Original Medicare includes Part A and Part B. Under this program, your Medicare providers send your claims directly to Medicare, and you wonât see a bill. Typically, you pay coinsurance or a copayment for Medicare Part A and Part B services, as well as Part A and Part B deductibles.
Full Answer
Will I have to pay for part an of Medicare?
Medicare Part A, which covers hospitalization, is free for anyone eligible for Social Security, even if they have not claimed benefits yet. If enrolled in Part B but not yet collecting Social Security benefits, you’ll be billed quarterly by Medicare.
What is the premium for Medicare Part A?
People who buy Part A will pay a premium of either $259 or $471 each month in 2021 depending on how long they or their spouse worked and paid Medicare taxes. If you choose NOT to buy Part A, you can still buy Part B.
How do I qualify for Medicare Part?
- Do you have, or are you eligible for, Part A?
- Is your income for 2021 at, or below, the income limits listed for any of the programs above?
- Do you have limited resources, below the limits above?
Do you have to pay for Medicare Part?
Most people get Part A for free, but some have to pay a premium for this coverage. To be eligible for premium-free Part A, an individual must be entitled to receive Medicare based on their own earnings or those of a spouse, parent, or child.

How does Medicare Part A get paid?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
How does Medicare Part A work?
Medicare is different from private insurance — it doesn't offer plans for couples or families. You don't have to make the same choice as your spouse. Part A covers inpatient hospital stays, skilled nursing facility care, hospice care, and some home health care.
Who pays Medicare Part A claims?
Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles).
What is billed to Medicare Part A?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
How does Medicare Part A deductible work?
Medicare Part A Deductible in 2022 Medicare Part A covers certain hospitalization costs, including inpatient care in a hospital, skilled nursing facility care, hospice and home health care. It does not cover long-term custodial care. For 2022, the Medicare Part A deductible is $1,556 for each benefit period.
Does Medicare Part A cover 100 percent?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
Does Medicare pay first or second?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Does Medicare automatically send claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.
What does Medicare pay as secondary payer?
As secondary payer, Medicare pays the lowest of the following amounts: (1) Excess of actual charge minus the primary payment: $175−120 = $55. (2) Amount Medicare would pay if the services were not covered by a primary payer: . 80 × $125 = $100.
Is Medicare paid monthly or quarterly?
All Medicare bills are due on the 25th of the month. In most cases, your premium is due the same month that you get the bill. Example of our billing timeline. For your payment to be on time, we must get your payment by the due date on your bill.
Why am I getting a bill for Medicare Part B?
If you have Medicare Part B but you are not receiving Social Security or Railroad Retirement Board benefits yet, you will get a bill called a “Notice of Medicare Premium Payment Due” (CMS-500). You will need to make arrangements to pay this bill every month.
How much is taken out of your Social Security check for Medicare?
In 2021, based on the average social security benefit of $1,514, a beneficiary paid around 9.8 percent of their income for the Part B premium. Next year, that figure will increase to 10.6 percent.
What is Medicare premium?
premium. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. for. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What does Part B cover?
In most cases, if you choose to buy Part A, you must also: Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Contact Social Security for more information about the Part A premium. Learn how and when you can sign up for Part A. Find out what Part A covers.
How much will Medicare premiums be in 2021?
People who buy Part A will pay a premium of either $259 or $471 each month in 2021 depending on how long they or their spouse worked and paid Medicare taxes. If you choose NOT to buy Part A, you can still buy Part B. In most cases, if you choose to buy Part A, you must also: Have. Medicare Part B (Medical Insurance)
What is premium free Part A?
Most people get premium-free Part A. You can get premium-free Part A at 65 if: The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents.
What is covered benefits and excluded services?
Covered benefits and excluded services are defined in the health insurance plan's coverage documents. from Social Security or the Railroad Retirement Board. You're eligible to get Social Security or Railroad benefits but haven't filed for them yet. You or your spouse had Medicare-covered government employment.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
What is Medicare Part A?
Medicare Part A, when combined with Medicare Part B (which covers outpatient insurance) is known as Original Medicare. Much of the care you receive through Medicare Part A is free, like home health services and hospice care.
How much does Medicare pay for a month?
If you’re getting retirement benefits or are eligible for retirement benefits, Medicare Part A has a $0 monthly premium payment. The same rule applies if you’re under 65 years old and have been claiming federal disability benefits for at least 24 months, or if you’ve been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis, or ALS). Americans who are eligible for Medicare, but not other federal benefits, can still get coverage for a monthly premium up to $471.
How much is Medicare coinsurance for 2021?
Days 61-90 : $352 coinsurance per day ($371 in 2021) Day 91 and beyond : $704 coinsurance per day for each "lifetime reserve day" after the benefit period ($742 in 2021) You get 60 “lifetime reserve days” while on Medicare. These are extra days you can apply toward your qualified stay.
When do you enroll in Medicare Part A?
If you’re on federal retirement benefits, you get automatically enrolled in Medicare Part A and Medicare Part B on the first day of the month you turn 65. Otherwise, you will need to sign up yourself during your initial enrollment period, which starts three months before you turn 65.
Does Medicare cover inpatient hospital?
Medicare Part A covers the cost of an inpatient hospital stay, but fees charged by a doctor or specialist physician will be covered by Part B. Medicare Part A does not cover the following at any hospital or facility: A private room, unless medically necessary. In-room television and phone services. Personal items.
Does Medicare cover home health care?
Medicare can cover the cost of home health care — like intermittent skilled nursing care or home health aides — in specific circumstances. Primarily, you must have recently had prior inpatient hospitalization and be homebound (unable to leave your home for medical reasons).
Does Medicare cover nursing home care?
Medicare will cover your stay at the nursing facilities after your qualifying hospital stay and if you have a legitimate medical condition. Medicare will not cover a nursing home stay if it is simply for personal care, like bathing and getting dressed (sometimes called custodial care).
How long does Medicare Part A last?
A benefit period begins when you enter the hospital and ends when you are out for 60 days in a row. One benefit period may include more than one hospitalization.
When does Medicare kick in?
Starting January 1 or whenever your plan year begins, you pay your health care costs up to the deductible amount. After that, your health plan kicks in to help pay the cost of your care for the rest of the plan year. The cycle starts over at the beginning of each new plan year. Medicare Part A deductibles are different.
How much is the Medicare deductible for 2021?
She is in the hospital over 60 days this time, so she must also pay a co-pay for 5 days. For 2021, the Part A deductible is $1,484 and the daily copay is $371. Item. Amount. First Stay. Medicare Part A deductible. $1,484.
How often is Medicare deductible charged?
Many homeowners and car insurance policies charge a deductible whenever you file a claim. A health insurance deductible is usually charged once for the plan year.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How long does it take to get a deductible back after a hospital stay?
If you go back into the hospital after 60 days, then a new benefit period starts, and the deductible happens again. You would be responsible for paying two deductibles in this case – one for each benefit period – even if you’re in the hospital both times for the same health problem.
How long does Medicare cover lifetime reserve days?
Part A Lifetime Reserve Days. Medicare Part A covers an unlimited number of benefit periods, and it helps pay for up to 90 days of care for each one. After 90 days, it’s possible to tap into lifetime reserve days. Lifetime reserve days are like a bank account of extra hospital days covered by Medicare.
How much does Medicare pay for diagnostic tests?
You pay 20% of the Medicare-approved amount of covered diagnostic non-laboratory tests done in your doctor’s oce or in an independent testing facility, and the Part B deductible applies. You pay a copayment for diagnostic non-laboratory tests done in a hospital outpatient setting.
How much does Medicare pay for insulin?
You pay 100% for insulin (unless used with an insulin pump, then you pay 20% of the Medicare-approved amount, and the Part B deductible applies). You pay 100% for syringes and needles, unless you have Part D.
How much insulin will Medicare pay for 2021?
Starting January 1, 2021, if you take insulin, you may be able to get Medicare drug coverage that offers savings on your insulin and pay no more than $35 for a 30-day supply. Visit Medicare.gov/plan-compare to find a plan that offers this savings in your area.
How long does Medicare cover knee replacement?
If you have knee replacement surgery, Medicare covers CPM devices for up to 21 days for use in your home.
How many sessions of kidney education are covered by Medicare?
Medicare covers up to 6 sessions of kidney disease education services if you have Stage IV chronic kidney disease that will usually require dialysis or a kidney transplant. Medicare covers this if your doctor or other health care provider refers you for the service, and when the service is given by a doctor, certain qualified non-doctor provider, or certain rural provider.
How long does Medicare cover psychiatric hospital?
If you’re in a psychiatric hospital (instead of a general hospital), Part A only pays for up to 190 days of inpatient psychiatric hospital services during your lifetime.Medicare doesn’t cover:
How to contact Medicare supplier?
You can also call 1-800-MEDICARE (1-800-633-4227) . TTY users can call 1-877-486-2048.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
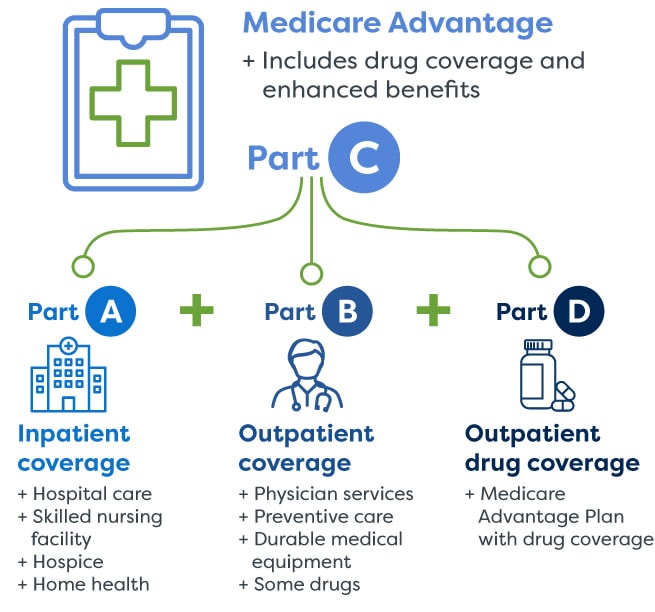
Medicare Advantage (Part C)
You pay for services as you get them. When you get a covered service, Medicare pays part of the cost and you pay your share.
You can add
You join a Medicare-approved plan from a private company that offers an alternative to Original Medicare for your health and drug coverage.
Most plans include
Some extra benefits (that Original Medicare doesn’t cover – like vision, hearing, and dental services)
Medicare drug coverage (Part D)
If you chose Original Medicare and want to add drug coverage, you can join a separate Medicare drug plan. Medicare drug coverage is optional. It’s available to everyone with Medicare.
Medicare Supplement Insurance (Medigap)
Medicare Supplement Insurance (Medigap) is extra insurance you can buy from a private company that helps pay your share of costs in Original Medicare.
What is Medicare Part B?
Medicare Part B. This is medical insurance and covers visits to doctors and specialists, as well as ambulance rides, vaccines, medical supplies, and other necessities.
How much is Medicare Part B 2021?
For Part B coverage, you’ll pay a premium each year. Most people will pay the standard premium amount. In 2021, the standard premium is $148.50. However, if you make more than the preset income limits, you’ll pay more for your premium.
What is the Medicare Part D premium for 2021?
Part D plans have their own separate premiums. The national base beneficiary premium amount for Medicare Part D in 2021 is $33.06, but costs vary. Your Part D Premium will depend on the plan you choose.
How does Social Security determine IRMAA?
The Social Security Administration (SSA) determines your IRMAA based on the gross income on your tax return. Medicare uses your tax return from 2 years ago. For example, when you apply for Medicare coverage for 2021, the IRS will provide Medicare with your income from your 2019 tax return. You may pay more depending on your income.
How many types of Medicare savings programs are there?
Medicare savings programs. There are four types of Medicare savings programs, which are discussed in more detail in the following sections. As of November 9, 2020, Medicare has not announced the new income and resource thresholds to qualify for the following Medicare savings programs.
How much do you need to make to qualify for SLMB?
If you make less than $1,296 a month and have less than $7,860 in resources, you can qualify for SLMB. Married couples need to make less than $1,744 and have less than $11,800 in resources to qualify. This program covers your Part B premiums.
Does Medicare change if you make a higher income?
If you make a higher income, you’ll pay more for your premiums, even though your Medicare benefits won’t change.
