How long do I have to join Medigap to switch plans?
Medigap policy to join a Medicare Advantage Plan but no later than 63 calendar days (or to switch to a Medicare SELECT policy) for the first time, you ve been in the plan less than a year, and you want to
How long do I have to wait to receive Medicare benefits?
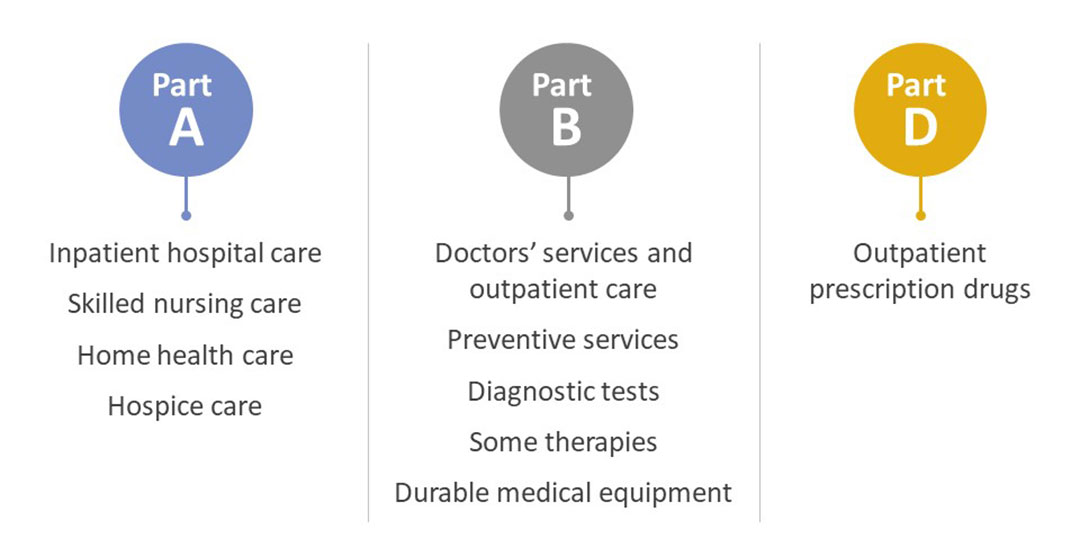
You may still have to wait up to 6 months before that benefit will be covered, no matter how long you've had your current Medigap policy. I'm moving out of state. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance).
When does my Medigap insurance start?
Generally, Medigap policies begin the first of the month after you apply. If, for any reason, the insurance company won't give you the effective date for the month you want, call your State Insurance Department. You paid for your policy, but it hasn't started If it's been 30 days and you didn't get your Medigap policy, call your insurance company.
What do you need to know about Medicare Medigap insurance?
You must have Medicare Part A and Part B. A Medigap policy is different from a Medicare Advantage Plan. Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. You pay the private insurance company a monthly

Can you add Medigap plans at any time?
Generally, there is no type of Medicare plan that you can get “any time.” All Medicare coverage, including Medicare Supplement (Medigap) plans, is subject to enrollment periods. Other types of Medicare plans, like Medicare Advantage and Medicare Part D prescription drug plans, have open enrollment periods every year.
Can you switch from Medicare Advantage to Medigap with pre-existing conditions?
The Medigap insurance company may be able to make you wait up to 6 months for coverage of pre-existing conditions. The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
Do Medicare Supplement plans have a waiting period?
What is the Medicare Supplement Waiting Period? For up to six months after your Medicare Supplement plan begins, your new plan can choose not to cover its portion of payments for preexisting conditions that were treated or diagnosed within six months of the start of the policy.
How long do I have to choose a Medigap plan?
A: If you already have Medigap insurance, you have 30 days of "open enrollment" following your birthday each year when you can buy a new Medigap policy without a medical screening or a new waiting period.
Can I be turned down for a Medigap policy?
In all but four states, insurance companies can deny private Medigap insurance policies to seniors after their initial enrollment in Medicare because of a pre-existing medical condition, such as diabetes or heart disease, except under limited, qualifying circumstances, a Kaiser Family Foundation analysis finds.
Can I switch from a Medicare Advantage plan to a Medigap plan?
Most Medicare Advantage Plans offer prescription drug coverage. , you may want to drop your Medigap policy. Your Medigap policy can't be used to pay your Medicare Advantage Plan copayments, deductibles, and premiums.
Can you switch from Medicare Advantage to Medigap without underwriting?
For example, when you get a Medicare Advantage plan as soon as you're eligible for Medicare, and you're still within the first 12 months of having it, you can switch to Medigap without underwriting.
Can you go back to Medicare Supplement after Medicare Advantage?
Once you've left your Medicare Advantage plan and enrolled in Original Medicare, you are generally eligible to apply for a Medicare Supplement insurance plan. Note, however, that in most cases, when you switch from Medicare Advantage to Original Medicare, you lose your “guaranteed-issue” rights for Medigap.
What is creditable coverage for Medigap?
For Medicare to consider a health plan to be creditable coverage, it must provide benefits at least as good as those Medicare provides. When a person has creditable coverage, they may delay enrollment in Medicare without accruing penalties.
Do most people get Medigap?
Among Medicare beneficiaries in traditional Medicare, most (83%) have supplemental coverage, either through Medigap (34%), employer-sponsored retiree health coverage (29%), or Medicaid (20%).
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
How do I pick a Medigap plan?
Follow the steps below to purchase your Medigap plan:Enroll in Medicare Part A and Part B. ... Find which insurance companies in your state are licensed to sell Medigap plans by visiting Medicare.gov.Compare costs between companies. ... Select a Medigap plan that works best for you and purchase your policy.
When to buy a Medigap policy
The best time to buy a Medigap Medicare Supplement Insurance (Medigap) An insurance policy you can buy to help lower your share of certain costs for Part A and Part B services (Original Medicare). policy is when you’re 65 (or older) and first get both Part A and Part B. You need both Part A and Part B to buy a Medigap policy.
How to buy a Medigap policy
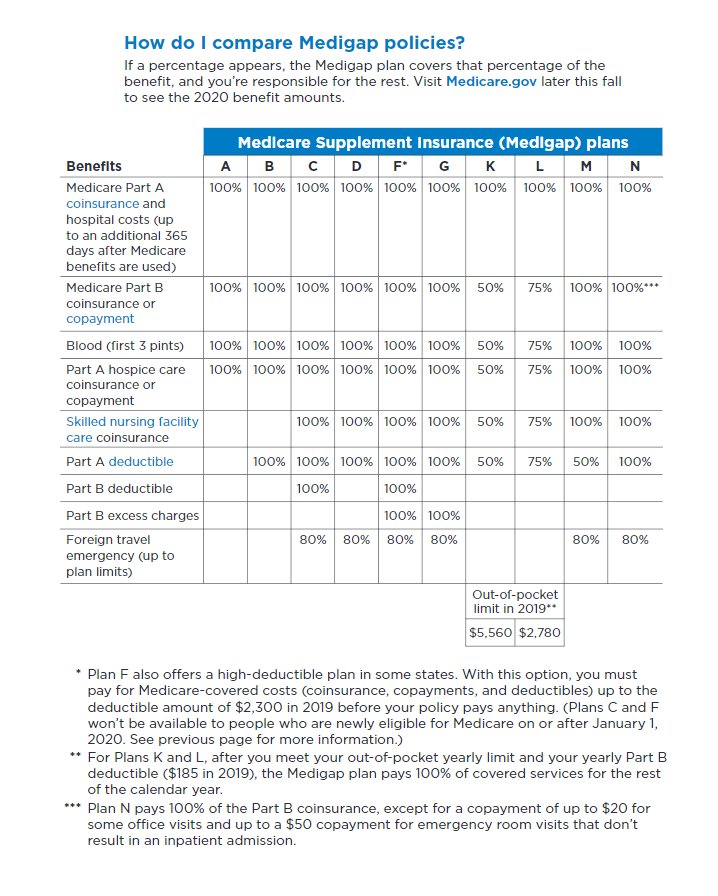
Medigap plans are standardized, and in most cases named by letters, like Plan G or Plan K.
When does Medigap coverage start?
Ask for your policy to become effective when you want coverage to start. Generally, Medigap policies begin the first of the month after you apply. If, for any reason, the insurance company won't give you the effective date for the month you want, call your State Insurance Department.
How long is the open enrollment period for Medigap?
Medigap Open Enrollment Period. A one-time only, 6-month period when federal law allows you to buy any Medigap policy you want that's sold in your state. It starts in the first month that you're covered under Part B and you're age 65 or older.
How to fill out a medical application?
Tips for filling out your application 1 Fill out the application carefully and completely, including medical questions. The answers you give will determine your eligibility for open enrollment or guaranteed issue rights (also called "Medigap protections"). 2 If your insurance agent fills out the application, check to make sure it's correct. 3 Remember that the insurance company can't ask you any questions about your family history or require you to take a genetic test. 4 If you buy a Medigap policy during your#N#Medigap Open Enrollment Period#N#A one-time only, 6-month period when federal law allows you to buy any Medigap policy you want that's sold in your state. It starts in the first month that you're covered under Part B and you're age 65 or older. During this period, you can't be denied a Medigap policy or charged more due to past or present health problems. Some states may have additional open enrollment rights under state law.#N#, the insurance company can’t use any medical answers you give to deny you a Medigap policy or change the price. 5 If you provide evidence that you're entitled to a guaranteed issue right, the insurance company can't use any medical answers you give to deny you a Medigap policy or change the price.
How to pay for insurance?
How to pay for your policy. It's best to pay by check, money order, or bank draft. Make it payable to the insurance company, not the agent. If buying from an agent, get a receipt with the insurance company's name, address, and phone number for your records. Some companies may offer electronic funds transfer.
Can you be denied a Medigap policy?
During this period, you can't be denied a Medigap policy or charged more due to past or present health problems. Some states may have additional open enrollment rights under state law. , the insurance company can’t use any medical answers you give to deny you a Medigap policy or change the price.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
Can you cancel a Medigap policy?
This means the insurance company can't cancel your Medigap policy as long as you pay the premium. Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
Step 1 – Decide which benefits you want, then decide which of the Medigap plans A–N meet your needs
Decide which benefits [glossary] you need and want while considering your current and future health care needs. You might not be able to switch policies later.
Step 4 – Buy the Medigap policy
Once you decide on the insurance company and the Medigap policy you want, you should apply. The insurance company must give you a clearly worded summary of your Medigap policy. Make sure you read it carefully. If you don't understand it, ask questions.
How long do you have to have a Medigap policy?
If you've had your Medicare SELECT policy for more than 6 months, you won't have to answer any medical questions.
How to switch Medigap insurance?
How to switch Medigap policies. Call the new insurance company and arrange to apply for your new Medigap policy. If your application is accepted, call your current insurance company, and ask for your coverage to end. The insurance company can tell you how to submit a request to end your coverage.
What happens if you buy a Medigap policy before 2010?
If you bought your policy before 2010, it may offer coverage that isn't available in a newer policy. If you bought your policy before 1992, your policy: Might not be a Guaranteed renewable policy. May have a bigger Premium increase than newer, standardized Medigap policies currently being sold. expand.
How long is the free look period for Medigap?
Medigap free-look period. You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period.". The 30- day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
Can you exclude pre-existing conditions from a new insurance policy?
The new insurance company can't exclude your Pre-existing condition. If you've had your Medigap policy less than 6 months: The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
Can I keep my Medigap policy if I move out of state?
I'm moving out of state. You can keep your current Medigap policy no matter where you live as long as you still have Original Medicare. If you want to switch to a different Medigap policy, you'll have to check with your current or new insurance company to see if they'll offer you a different policy. If you decide to switch, you may have ...
What is a Medigap policy?
Medigap policy with creditable drug coverage. Prescription drug coverage (for example, from an employer or union) that's expected to pay, on average, at least as much as Medicare's standard prescription drug coverage.
Can you get your Medicare coverage back if you have a Medigap policy?
If your Medigap policy covers prescription drugs, you'll need to tell your Medigap insurance company if you join a Medicare Prescription Drug Plan. The Medigap insurance company will remove the prescription drug coverage from your Medigap policy and adjust your premium. Once the drug coverage is removed, you can't get that coverage back, even though you didn't change Medigap policies.
Does Medigap have to send a notice?
Your Medigap company must send you a notice each year telling you if the prescription drug coverage in your Medigap policy is creditable. Keep these notices in case you decide later to join a Medicare drug plan.
Do you have to pay late enrollment penalty for Medigap?
You'll probably have to pay a late enrollment penalty if you have a Medigap policy that doesn't include creditable prescription drug coverage and you decide to join a Medicare Prescription Drug Plan later. This means you'll pay a higher monthly premium than if you joined when you were first eligible.
How long does it take to get approved for Medigap?
Medigap’s initial enrollment is a one-time 6-month application time period that guarantees that you will be approved for a Medigap. If you miss the initial enrollment window you will usually have to answer health questions and could be denied coverage.
When does Medigap start?
When your Medigap effective will begin: 3 months before your 65th birth month. The 1st of your 65th birth month. During your birth month. The 1st of the following month. During your 65th birth month. The 1st of the following month. During the 5 months after your 65th birth month. The 1st of the following month.
How long do you have to enroll in Medicare if you don't have Part B?
If you chose not to delay Medicare Part B, but have creditable coverage, when you leave that coverage you will have 63 days to enroll in a handful of Medigap plans.
What is Medicare Supplement?
Medicare Supplement, also known as Medigap, is supplemental insurance that fills in the gaps of Original Medicare. If you have decided that a Medigap policy is the right insurance for you, then you will want to sign up when you’re first eligible.
What is the number to call for Medigap?
We can help you choose a company that will work best for your health and financial needs, call our licensed independent insurance agents at 800-930-7956. *Notes:
What is the phone number for Medicare?
If you have an urgent matter or need enrollment assistance, call us at 800-930-7956. By submitting your question here, you agree that a licensed sales representative may respond to you about Medicare Advantage, Prescription Drug, and Medicare Supplement Insurance plans.
What happens if you miss your enrollment period?
If you miss your initial enrollment period you’ll usually have to go through medical underwriting unless you live in CT and NY or you qualify for a few special enrollment. Medical underwriting just means you’ll have to answer medical questions before you will be approved.