Hospice
Hospice care is a type of care and philosophy of care that focuses on the palliation of a chronically ill, terminally ill or seriously ill patient's pain and symptoms, and attending to their emotional and spiritual needs. In Western society, the concept of hospice has been evolving in Europe since the 11…
How does Medicare reimburse hospitals?
Mar 23, 2020 · Part A covers the first 60 days of a hospital stay after the associated deductible and coinsurance payments have been made. Part A also includes coverage for skilled nursing facilities and hospice care. What Does it Mean for a Hospital to “Accept Assignment?” Medicare determines reimbursement based on whether or not a provider participates in Medicare …
How does Medicare calculate reimbursement?
Part A Medicare coverage is responsible for all inpatient care, which may include surgeries and their recovery, hospital stays due to illness or injury, certain tests and procedures, and more. As far as out-of-pocket costs, you will be responsible for paying your deductible, coinsurance payments if your hospital stay is beyond 60 days, and for any care that is not deemed …
Does Medicare pay all hospital costs?
Mar 26, 2022 · How Do Hospitals Get Reimbursed By Medicare? In a Prospective Payment System (PPS), Medicare payment is linked to predetermined, fixed amounts. In order to determine how much to pay for a certain service (in particular, diagnosis-related groups for inpatient hospital services) the classification is used.
How to submit a claim for Medicare reimbursement?
To get reimbursed in these cases, you’ll need to submit a reimbursement form. You can find a copy of the Patient’s Request for Medical Payment form to download, complete and mail in at the CMS website. You’ll also need to include an itemized bill from the health care provider. The itemized bill with a Medicare reimbursement claim must include:
How does Medicare Part A pay hospitals?
Inpatient hospitals (acute care): Medicare pays hospitals per beneficiary discharge, using the Inpatient Prospective Payment System. The base rate for each discharge corresponds to one of over 700 different categories of diagnoses—called Diagnosis Related Groups (DRGs)—that are further adjusted for patient severity.Mar 20, 2015
How does hospital reimbursement work?
Healthcare providers are paid by insurance or government payers through a system of reimbursement. After you receive a medical service, your provider sends a bill to whoever is responsible for covering your medical costs.Feb 27, 2020
Does Medicare Part A pay 100% of hospital?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
How is reimbursement determined?
Payers assess quality based on patient outcomes as well as a provider's ability to contain costs. Providers earn more healthcare reimbursement when they're able to provide high-quality, low-cost care as compared with peers and their own benchmark data.
What are the four main methods of reimbursement?
What are the Methods of Hospital Reimbursement?Discount from Billed Charges.Fee-for-Service.Value-Based Reimbursement.Bundled Payments.Shared Savings.Jun 29, 2017
Does Medicare cover hospitals?
Medicare generally covers 100% of your medical expenses if you are admitted as a public patient in a public hospital. As a public patient, you generally won't be able to choose your own doctor or choose the day that you are admitted to hospital.Jun 24, 2021
How Long Does Medicare pay for hospital stay?
90 daysMedicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.May 29, 2020
What is Medicare Part A deductible for 2021?
Medicare Part A Premiums/Deductibles The Medicare Part A inpatient hospital deductible that beneficiaries will pay when admitted to the hospital will be $1,484 in 2021, an increase of $76 from $1,408 in 2020.Nov 6, 2020
When a patient uses Medicare as their primary insurance company, is the hospital required to choose appropriate and accurate diagnoses that
When a patient uses Medicare as their primary insurance company, the hospital is required to choose appropriate and accurate diagnoses that apply to the patient so that they can bill for the associated care.
What is Medicare insurance?
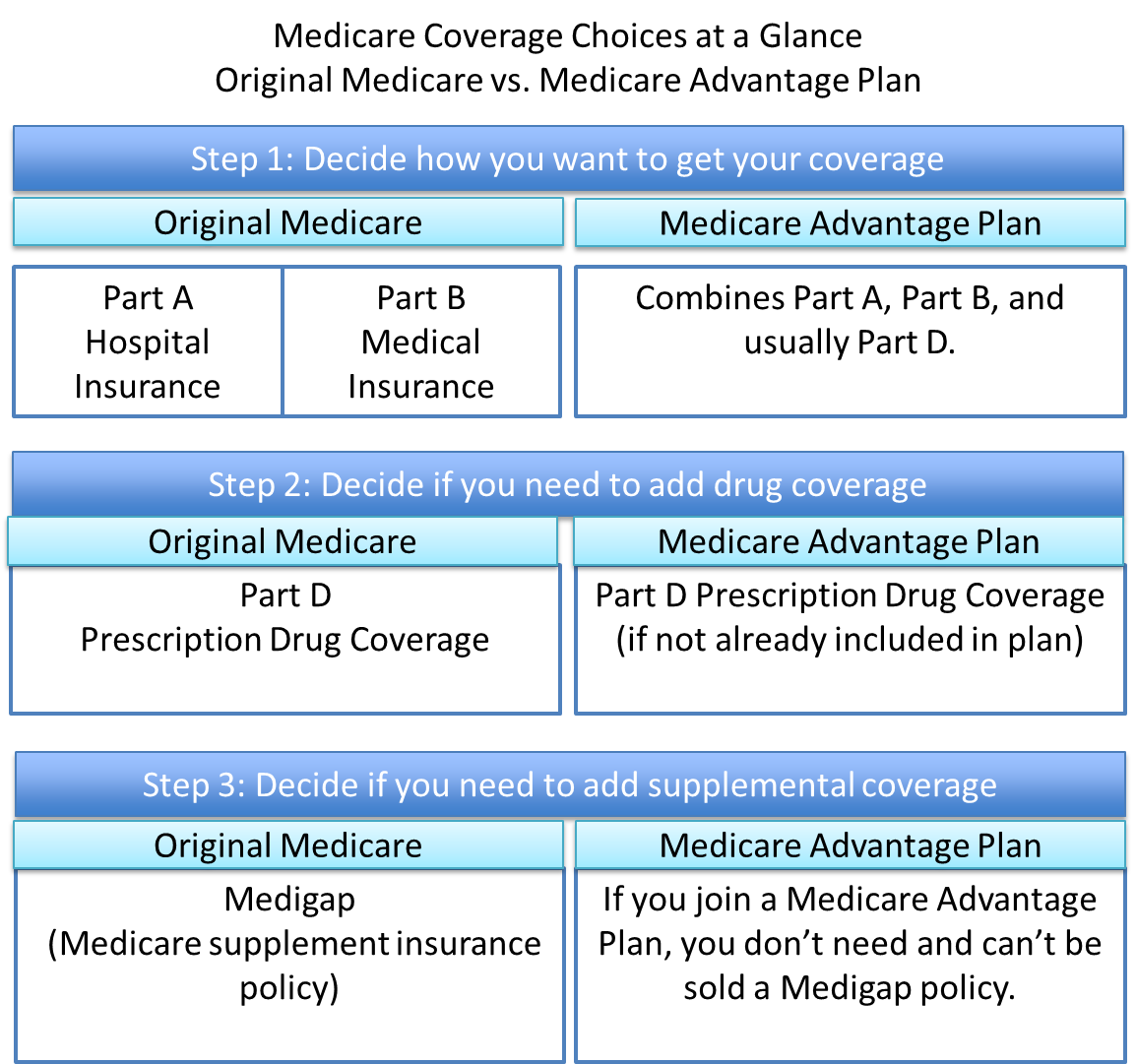
Medicare insurance is one of the most popular options for those who qualify, and the number of people using this insurance continues to grow as life expectancy continues to increase. Medicare policies come available with many different parts, including Part A, Part B, Part C, and Part D.
How long do you have to pay coinsurance for hospital?
As far as out-of-pocket costs, you will be responsible for paying your deductible, coinsurance payments if your hospital stay is beyond 60 days, and for any care that is not deemed medically necessary. However, the remainder of the costs will be covered by your Medicare plan.
Does Medicare pay flat rate?
This type of payment system is approved by the hospitals and allows Medicare to pay a simple flat rate depending on the specific medical issues a patient presents with and the care they require. In addition, In some cases, Medicare may provide increased or decreased payment to some hospitals based on a few factors.
Does Medicare cover inpatient care?
If you receive care as an inpatient in a hospital, Medicare Part A will help to provide coverage for care. Part A Medicare coverage is responsible for all inpatient care , which may include surgeries and their recovery, hospital stays due to illness or injury, certain tests and procedures, and more. As far as out-of-pocket costs, you will be ...
How Does Medicare Reimbursement Work?
If you are on Medicare, you usually don’t have to submit a claim when you receive medical services from a doctor, hospital or other health care provider so long as they are participating providers.
How to Get Reimbursed from Medicare
While most doctors simply bill Medicare directly, some other health care providers may require you to file for reimbursement from Medicare.
Reimbursement for Original Medicare
You won’t likely see a bill for services covered by Original Medicare. Participating providers will simply bill Medicare directly.
Medicare Advantage
You will never have to file a Medicare reimbursement claim if you have a Medicare Advantage plan. Medicare pays the private companies that manage Medicare Advantage plans to handle your claims for you.
Part D Prescription Drug Plan Reimbursement
Medicare Part D Prescription Drug plans are administered by private insurance companies. Generally, these companies handle any reimbursement process so you don’t have to worry about filing one.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
What happens if you see a doctor in your insurance network?
If you see a doctor in your plan’s network, your doctor will handle the claims process. Your doctor will only charge you for deductibles, copayments, or coinsurance. However, the situation is different if you see a doctor who is not in your plan’s network.
What to do if a pharmacist says a drug is not covered?
You may need to file a coverage determination request and seek reimbursement.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Do you have to pay for Medicare up front?
But in a few situations, you may have to pay for your care up-front and file a claim asking Medicare to reimburse you. The claims process is simple, but you will need an itemized receipt from your provider.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
Zipcode to Carrier Locality File
This file is primarily intended to map Zip Codes to CMS carriers and localities. This file will also map Zip Codes to their State. In addition, this file contains an urban, rural or a low density (qualified) area Zip Code indicator.
Provider Center
For a one-stop resource web page focused on the informational needs and interests of Medicare Fee-for-Service (FFS) providers, including physicians, other practitioners and suppliers, go to the Provider Center (see under "Related Links" below).
What is Medicare Bad Debt?
Medicare reimbursable bad debt can be a significant source of additional reimbursement for many hospitals.
Criteria for Allowable Bad Debts
The debt must be related to covered services and derived from deductible and coinsurance amounts.
What is Medicare Advantage Bad Debt?
Medicare Advantage bad debt seeks to reimburse hospitals for unpaid and uncollectable deductibles and coinsurance incurred by private Medicare Advantage Plan members enrolled with Medicare Part C carriers.
What is the Difference between Traditional Medicare Bad Debts and Medicare Advantage Bad Debts?
Traditional Medicare bad debts are those unpaid deductibles and coinsurance amounts that are related to Medicare Part A and Medicare Part B beneficiaries. These Part A and B bad debts are reported on the Medicare cost report each year and reimbursed as a lump sum to the hospital.
How does Healthcare Reimbursement Solutions (HRS) Assist Hospitals with Medicare Bad Debt and Medicare Advantage Bad Debt?
Healthcare Reimbursement Solutions (HRS) ensures your Medicare Bad Debt listings are complete, accurate, and created according to regulations outlined by CMS.
The Spend Down Program
Spend Down programs help the program participants to qualify for Medicaid coverage.
What Is Medicare Part B How Does It Relate To Hospital Beds
Medicare Part B is a standard part of the Original Medicare program which focuses on medical insurance. Medicare Part B covers services that focus on outpatient care, preventive care, and durable medical equipment.
You Can Add Home Care Equipment To A Hospital Bed
Hospital beds arent purely medical these days, they are luxurious, allowing for more comfortable recoveries, better sleep, and a more at-home feel.
Be Patient When Waiting
This is less of a tip on how to be approved and more advice on how to survive the waiting process. It can take weeks for this process to go from start to finish, frustrating some Medicaid patients and worrying others.
Will Medicare Cover Hospital Beds
If you or a loved one is struggling with the constraints of a traditional bed, there are innovative options that can make you safer and more comfortable at home.
How Are Hospital Beds Covered Under Medicare
A hospital bed is considered durable medical equipment that your doctor can prescribe for use in your own home.
Considering Height And Width
Most hospital beds weigh more and are wider than regular beds. Meanwhile, some can be adjusted to be higher or lower than regular beds.
What is Medicare reimbursement?
The Centers for Medicare and Medicaid (CMS) sets reimbursement rates for all medical services and equipment covered under Medicare. When a provider accepts assignment, they agree to accept Medicare-established fees. Providers cannot bill you for the difference between their normal rate and Medicare set fees.
How much does Medicare pay?
Medicare pays for 80 percent of your covered expenses. If you have original Medicare you are responsible for the remaining 20 percent by paying deductibles, copayments, and coinsurance. Some people buy supplementary insurance or Medigap through private insurance to help pay for some of the 20 percent.
What does it mean when a provider is not a participating provider?
If the provider is not a participating provider, that means they don’t accept assignment. They may accept Medicare patients, but they have not agreed to accept the set Medicare rate for services.
What is Medicare Part D?
Medicare Part D or prescription drug coverage is provided through private insurance plans. Each plan has its own set of rules on what drugs are covered. These rules or lists are called a formulary and what you pay is based on a tier system (generic, brand, specialty medications, etc.).
Is Medicare Advantage private or public?
Medicare Advantage or Part C works a bit differently since it is private insurance. In addition to Part A and Part B coverage, you can get extra coverage like dental, vision, prescription drugs, and more.
Do providers have to file a claim for Medicare?
They agree to accept CMS set rates for covered services. Providers will bill Medicare directly, and you don’t have to file a claim for reimbursement.
Can you bill Medicare for a difference?
Providers cannot bill you for the difference between their normal rate and Medicare set fees. The majority of Medicare payments are sent to providers of for Part A and Part B services. Keep in mind, you are still responsible for paying any copayments, coinsurance, and deductibles you owe as part of your plan.
