Other examples of how Medicare supplement plans work with Medicare include:
- All plans include coverage for blood work at varying levels; Plan K covers it 50 percent and Plan L covers it at 75...
- If you have to endure a lengthy hospital stay, a Medicare supplement plan can save you money. For example, coinsurance...
- Medicare supplement plans don’t cover routine dental or...
Full Answer
What are the top 5 Medicare supplement plans?
- Plan G
- Plan N
- Plan A
- Plan F
- High Deductible Plan F
Are Medicare supplement plans worth it?
Medicare Supplement plans are worth it; doctor freedom, low out of pocket costs, and when Medicare pays the claim, your supplemental Medicare plan will pay the rest. Our team of experts is ready to answer your questions are share the most popular Medigap plans in your area. Call us today to find out if Medicare Supplements are worth it for you!
What is the best Medicare supplement insurance plan?
- United Healthcare: 26%
- Humana: 18%
- BCBS plans: 15%
- CVS (Aetna): 11%
- Kaiser Permanente: 7%
- Centene: 4%
- Cigna: 2%
- Other companies: 18%
How to choose the best Medicare supplement plans?
How to choose the best Medicare supplement plans. The best Medicare supplement plan for you will depend on which Original Medicare parts you need filled and the cost of the plan.You should choose the supplement policy that provides the best benefits for you and fills in the coverage gaps where you expect to spend the most on health care.
What does Medicare Supplement plan I cover?
Plan I includes the Basic Benefits, Pays the Part A deductible and Skilled Nursing Coinsurance. Plan I Includes Foreign Travel Emergency benefits. Plan I includes at home recovery.
Is there a Medicare Supplement that covers everything?
Medicare Supplement insurance Plan F offers more coverage than any other Medicare Supplement insurance plan. It usually covers everything that Plan G covers as well as: The Medicare Part B deductible at 100% (the Part B deductible is $203 in 2021).
How do supplemental insurance plans work?
Supplemental health insurance is a plan that covers costs above and beyond what standard health policies will pay. It may provide extra coverage. It may even pay for costs not covered by a traditional health plan, such as coinsurance, copays, and deductibles.
How are Medicare supplements divided?
Supplemental insurance plans are divided into categories with an alphabetic label. Medigap plans in tiers A through K provide the highest cost sharing benefits, while plans K through N plans provide less cost coverage.
What are the top 3 most popular Medicare Supplement plans in 2021?
Three Popular Medicare Supplement PlansBlue Cross Blue Shield. According to Blue Cross Blue Shield (BCBS), Plans F and N are available in most areas. ... AARP United Healthcare. The United Healthcare Medicare Supplement plan is also very popular. ... Humana.
How much is Medicare Supplement monthly?
Medicare Supplement Plans have premiums that cost anywhere from around $70/month to around $270/month. Typically, plans with higher monthly premiums will have lower deductibles.
Why is it not a good idea to have supplemental insurance?
For example, it may not cover all the expenses you expected; it may impose waiting periods before payments start; or it may contain limits based on how much you paid and for how long. It is important to understand that supplemental insurance is not regulated by the Affordable Care Act.
Does Medicare Supplement pay Part A deductible?
Most Medicare Supplement insurance plans cover the Part A deductible at least 50%. All Medicare Supplement plans also cover your Part A coinsurance and hospital costs 100% for an additional 365 days after your Medicare benefits are used up.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
What is the difference between a Medicare Advantage plan and a Medicare Supplement?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
How many pints of blood are covered by Medicare Supplement core benefits?
three pintsHow many pints of blood will be paid for by Medicare Supplement core benefits? Medicare Supplement core policy benefits will pay for the first three pints of blood.
How many Medicare Supplement Plans are there?
These plans cover more than just out-of-pocket costs from Medicare and may provide additional benefits for some people. Currently, 10 Medicare supplement plans are available. These are:
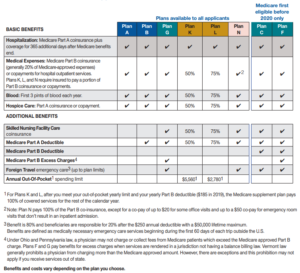
What does "no" mean in Medicare Supplement?
“Yes” under a plan letter means that it covers 100% of the benefit. “No” under a plan letter means that it does not cover that benefit.
How long does Medicare Part A coinsurance last?
Part A coinsurance includes coverage for an extra 365 days worth of hospital costs after using Medicare Part A.
What is the difference between coinsurance and deductible?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%.
What is a copayment for Medicare?
Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs. This article explains how Medicare supplement plans work, how to find one, and how to work out which plan is best.
What is the primary payer for Medicare?
If a person has more than one insurance policy, they will have decided on a primary or secondary payer. Medicare parts A and B , which would serve as the primary payer, administer their coverage first.
Which states have Medigap policies?
However, Wisconsin, Minnesota, and Massachusetts have all set their own standards for administering Medigap policies. People who live in one of these states should check with Medicare directly to confirm their local standards.
What are Medicare Supplement Plans?
Medicare Supplement plans, also known as Medigap, are supplement insurance plans that work with Original Medicare Part A and Part B.
What are High-Deductible Medicare Supplement Plans?
There are two high-deductible Medicare Supplement Plans available. High deductible Plan F and Plan G both have a regular version and a “high-deductible” version. Since the policyholder is agreeing to accept more out-of-pocket expenses for their annual healthcare expenses, the insurance company offers the plan at a lower monthly premium.
Why is Medicare Supplement important?
If you choose the original Medicare option, Medicare supplement plans are important because these plans add an extra element, or boost, to your main coverage by paying for gaps for stand-alone prescription drug plans, employer group health coverage and other retiree benefits. Original Medicare will pay first, followed by the payment by ...
How many Medicare supplement plans are there?
How Medicare supplement insurance plans work with Medicare plans. There are up to 10 standardized plans available – labeled A, B, C, D, F, G, K, L, M and N – that cover anywhere from four to nine of these benefits:
What are the benefits of Medicare?
There are up to 10 standardized plans available – labeled A, B, C, D, F, G, K, L, M and N – that cover anywhere from four to nine of these benefits: 1 Medicare Part A coinsurance for hospital costs (up to an additional 365 days after Medicare benefits are used) 2 Medicare Part B coinsurance, copayment 3 First three pints of blood for a medical procedure 4 Part A hospice care coinsurance or copayment 5 Skilled nursing facility care coinsurance 6 Part A deductible 7 Part B deductible 8 Part B excess charges 9 Foreign travel emergencies
What to do before making a final decision on Medicare supplement insurance?
Before making any final decisions regarding Medicare and Medicare supplement insurance, speak to a policy expert professional to make sure you are covered properly and your premium is affordable for your budget.
How much does coinsurance cost for hospitalization?
For example, coinsurance for hospitalization costs $335 per day for days 61-90. Beyond day 90, the cost is $670 until a lifetime reserve is met, in which case you must pay the rest of the costs. Keep in mind you must pay your Medicare Part A deductible ($1,340 for 2018) before receiving these benefits. Medicare supplement plans don’t cover routine ...
How long does Medicare cover hospital coinsurance?
Medicare Part A coinsurance for hospital costs (up to an additional 365 days after Medicare benefits are used) Keep in mind, all 10 Medicare supplement plans cover the coinsurance and 100 percent of hospital costs for Medicare Part A, but after that, plans differ in what they cover. For example, only Medicare supplement plans C and F cover ...
Do you have to leave Medicare first?
If you have a Medicare Advantage Plan, you must leave it first before your new Medicare supplement (Medigap) policy begins; apply for the Medigap plan first before you leave your other plan. Buy a Medigap policy from an insurance company licensed in your state to sell them.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
Does Medicare cover prescription drugs?
Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage. If you want prescription drug coverage, you can join a Medicare Prescription Drug Plan (Part D). If you buy Medigap and a Medicare drug plan from the same company, you may need to make 2 separate premium payments. Contact the company to find out how to pay your premiums.
Does Medigap cover everything?
Medigap policies don't cover everything. Medigap policies generally don't cover. long-term care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
Does Medicare cover hospice?
Through Original Medicare, Part A covers hospice care, but patients may be charged copayments or coinsurances for certain services; Plan N covers these costs. Copayments and coinsurances with Part B are almost entirely covered, however, some office visits may still require a $20 copay. Emergency room visits, which fall under Part B coverage terms, will require a $50 copay when the recipient is not admitted for inpatient care. Plan N covers 80% of the cost of care received while traveling outside of the country.
Does Medicare Supplement Plan N cover coinsurance?
This also extends inpatient coverage for up to 365 days once Part A’s inpatient coverage is used up. Plan N also covers 100% of the coinsurance at a skilled nursing facility. The first 3 pints of blood transfusion are also a fully covered hospital benefit.
Why buy Medicare Supplement Insurance?
Buy a Medicare Supplement Insurance (Medigap) policy to help lower your share of costs for services you get.
How does Original Medicare work?
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them. There’s no limit on what you’ll pay out-of-pocket in a year unless you have other coverage (like Medigap, Medicaid, or employee or union coverage). Get details on cost saving programs.
What is Medicare Advantage?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
Is Medicare a private insurance?
Medicare is different from private insurance — it doesn’t offer plans for couples or families. You don’t have to make the same choice as your spouse.
Does Medicare cover urgent care?
Plans must cover all emergency and urgent care, and almost all medically necessary services Original Medicare covers. Some plans tailor their benefit packages to offer additional benefits to treat specific conditions.
When did Medicare start providing prescription drugs?
Since January 1, 2006, everyone with Medicare, regardless of income, health status, or prescription drug usage has had access to prescription drug coverage. For more information, you may wish to visit the Prescription Drug Coverage site.
How long do you have to be on disability to receive Social Security?
You have been entitled to Social Security or Railroad Retirement Board disability benefits for 24 months. ( Note: If you have Lou Gehrig's disease, your Medicare benefits begin the first month you get disability benefits.)
What Is a Medicare Supplement Insurance Plan?
Medicare Supplement Insurance plans provide additional coverage to supplement Original Medicare.
What is Medicare Supplement?
Medicare Supplement insurance plans are private insurance plans that are offered to help bridge the gap between the coverage you need and what is offered through Medicare. While Medicare pays for a large percentage of the healthcare services and supplies you may need, it does not offer complete coverage, so Medicare Supplement insurance plans can ...
Who is Eligible for a Medigap Plan?
Anyone who is eligible for Medicare and enrolled in Part A and Part B may be eligible to purchase a Medigap Plan. If you miss your Medigap Open Enrollment period, you may not be able to purchase a policy depending on your health condition. You cannot have a Medigap policy and a Medicare Advantage Plan at the same time.
How Much Does a Medigap Plan Cost?
You pay a monthly premium for your Medigap plan. This premium varies depending on benefits offered, when you purchase your policy, how it is priced, and in which state you reside. Because Medigap plans are offered through private insurance companies, the companies set their premiums. Monthly premium costs may increase each year based on age, inflation, or other factors.
How Do I Enroll in a Medigap Plan?
There are certain situations which may give you guaranteed issue rights to purchase a Medigap policy, regardless of your health conditions or any preexisting health conditions.
How long do you have to enroll in Medicare Supplement?
If you choose to join a Medicare Supplement plan, you should do so during your six-month open enrollment period, which is the initial six months when you first become eligible for Medicare. It starts the month you turn 65 and as soon as you are signed up for Medicare Part B. The benefit of enrolling in a Medigap policy during the open enrollment period is that you are guaranteed coverage to purchase, no matter your health conditions , and you may lock in at a lower price and premium. After your enrollment period is over, you may have more difficulty finding coverage based on your health conditions, and your costs and premiums may be higher as well.
What happens when you buy a Medicare Supplement?
When you purchase a Medicare Supplement insurance plan, your Medigap policy will serve as a secondary source of insurance. That means that Medicare will be used first to pay for any Medicare-approved costs for any healthcare supplies and services. After Medicare has been applied, then your Medigap policy will be charged.
