
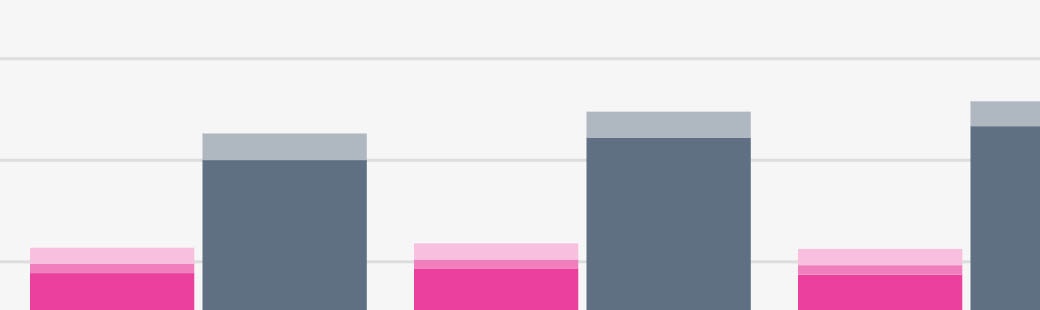
Researchers found that the costs related to falls was significant. “A substantial share of healthcare expenditures for adults aged 65 and older was attributable to falls,” accounting for about 6 percent of Medicare expenditures and 8 percent of Medicaid costs. Of the $50 billion, almost 99 percent was spent in the aftermath of nonfatal falls.
Full Answer
Does Medicare cover falls and falls prevention?
Despite taking the necessary precautions, falls can still occur. Getting help immediately is extremely important, and your Medicare insurance can help cover the costs of your care. Medicare Part B (Medical Insurance) can help cover the costs of doctor visits and preventive care.
What is the cost of Falls among older adults?
Cost of Older Adult Falls Falls among adults age 65 and older are very costly. Each year about $50 billion is spent on medical costs related to non-fatal fall injuries and $754 million is spent related to fatal falls. 1
What happens when you fall at home?
Falls can cause broken bones, fractures, and even traumatic brain injury. According to the Centers for Disease Control and Prevention (CDC), approximately 800,000 people are hospitalized each year from falls. Seniors are at a higher risk for falls at home.
Do nurses become afraid of falls to achieve zero falls?
Results: Intense messaging from hospital administration to achieve zero falls resulted in nurses developing a fear of falls, protecting self and unit, and restricting fall risk patients as a way to stop messages and meet the hospital goal.
What does Medicare consider a fall?
Falls - The MDS defines a fall as unintentionally coming to rest on the ground, floor, or other lower level but not as a result of an overwhelming external force (e.g., resident pushes another resident).
Does Medicare reimburse for falls?
Generally, Medicare covers treatment for your injuries if you fall. Original Medicare is the federal health insurance program that consists of Part A (hospital insurance) and Part B (medical insurance).
What is the expected impact of Medicare and Medicaid institution of never events for which they will not pay?
What is the expected impact of Medicare and Medicaid's institution of "never events" for which they will not pay? Patient safety will improve. Integrated systems will dominate because they: have the flexibility to survive rough times.
What is the financial impact of patient falls with injury?
The Real Numbers Of those patients who fall, 30%-35% will sustain an injury, and each injury, on average, adds more than six days to a patient's hospital stay. That adds up to an average cost of a fall with injury to more than $14,000 per patient.
Are falls a never event?
As noted above, falls with injury are a serious reportable event for The Joint Commission and are considered a "never event" by CMS.
Does Medicare cover fall prevention program?
Medicare Advantage contracts with community-based organizations to provide falls prevention programs to beneficiaries. Falls prevention programs that lead to significant behavioral changes avert medical costs.
Which of the following is considered a never event by the Centers for Medicare and Medicaid Services CMS is not reimbursable?
Examples of “never events” include surgery on the wrong body part; foreign body left in a patient after surgery; mismatched blood transfusion; major medication error; severe “pressure ulcer” acquired in the hospital; and preventable post-operative deaths.
What constitutes a never event?
Never Events are defined as Serious Incidents that are wholly preventable because guidance or safety recommendations that provide strong systemic protective barriers are available at a national level and should have been implemented by all healthcare providers.
Are falls reported to CMS?
CMS stopped reimbursing health care costs related to hospital-acquired falls in 2008. This policy may have influenced changes in practice patterns among nurses in community and tertiary hospitals. Specifically, nurses may have increased the implementation of fall prevention measures.
What is the average cost of a fall?
How Are State Costs Calculated?Location Sort by location in no orderTotal Cost Sort by total cost in no orderPrivate/Out of Pocket Sort by private/out of pocket in no orderArizona$857,000,000$116,000,000Arkansas$436,000,000$48,000,000California$4,371,000,000$652,000,000Colorado$478,000,000$96,000,00047 more rows
What are the 3 types of falls?
Falls can be classified into three types:Physiological (anticipated). Most in-hospital falls belong to this category. ... Physiological (unanticipated). ... Accidental.
What is the true cost of a fall in a healthcare facility?
The financial cost of a fall It is estimated that this figure will rise to around $54.9 billion by 2020. Direct medical costs were calculated to include hospital and nursing home fees, doctors and professional services, use of medical equipment, prescription drugs, etc.
How to reduce fall risk?
A proper diet and some light exercise can keep your body alert and energetic. It can also help maintain your strength, endurance and flexibility, which can all reduce your fall risk.
Why do older people fall?
A lack of adequate nutrition can cause side-effects such as lightheadedness and weakness, which can further increase the risk of a fall.
What is fall prevention?
Each state has a fall prevention coalition, which is an organization that aims to reduce falls in older adults. Each state coalition may differ in the approach taken to prevent falls.
Can tight clothing affect mental health?
This can impede motor skills and – in some cases – negatively impact short term mental capacity.
What are the factors that can be changed to help prevent falls?
Many risk factors can be changed or modified to help prevent falls. They include: Lower body weakness. Vitamin D deficiency (that is, not enough vitamin D in your system) Difficulties with walking and balance. Use of medicines, such as tranquilizers, sedatives, or antidepressants.
What are the causes of falls?
broken or uneven steps, and. throw rugs or clutter that can be tripped over. Most falls are caused by a combination of risk factors. The more risk factors a person has, the greater their chances of falling. Healthcare providers can help cut down a person’s risk by reducing the fall risk factors listed above.
How to prevent falling?
What You Can Do to Prevent Falls. Falls can be prevented. These are some simple things you can do to keep yourself from falling. Talk to Your Doctor. Ask your doctor or healthcare provider to evaluate your risk for falling and talk with them about specific things you can do.
How many older people fall each year?
Facts About Falls. Each year, millions of older people—those 65 and older—fall. In fact, more than one out of four older people falls each year, 1 but less than half tell their doctor. 2 Falling once doubles your chances of falling again. 3.
What percentage of hip fractures are caused by falling?
More than 95% of hip fractures are caused by falling, 8 usually by falling sideways. 9. Falls are the most common cause of traumatic brain injuries (TBI). 10. In 2015, the total medical costs for falls totaled more than $50 billion. 11 Medicare and Medicaid shouldered 75% of these costs.
Can a fall cause a broken bone?
Many falls do not cause injuries. But one out of five falls does cause a serious injury such as a broken bone or a head injury. 4,5 These injuries can make it hard for a person to get around, do everyday activities, or live on their own. Falls can cause broken bones, like wrist, arm, ankle, and hip fractures. Falls can cause head injuries.
Can a fall cause a head injury?
Falls can cause head injuries. These can be very serious, especially if the person is taking certain medicines (like blood thinners). An older person who falls and hits their head should see their doctor right away to make sure they don’t have a brain injury.
What percentage of Medicare is attributed to falls?
“A substantial share of healthcare expenditures for adults aged 65 and older was attributable to falls,” accounting for about 6 percent of Medicare expenditures and 8 percent of Medicaid costs.
What age group is at highest risk of falls?
Of particular note, the study found that people age 85 or older are “at highest risk of falls” while being the “fastest-growing segment” of the older population. “Therefore, the economic burden from falls is likely to increase substantially in the coming years,” study authors wrote, noting that “75 percent of the cost of older adult falls is ...
When a resident falls who has already been entered into the FMP, should the nurse send a FAX alert
When a resident falls who has already been entered into the FMP, the nurse should send a FAX Alert to the primary care provider. The purpose of this alert is to inform the physician, nurse practitioner or physician's assistant of the resident's most recent fall as well as the resident's total number of falls during the previous 180 days.
What should a nurse do after a resident falls?
Upon evaluation, the nurse should stabilize the resident and provide immediate treatment if necessary.
What is the FMP assessment?
In addition to the clues discovered during immediate resident evaluation and increased monitoring, the FMP Falls Assessment is used for a more in-depth look at fall risk. Five areas of risk accepted in the literature as being associated with falls are included. They are:
How long does it take to develop a fall care plan?
Results of the Falls Assessment, along with any orders and recommendations, should be used by the interdisciplinary team to develop a comprehensive falls care plan within 1-7 days after the fall. The Fall Interventions Plan should be used by the Falls Nurse Coordinator as a worksheet and to record the final interventions selected for the resident. The interventions listed on this form are grouped in the same five risk areas used for the Falls Assessment.
What is the section A of the TRIPS form?
Section A includes basic resident information, methods for documentation in the medical record and notification of the primary care provider and family. In section B there are questions related to 1) circumstances, 2) staff response and 3) resident and care outcomes.
What is an immediate response?
An immediate response should help to reduce fall risk until more comprehensive care planning occurs. Therefore, an immediate intervention should be put in place by the nurse during the same shift that the fall occurred.
What is a written full description of all external fall circumstances at the time of the incident?
A written full description of all external fall circumstances at the time of the incident is critical. This includes factors related to the environment, equipment and staff activity. ( Figure 1)
