How is Medicare Advantage funded?
- Funding overview. There are two main sources of funding for Medicare Advantage. Advantage plans pay for the services...
- Bidding process. The Advantage plan bidding process involves two steps. First, each plan submits a bid to Medicare,...
- Base rate and risk adjustment rate. Medicare Advantage uses the bid and the benchmark to determine...
How much does Medicare pay Advantage plans?
Medicare Advantage plans have a cap on what the member must pay each year for health care services. Once the cap is met (anywhere from $3,500 to $6,000), the plan covers the remainder of the claims at 100%. Second, Medicare Advantage plans have set copayments for a variety of health care services such as office visits, labs, imaging, and ...
Why should I get a Medicare Advantage plan?
Things to know about Medicare Advantage Plans
- You're still in the Medicare Medicare is the federal health insurance program for: People who are 65 or older Certain younger people with disabilities People with End-Stage Renal Disease (permanent ...
- You still have Medicare rights and protections.
- You still get complete Part A and Part B coverage through the plan. ...
Who pays for Medicare Advantage plans?
Medicare Advantage plans expect a booming 2023, thanks in part to high projected revenue growth. But some Medicare watchers say the Centers for Medicare and Medicaid Services missed an opportunity to even out payments to the plans, which they say are ...
Why Advantage plans are bad?
disadvantage of medicare advantage plans
- Networks
- Referrals
- Prior Authorizations
- Frequent Expenses
- Out-of-Pocket Maximums
- Plan Changes
- Medicare is no longer managing your healthcare
What are the sources of revenue for Medicare Advantage plans?
Three sources of revenue for Advantage plans include general revenues, Medicare premiums, and payroll taxes. The government sets a pre-determined amount every year to private insurers for each Advantage member. These funds come from both the HI and the SMI trust funds.
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Is Medicare Advantage a private company?
If you have Original Medicare, the government pays for Medicare benefits when you get them. Medicare Advantage Plans, sometimes called “Part C” or “MA Plans,” are offered by private companies approved by Medicare. Medicare pays these companies to cover your Medicare benefits.
What is the biggest difference between Medicare and Medicare Advantage?
With Original Medicare, you can go to any doctor or facility that accepts Medicare. Medicare Advantage plans have fixed networks of doctors and hospitals. Your plan will have rules about whether or not you can get care outside your network. But with any plan, you'll pay more for care you get outside your network.
Can you switch back to Medicare from Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.
Who is behind Medicare Advantage?
UnitedHealthcare and Humana together account for 43 percent of all Medicare Advantage enrollees, and the BCBS affiliates (including Anthem BCBS plans) account for another 15 percent of in 2018. Another four firms (Aetna, Kaiser Permanente, Wellcare, and Cigna) account for another 21 percent of enrollment in 2018.
What is the difference between Medigap and Medicare Advantage?
Medigap is supplemental and helps to fill gaps by paying out-of-pocket costs associated with Original Medicare while Medicare Advantage plans stand in place of Original Medicare and generally provide additional coverage.
Is Medicare federally funded?
As a federal program, Medicare relies on the federal government for nearly all of its funding. Medicaid is a joint state and federal program that provides health care coverage to beneficiaries with very low incomes.
Is Medicare Advantage cheaper than original Medicare?
The costs of providing benefits to enrollees in private Medicare Advantage (MA) plans are slightly less, on average, than what traditional Medicare spends per beneficiary in the same county. However, MA plans that are able to keep their costs comparatively low are concentrated in a fairly small number of U.S. counties.
What is the most popular Medicare Advantage plan?
AARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.
What are the advantages and disadvantages of Medicare Advantage plans?
Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
Who pays for Medicare?
Medicare is funded through multiple sources: 46% comes from general federal revenue such as income taxes, 34% comes from Medicare payroll taxes and...
Is Medicare funded by the state or federal government?
Medicare is a federal program, and as a result, the vast majority of Medicare funding comes from the federal government. However, state governments...
What percentage of Medicare is paid by the federal government?
The federal government finances 99% of the Medicare budget, while the remaining 1% comes from states.
Are Medicare and Medicaid funded in the same way?
Medicare and Medicaid are two different programs, serving two disparate populations, and the programs are funded differently. As a federal program,...
How much does the government pay Medicare Advantage plans?
Medicare pays Medicare Advantage plans more than $1,000 a month for each beneficiary enrolled in their plan. Medicare spends more than $348 billion...
What is Medicare Advantage?
Medicare spending. Summary. Medicare Advantage, or Part C, is a health insurance program. It is funded from two different sources. The monthly premiums of beneficiaries provide part of the funding. However, the main source is a federal agency called the Centers for Medicare & Medicaid Services, which runs the Medicare program.
What percentage of Medicare is on Advantage plans?
In 2019, Medicare payments to Advantage plans to fund Part A and Part B benefits were $250 billion, according to the Kaiser Family Foundation. This represents 33% of Medicare’s total spending.
How does Medicare bidding work?
First, each plan submits a bid to Medicare, based on the estimated cost of Part A and Part B benefits per person. Next, Medicare compares the amount of the bid against the benchmark.
What determines the amount of Medicare payments?
The amount of the monthly payments depends on two main factors: the healthcare practices in the county where each beneficiary lives, which influences a procedure called the bidding process. the health of each beneficiary, which governs how Medicare raises or lowers the rates, in a system known as risk adjustment.
What happens if Medicare bid is lower than benchmark?
If the bid is lower than the benchmark, the plan gets a rebate from Medicare that is a percentage of the difference between the bid and the benchmark. Plans that receive rebates should use a portion of the rebates to fund supplemental benefits or to reduce premiums.
What is benchmark Medicare?
The benchmark is a percentage of costs of average Medicare spending per individual. Each county in the United States has its own benchmark. It reflects the practice patterns of resident healthcare providers that bill Medicare. Practice patterns differ among counties, so their benchmarks also differ.
What are the sources of Medicare funds?
Two trust funds held by the United States Department of the Treasury supply the money for Medicare payments. The funds are the Hospital Insurance Trust Fund and the Supplemental Medical Insurance Trust fund.
How many people did Medicare cover in 2017?
programs offered by each state. In 2017, Medicare covered over 58 million people. Total expenditures in 2017 were $705.9 billion. This money comes from the Medicare Trust Funds.
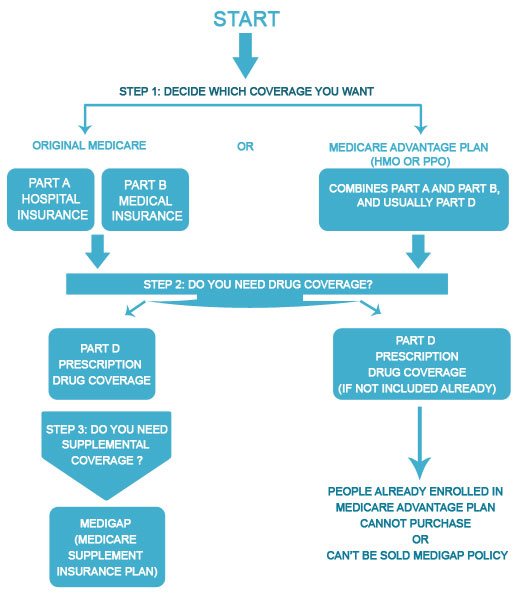
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. and. Medicare Drug Coverage (Part D) Optional benefits for prescription drugs available to all people with Medicare for an additional charge.
What is the CMS?
The Centers for Medicare & Medicaid Services ( CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the. Department Of Health And Human Services (Hhs) The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, ...
What is covered by Part A?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents.
Who pays payroll taxes?
Payroll taxes paid by most employees, employers, and people who are self-employed. Other sources, like these: Income taxes paid on Social Security benefits. Interest earned on the trust fund investments. Medicare Part A premiums from people who aren't eligible for premium-free Part A.
Does Medicare cover home health?
Medicare only covers home health care on a limited basis as ordered by your doctor. , and. hospice. A special way of caring for people who are terminally ill. Hospice care involves a team-oriented approach that addresses the medical, physical, social, emotional, and spiritual needs of the patient.
What is Medicare Advantage?
Medicare Advantage, a health plan provided by private insurance companies, is paid for by federal funding, subscriber premiums and co-payments. It includes the same coverage as the federal government’s Original Medicare program as well as additional supplemental benefits.
How is health insurance funded?
Treasury. The Hospital Insurance Trust Fund is funded by federal payroll taxes and income taxes from Social Security benefits.
What is Supplementary Medical Insurance Fund?
The Supplementary Medical Insurance Fund is composed of funds approved by Congress and Part B and Part D premiums paid by subscribers.
Is Medicare Advantage financed by monthly premiums?
Each insurance company is approved and contracted by Medicare and must fulfill guidelines for coverage as established by the government. Medicare Advantage plans are also financed by monthly premiums paid by subscribers. The premium amounts vary by company and plan.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).