medicare Supplement Insurance cover Part B?
Medicare Supplement Insurance (Medigap) has several policies that will help cover your Part B costs, including premiums, deductibles and out-of-pocket costs.
Is Medicare Part B based on income?
Unlike the Part B premium, this amount isn’t based on income. Everyone enrolled in Original Medicare pays the same Part B deductible. That means no matter how high your income is, you’ll pay the standard Medicare Part B deductible amount.
Is Medicare Part B the same as Medicare Advantage?
But Part B coverage isn’t exclusive to Original Medicare; you’ll receive at least the same benefits with Medicare Advantage (Part C).
Does Medicare cover wheelchairs?
Medically necessary: Your doctor must deem your treatment is required to improve or maintain your health. Preventive services: Medicare-approved screenings and other preventive services are covered and generally at no-cost. Part B can also cover wheelchairs and other medically necessary equipment.
How much is Medicare Part B 2021?
The standard Part B premium for 2021 is $148.50 to $504.90 per month depending on your income. However, some people may pay less than this amount because of the “hold harmless” rule. The rule states that the Part B premium may not increase more than the Social Security Cost of Living Adjustment (COLA) increase in any given year. In short, this provision prevents your Social Security checks from declining year-over-year and caps Medicare Part B premium increases to be no more than the amount of your COLA.2
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What happens if you don't receive Medicare?
In this case, Medicare will send you a bill for Part B coverage called the Medicare Premium Bill. Read this article for five ways to pay your Part B premium payments.
Do you get Social Security if you are new to Medicare?
You are new to Medicare. You don’t get Social Security benefits. You pay higher premiums due to having a higher income. Additionally, people with higher incomes may pay more than the standard Part B premium amount due to an “income-related monthly adjustment.”.
Does Medicare Part B increase?
In short, this provision prevents your Social Security checks from declining year-over-year and caps Medicare Part B premium increases to be no more than the amount of your COLA.2. For people who are not “held harmless” the Part B premiums can increase as much as necessary until the standard rate is reached for the given year.
What happens after you meet your Medicare Part B deductible?
What Happens After You Meet the Part B Deductible? After you reach your Medicare Part B deductible, you will typically pay a 20% coinsurance for all services and items that are covered by Part B for the remainder of 2019. On Jan. 1, 2020, your deductible will reset, and you will have to pay the 2020 Medicare Part B deductible before your Part B ...
How much is Medicare Part B deductible?
The 2019 Part B deductible is $185 per year (up from $183 in 2018). This guide also explores the Part B deductible and some of the other 2019 Medicare Part B costs you may face, as well as ways you can get coverage for some of your Medicare Part B costs.
What is the Medicare Part B deductible for 2019?
As mentioned above, the annual Medicare Part B deductible for 2019 is $185. So what exactly does that mean? You are responsible for the first $185 worth of services or items that are covered by Medicare Part B that you receive in the calendar year of 2019.
How much is the $65 out of pocket for Part B?
After the $65 is paid, you have reached $185 in out-of-pocket spending for covered Part B services in 2019. You have reached your deductible and you will now be responsible for any Part B coinsurance charges. There is still $85 remaining for your doctor's visit ($150 total charge minus the $65 you paid out of pocket).
What is the 2019 Medicare premium based on?
So that means your 2019 premiums are based off of your reported income from 2017. Most people pay the standard Part B premium amount, but higher income earners may pay a higher amount called the Income-Related Monthly Adjusted Amount, or IRMAA.
What is Part B insurance?
Part B covers: Qualified medical care, such as doctor's office visits and procedures. Certain preventive care. Some durable medical equipment (DME) Medicare Supplement Insurance (Medigap) Plan F and Plan C both provide full coverage for the 2019 Part B deductible.
How much is a knee injury deductible in July?
In July, you injure your knee and schedule another appointment with your doctor. This time you are billed $150 for the appointment. You will be responsible for paying the first $65 of the $150 for the appointment out of your own pocket, because that is how much is left on your deductible. After the $65 is paid, ...