Full Answer
Can I submit a paper claim to Medicare?
Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. CMS has provided a listing of exceptions to electronic claim submission on its Administrative Simplification Compliance Act Self-Assessment Web page. Some of these include:
What is a Medicare Part B Medicare claims mailing address?
These companies process claims made on services covered by Medicare Part B like medical services, lab tests and imaging, vaccines and durable medical equipment. Your specific Medicare claims mailing address can be found on your Medicare Summary Notice (MSN).
How long does it take to process a Medicare Part B claim?
NOTE: Part B claims, including Medicare Secondary Payer (MSP) claims, are accepted and processed as electronic claims through myCGS, our secure web portal. Electronic claims can be paid in as few as 14 days, compared to 29 days for paper claims. Submitting claims through myCGS is FREE!
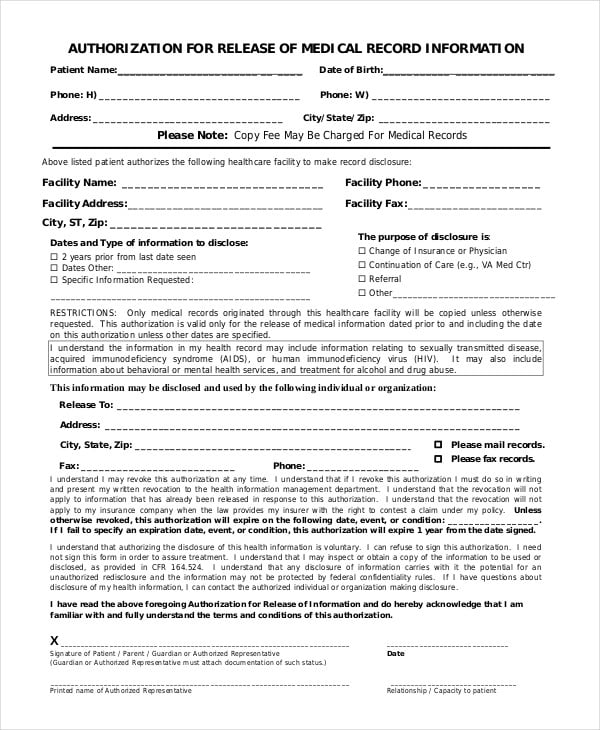
How do I fill out a Medicare claim form?
Provide your Medicare number, insurance policy number or the account number from your latest bill. Identify your claim: the type of service, date of service and bill amount. Ask when your claim will be processed and when you will find out how much has been paid by Medicare or your Medigap company or retiree plan. Identify yourself.
Does Medicare Part B accept paper claims?
Medicare Part B paper claims may be filed using only the red printed (08/05) claim form. This form is appropriate for filing all types of health insurance claims to private insurers as well as government programs.
Can you submit Medicare claims on paper?
The Administrative Simplification Compliance Act (ASCA) requires that as of October 16, 2003, all initial Medicare claims be submitted electronically, except in limited situations. Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. web page.
Where do I mail Medicare Part B claims?
Medicare Claims Mailing Addressed for Mental Health Part B ClaimsNoridian Healthcare Solutions.P.O. Box 6704 Fargo, ND 58108-6704.
How do providers submit claims to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Does Medicare accept handwritten claims?
Medicare to Reject Handwritten Claims. Providers who wish to continue to submit paper claims may do so as long as they are printed and as long as the only handwriting included in the claim is in a signature field. Software programs are available that will allow providers to print information into a CMS 1500 form.
Does Medicare accept secondary paper claims?
Currently, Medicare does not accept electronically filed claims when there is more than one payer primary to Medicare. Claims that involve more than one primary payer to Medicare must be submitted on the 1500 paper claim form, with all appropriate attachments.
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
What is the address for Medicare claims?
Medicare claim address, phone numbers, payor id – revised listStateAppeal addressArizonaAZMedicare Part B PO Box 6704 Fargo, ND 58108-6704MontanaMTMedicare Part B PO Box 6735 Fargo, ND 58108-6735North DakotaNDMedicare Part B PO Box 6706 Fargo, ND 58108-6706South DakotaSDMedicare Part B PO Box 6707 Fargo, ND 58108-670719 more rows
How do I submit Medicare secondary claims?
Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.
What is the difference between paper claims and electronic claims?
Paper claims that are almost obsolete are still used by certain payers. To send out paper claims, billers will have to enter claim details in the forms provided by insurance companies and send the completed details across. In contrast electronic claims are created and sent to clearinghouses/insurers via their EHRs.
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
How are Medicare claims processed?
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
What is Medicare contractor edit?
Medicare contractors perform a series of edits. The initial edits are to determine if the claims in a batch meet the basic requirements of the HIPAA standard. If errors are detected at this level, the entire batch of claims would be rejected for correction and resubmission.
Can a provider purchase software?
Providers can purchase software from a vendor, contract with a billing service or clearinghouse that will provide software or programming support, or use HIPAA compliant free billing software that is supplied by Medicare carriers, DMEMACs and A/B MACs.
How to file a claim with Medicare?
Follow these steps: Fill out the claim form provided by your insurance company (if required). Attach copies of the bills you are submitting for payment (if required). Attach copies of the MSN related to those bills.
How does Medicare receive claims?
Your Medigap (supplemental insurance) company or retiree plan receives claims for your services 1 of 3 ways: Directly from Medicare through electronic claims processing. This is done online. Directly from your provider, if he/she accepts Medicare assignment. This is done online, by fax or through the mail.
How much does Medicare pay for Part B?
If the provider accepts assignment (agrees to accept Medicare’s approved amount as full reimbursement), Medicare pays the Part B claim directly to him/her for 80% of the approved amount. You are responsible for the remaining 20% (this is your coinsurance ). If the provider does not accept assignment, he/she is required to submit your claim ...
What happens if a provider does not accept assignment?
If the provider does not accept assignment, he/she is required to submit your claim to Medicare, which then pays the Part B claim directly to you. You are responsible for paying the provider the full Medicare-approved amount, plus an excess charge . Note: A provider who treats Medicare patients but does not accept assignment cannot charge more ...
Does Medicare send a bill for MSN?
For more information, see Assignment for Original Fee-for-Service Medicare . Medicare will send you a Medicare Summary Notice (MSN) form each quarter. Previously known as the Explanation of Medicare Benefits, the MSN is not a bill. You should not send money to Medicare after receiving an MSN.
What is the requirement for Medicare claim submission?
Mandatory Claim Submission. Section 1848 (g) (4) of the Social Security Act requires that you submit claims for all your Medicare patients for services rendered. This requirement applies to all physicians and suppliers who provide covered services to Medicare beneficiaries. Providers may not charge patients for preparing or filing a Medicare claim.
What is a claim in Medicare?
Claim is for services initially paid by a third-party insurer who then files a Medicare claim to recoup what Medicare pays as primary insurer (for example, indirect payment provisions); Claim is for other unusual services, which are evaluated by MAC s on a case-by-case basis;
What is Medicare initial claim?
Initial claims are those claims submitted to a Medicare fee-for-service carrier, DME Medicare Administrative Contractor, or FI for the first time, including resubmitted previously rejected claims, claims with paper attachments, demand bills, claims where Medicare is secondary, and non-payment claims. Initial claims do not include adjustments or claim corrections submitted to FI s on previously submitted claims or appeal requests.
How long does Noridian hold a claim?
The payment floor (minimum amount of time, required by law, for which all Medicare carriers must hold payment) is 14 days for electronic claims, as opposed to 29 days for paper claims.
What is an OTAF claim?
Obligated to Accept as Payment in Full' (OTAF) Medicare Secondary Payer (MSP) claims when there is more than one primary payer. MSP claims for which there is more than one primary payer and more than one allowed amount.
How is EDI filed?
EDI claims are transmitted electronically via telephone lines, via a modem, to Noridian. EDI filing gives the provider control over the timeliness and accuracy of the claims entry by eliminating the need for mailroom processing and manual data entry by Noridian.
What is an assigned claim in Noridian?
Certain services, when rendered, may only be paid on an assigned basis: Clinical diagnostic laboratory services. Physician services to individuals dually entitled to Medicare and Medicaid.