
An advance written notice of non-coverage helps Medicare Fee-for-Service (FFS) patients choose items and services Medicare usually covers but may not pay because they’re medically unnecessary or custodial in nature. The Advance Beneficiary Notice helps patients decide whether to get the item or service Medicare may not cover and accept financial responsibility. If you don’t provide the patient with required written notices, Medicare may hold you financially liable if they deny payment. This booklet explains the Advance Beneficiary Notice-issued notice types, uses, and timing.
What are non covered charges?
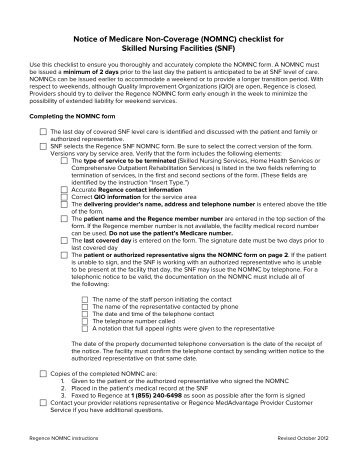
A Notice of Medicare Non-Coverage (NOMNC) is a notice that indicates when your care is set to end from a home health agency (HHA), skilled nursing facility (SNF), comprehensive outpatient rehabilitation facility (CORF), or hospice. It includes information for how to appeal the provider ’s decision to a Quality Improvement Organization (QIO).
How to obtain Medicaid denial letter?
Issuing an Advance Written Notice of Non-coverage as a Courtesy. Medicare doesn’t require you to notify the patient before you provide an item or service we never cover or isn’t a Medicare benefit. However, as a courtesy, you may issue a voluntary notice to alert the patient about their financial liability.
What is Medicare non covered service?
NOTICE OF MEDICARE NON-COVERAGE Patient Name: Patient ID Number: THE EFFECTIVE DATE COVERAGE OF YOUR CURRENT {insert type} SERVICES WILL END: {insert effective date} • Your MedicareAdvantage (MA) plan and/or provider have determined that Medicare probably will not pay for your current {insert type} services after the effective date
Is ABN only for Medicare?
You'll get this notice each year if you have drug coverage from an employer/union or other group health plan. This notice will let you know whether or not your drug coverage is “creditable.”.
When must you provide a client with an Nomnc Notice of Medicare non-coverage?
The NOMNC must be delivered at least two calendar days before Medicare covered services end or the second to last day of service if care is not being provided daily. Note: The two day advance requirement is not a 48 hour requirement.
What is an Advance beneficiary Notice of Non-Coverage?
The Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, is issued by providers (including independent laboratories, home health agencies, and hospices), physicians, practitioners, and suppliers to Original Medicare (fee for service - FFS) beneficiaries in situations where Medicare payment is expected to be ...
Can you bill a Medicare patient for a non covered service without an ABN?
An ABN is not required, but a conversation with your patient before the services are rendered would be appropriate. For example, a 67-year-old established patient presents for a covered service, such as an office visit for a chronic illness (e.g., 99213).
What document must be provided to Medicare patients when Medicare is unlikely to cover a service?
What document must be provided to Medicare patients when Medicare is unlikely to cover a service? Must be given a copy of the Medicare Advance Beneficiary Notice (ABN).
What does advance beneficiary notice mean?
An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying you: Medicare may deny payment for that specific procedure or treatment. You will be personally responsible for full payment if Medicare denies payment.
Are ABNs only for Medicare patients?
ABNs only apply to patients who are enrolled directly with Medicare, not patients who have coverage through a Medicare product from a private insurance company.
What is a non-covered service?
A service can be considered a non-covered service for many different reasons. Services that are not considered to be medically reasonable to the patient's condition and reported diagnosis will not be covered. Excluded items and services: Items and services furnished outside the U.S.
What form is provided to a patient to indicate a service may not be covered by Medicare and the patient may be responsible for the charges?
Advance Beneficiary Notice (ABN)An Advance Beneficiary Notice (ABN), also known as a waiver of liability, is a notice a provider should give you before you receive a service if, based on Medicare coverage rules, your provider has reason to believe Medicare will not pay for the service.
What Medicare form is used to show charges to patients for potentially non-covered services?
(Medicare provides a form, called an Advance Beneficiary Notice (ABN), that must be used to show potentially non-covered charges to the patient.)
Which of the following criteria is used to determine medical necessity?
A patient's diagnosis is one criterion that drives medical necessity from a payer's perspective. From a clinical perspective, medical necessity is determined by the provider based on evidence-based medical data.
When should an ABN not be issued?
If the provider does not have a reasonable belief that the service or item that is normally payable will be denied than an ABN is prohibited from being issued. Other circumstances were you are prohibited from issuing an ABN include: To make a beneficiary liable for Medically Unlikely Edit (MUE) denials.
Why is ABN important to the provider?
An ABN is important because it allows a provider to administer a service to a Medicare patient that may not be covered by Medicare.
How long is a Medicare extended treatment notice valid?
A single notice for an extended course of treatment is only valid for 1 year. If the extended course of treatment continues after 1 year, issue a new notice.
When do you issue a reduction notice?
Reductions occur when a component of care decreases (for example, frequency or service duration). Do not issue the notice every time there is a reduction in care. If a reduction occurs and the beneficiary wants to continue getting care no longer considered medically reasonable and necessary, you must issue the notice before the beneficiary gets the noncovered care.
How long does it take for Medicare to refund a claim?
Medicare considers refunds timely within 30 days after you get the Remittance Advice from Medicare or within 15 days after a determination on an appeal if you or the beneficiary file an appeal.
Is an ABN valid for Medicare?
An ABN is valid if beneficiaries understand the meaning of the notice. Where an exception applies, beneficiaries have no financial liability to a non-contract supplier furnishing an item included in the Competitive Bidding Program unless they sign an ABN indicating Medicare will not pay for the item because they got it from a non-contract supplier and they agree to accept financial liability.
Does Medicare cover frequency limits?
Some Medicare-covered services have frequency limits. Medicare only pays for a certain quantity of a specific item or service in each period for a diagnosis. If you believe an item or service may exceed frequency limits, issue the notice before furnishing the item or service to the beneficiary.
What is it?
You'll get this notice each year if you have drug coverage from an employer/union or other group health plan. This notice will let you know whether or not your drug coverage is “creditable.”
What should I do if I get this notice?
Keep the notice. You may need it if you decide to join a Medicare drug plan later. (Don't send creditable coverage letters/certificates to Medicare.)
What is a CMS model notice?
CMS model notices contain all of the elements CMS requires for proper notification to enrollees or non-contract providers, if applicable. Plans may modify the model notices and submit them to the appropriate CMS regional office for review and approval. Plans may use these notices at their discretion.
Where can I find the Medicare Outpatient Observation Notice?
This form and its instructions can be accessed on the webpage " Medicare Outpatient Observation Notice (MOON)" at: /Medicare/Medicare-General-Information/BNI/MOON
What is a MOON in Medicare?
Medicare Outpatient Observation Notice (MOON) Hospitals and CAHs are required to provide a MOON to Medicare beneficiaries (including Medicare Advantage health plan enrollees) informing them that they are outpatients receiving observation services and are not inpatients of a hospital or critical access hospital (CAH).
How long does a hospital have to issue a notice to enrollees?
As under original Medicare, a hospital must issue to plan enrollees, within two days of admission, a notice describing their rights in an inpatient hospital setting, including the right to an expedited Quality Improvement Organization (QIO) review at their discharge. (In most cases, a hospital also issues a follow-up copy of this notice a day or two before discharge.) If an enrollee files an appeal, then the plan must deliver a detailed notice stating why services should end. The two notices used for this purpose are:
When does a plan issue a written notice?
A plan must issue a written notice to an enrollee, an enrollee's representative, or an enrollee's physician when it denies a request for payment or services. The notice used for this purpose is the:
What are the different types of notices?
The following model notices are available in both Microsoft Word and PDF formats in the "Downloads" section below: 1 Notice of Right to an Expedited Grievance 2 Waiver of Liability Statement 3 Notice of Appeal Status 4 Notice of Dismissal of Appeal
What is an advance notice for a nursing facility?
A provider must issue advance written notice to enrollees before termination of services in a Skilled Nursing Facility (SNF), Home Health Agency (HHA), or Comprehensive Outpatient Rehabilitation Facility (CORF). If an enrollee files an appeal, then the plan must deliver a detailed explanation of why services should end. The two notices used for this purpose are:
What is a CORF in Medicare?
Comprehensive outpatient rehabilitation facilities (CORFs) are settings in which a beneficiary may receive multidisciplinary rehabilitative services billed under Part B. [25] CORF services are eligible for Medicare payment only if the beneficiary could receive the same services if he or she were a hospital inpatient and if the CORF services are directly related to rehabilitation. [26] The new transmittal makes it clear that CORFs must issue an ABN if services are no longer medically necessary but the beneficiary wishes to continue treatment. [27]
What happens if a provider fails to issue an ABN?
If a provider fails to issue the ABN or uses an outdated version, the provider risks being held liable for the services or items in question. [12] ABNs inform Medicare beneficiaries in advance that a particular service will not be covered by Medicare. Beneficiaries can then decide whether to have the service or treatment and whether to appeal to Medicare to challenge the non-coverage.
What should advocates do as CMS refines ABN requirements?
As CMS continues to refine requirements of the ABN, advocates and providers should keep a close tab on the ensuing changes. Additionally, advocates should make sure that as CMS becomes more permissive in electronic ABN retention and notice, beneficiaries are appropriately informed of their rights .
Is an ambulance covered by Medicare?
Ambulance services are covered under Part B of the Medicare program if they are medically necessary. [22] Before shifting liability to a beneficiary for ambulance services that are not reasonably necessary, the provider must issue an ABN. [23] Delivery of an ANB during an emergency is inappropriate. The transmittal provides three clarifying questions for guidance as to when an ABN is mandatory. If the answer to all the following questions is "yes", an ABN must be issued: "Is this service a covered ambulance benefit; Will payment for part or all of this service be denied because it is not reasonable and necessary; and Is the patient stable and the transport non-emergent?" [24]
Does Medicare reimburse for prosthetics?
As Medicare's Durable Medical Equipment Prosthetics Orthotics and Supplies Competitive Bidding Program (DMEPOS) is rolled out in a given geographic area, providers and suppliers who are not certified under DMEPOS will not be reimbursed by Medicare for equipment provided to beneficiaries. [19] If such providers wish to serve Medicare beneficiaries, they must supply them with an ABN before the equipment is delivered to the beneficiary. [20] If the supplier complies with the ABN requirements and the beneficiary still wishes to receive the equipment, the supplier may ask to be paid by the beneficiary at its full payment rate. [21]
Can CMS retain ABNs?
CMS is moving toward electronic retention of documents. The manual now specifies that providers are permitted to retain electronic copies of signed ABNs. [30] Providers may also inform beneficiaries electronically about a service that will not be covered by Medicare. Electronic ABN's are valid only if the beneficiary can clearly see the screen. Providers must, nonetheless, supply the beneficiary with a hard copy of the ABN following signed acknowledgement. [31] Additionally, notices are no longer contained within the manual appendix. Instead, providers are directed to the CMS website, and are charged with the duty to check expiration dates and the CMS website for periodic updates. [32] Step-by-step instructions for notice can be found at www. cms. gov / BNI / Downloads / ABNFormInstructions. zip. [33]
