Most Medicare-certified providers are required to submit an annual cost report to CMS The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…Centers for Medicare and Medicaid Services
Full Answer
How do I report a claim to Medicare?
Reporting is accomplished by either the submission of an electronic file of liability, no-fault, and workers’ compensation claim information, where the injured party is a Medicare beneficiary, or by entry of this claim information directly into a secure Web portal, depending on the volume of data to be submitted.
Where do I send inquiries about Medicare provider data?
Inquiries regarding this data can be sent to [email protected]. To receive email notifications, please sign up for the Medicare Provider Data GovDelivery subscription here.
What is included in a Medicare Cost Report?
Most Medicare-certified providers are required to submit an annual cost report to CMS. The cost report contains provider information such as facility characteristics, utilization data, cost and charges by cost center (in total and for Medicare), Medicare settlement data, and financial statement data.
How do I receive email notifications for Medicare provider data GovDelivery?
To receive email notifications, please sign up for the Medicare Provider Data GovDelivery subscription here.
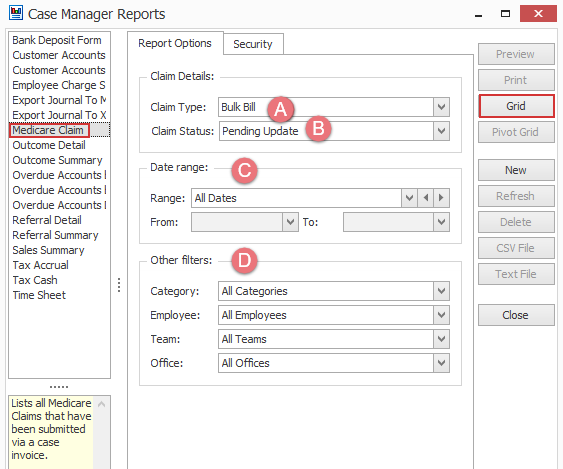
How do providers submit claims to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What is the reporting process of CMS?
Reporting is accomplished by either the submission of an electronic file of liability, no-fault, and workers' compensation claim information, where the injured party is a Medicare beneficiary, or by entry of this claim information directly into a secure Web portal, depending on the volume of data to be submitted.
How is Medicare data collected?
Abstraction of administrative/claims data. Medicare administrative data or Medicare Fee-for-Service claims (administrative) data, also known as health services utilization data, are collected by the Centers for Medicare and Medicaid Services (CMS) and derived from reimbursement information or the payment of bills.
How are Medicare claims processed?
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
What is Medicare Secondary Payer reporting?
As background, the MSP reporting requirements are intended to help the Centers for Medicare and Medicaid Services (CMS) determine whether a plan is primary to Medicare—that is, whether a plan pays first, and Medicare is a secondary payer.
What is MSP reporting?
The MSP Input File is used to report GHP coverage information for Active Covered Individuals who are Medicare beneficiaries. It assists the Benefits Coordination & Recovery Center (BCRC) in determining when Medicare should be paying secondary for a GHP covered individual.
What type of data does CMS collect?
The data held currently by CMS come from a variety of sources, of which the most important is claims for all types of services provided. All claims contain basic diagnostic information, as well as information on date of service, the type of service provided, and the identity of the prescribing physician.
What is included in CMS data?
CMS Main NavigationMedicare Provider Utilization and Payment Data.Medicare Provider Utilization and Payment Data: Physician and Other Practitioners. Medicare Provider Utilization and Payment Data: Inpatient. Medicare Provider Utilization and Payment Data: Outpatient.
What is administrative claims data?
Administrative claims data includes information necessary for reimbursement of medical services, which generally consists of diagnoses and procedures received during inpatient, outpatient, or emergency room visits, and dispensed prescription medications.
Who processes Medicare claims?
Medicare Administrative ContractorA Medicare Administrative Contractor (MAC) is a private health care insurer that has been awarded a geographic jurisdiction to process Medicare Part A and Part B (A/B) medical claims or Durable Medical Equipment (DME) claims for Medicare Fee-For-Service (FFS) beneficiaries.
How are claims processed?
How Does Claims Processing Work? After your visit, either your doctor sends a bill to your insurance company for any charges you didn't pay at the visit or you submit a claim for the services you received. A claims processor will check it for completeness, accuracy and whether the service is covered under your plan.
Can providers check Medicare claims online?
Providers can submit claim status inquiries via the Medicare Administrative Contractors' provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.
How to file an appeal with Medicare?
For questions about a specific service you got, look at your Medicare Summary Notice (MSN) or log into your secure Medicare account . You can file an appeal if you disagree with a coverage or payment decision made by one of these: 1 Medicare 2 Your Medicare health plan 3 Your Medicare drug plan
What is an improper care complaint?
Improper care or unsafe conditions. You may have a complaint about improper care (like claims of abuse to a nursing home resident) or unsafe conditions (like water damage or fire safety concerns).
What is POA indicator reporting?
POA indicator reporting is mandatory for all claims involving inpatient admissions to general acute care hospitals or other facilities. POA is defined as present at the time the order for inpatient admission occurs.
Does CMS require POA?
CMS does not require a POA Indicator for an external cause of injury code unless it is being reported as an "other diagnosis.". Issues related to inconsistent, missing, conflicting, or unclear documentation must be resolved by the provider.
Who must report a claim to Medicare?
Reporting a Case. Medicare beneficiaries, through their attorney or otherwise, must notify Medicare when a claim is made against an alleged tortfeasor with liability insurance (including self-insurance), no-fault insurance or against Workers’ Compensation (WC). This obligation is fulfilled by reporting the case in the Medicare Secondary Payor ...
When does Medicare focus on the date of last exposure?
When a case involves continued exposure to an environmental hazard, or continued ingestion of a particular substance, Medicare focuses on the date of last exposure or ingestion to determine whether the exposure or ingestion occurred on or after 12/5/1980.
How to get BCRC contact information?
Contact information for the BCRC may be obtained by clicking the Contacts link. When reporting a case in the MSPRP or contacting the BCRC, the following information is needed: Beneficiary Information: Once all information has been obtained, the BCRC will apply it to Medicare’s record.
Does Medicare cover non-ruptured implants?
For non-ruptured implanted medical devices, Medicare focuses on the date the implant was removed. (Note: The term “exposure” refers to the claimant’s actual physical exposure to the alleged environmental toxin, not the defendant’s legal exposure to liability.)
Does Medicare cover MSP?
Medicare has consistently applied the Medicare Secondary Payer (MSP) provision for liability insurance (including self-insurance) effective 12/5/1980. As a matter of policy, Medicare does not claim a MSP liability insurance based recovery claim against settlements, judgments, awards, or other payments, where the date of incident (DOI) ...
What is NGHP reporting?
Mandatory Insurer Reporting for Non-Group Health Plans (NGHP) Section 111 of the Medicare, Medicaid, and SCHIP Extension Act of 2007 (MMSEA) added mandatory reporting requirements with respect to Medicare beneficiaries who have coverage under group health plan (GHP) arrangements as well as for Medicare beneficiaries who receive settlements, ...
Who must report under Section 111?
Who Must Report. An organization that must report under Section 111 is referred to as a responsible reporting entity (RRE). In general terms, NGHP RREs include liability insurers, no-fault insurers, and workers’ compensation plans and insurers. RREs may also be organizations that are self-insured with respect to liability insurance, ...
60-Day Grace Period – Reporting Period 1
The September 30, 2021 Reporting Period 1 deadline has not changed, however in response to challenges providers are facing given the Covid surges and natural disasters around the country a 60-day Grace Period is in place.
Step 1: Register in the Provider Relief Fund Reporting Portal
The PRF Reporting Portal is open for recipients who received one or more payments exceeding, in the aggregate, $10,000 during Payment Received Period 1 (April 10, 2020 to June 30, 2020).
Step 2: Read the Reporting Requirements Notice
The Post-Payment Notice of Reporting Requirements updated on June 11, 2021 provides details on how to report on the use of funds. This supersedes all previous Notices of Reporting Requirements. Read the Reporting Requirements Notice (PDF - 232 KB) and reference the Reporting and Auditing Frequently Asked Questions.
Step 3: Complete and Submit Your Report
Complete and submit your report via the Provider Relief Fund Reporting Portal.
Important Dates for Reporting
Recipients who received one or more payments exceeding $10,000, in the aggregate, during a Payment Received Period are required to report in each applicable Reporting Time Period as outlined in the table below.
Need Help With Reporting?
We have detailed answers to common questions related to reporting requirements and auditing. Read the Frequently Asked Questions.
Partial Return of Funds
Once the report has been filed, the provider must return any unused funds to the government within 30 calendar days after the end of the applicable Reporting Time Period, as explained in the Terms and Conditions, and the Reporting Requirements Notice (PDF - 201 KB) (June 11, 2021).