How Long Should You Keep Medicare Summary Notices?
- Medicare generally recommends that you keep notices for 1 to 3 years. It’s extremely unusual that Medicare would follow up on anything older than that. ...
- Tax purposes are generally a good index for document retention. In most cases, the IRS can’t audit you after 3 years have passed. ...
- For your own sake, do what you’re comfortable with. ...
How long should you keep Medicare EOB?
Dec 13, 2021 · Most experts recommend saving your Medicare summary notices for one to three years. At the very least, you should keep them while the medical services listed are in the process of payment by Medicare and supplemental insurance. How long should you keep medical statements? Medical Bills How long to keep: One to three years.
How long can you stay in a hospital with Medicare?
May 30, 2019 · Certainly, they need to be kept while the medical services that are summarized on the forms are in the process of payment by Medicare and supplemental insurance policies. After that, it is your call. One suggestion, storage space permitting, is to save medical payment records for three to six years as you would tax deduction records.
How long to keep Medicare statements after death?
Oct 26, 2021 · How Long Should I Keep Medicare Summary Notices Holding on to your MSNs for at least 12 months is a good rule of thumb. It allows you to …
How long do you need to keep Medicare statements?
How long should you keep Medicare summary notices? 1 to 3 years. What documents should you keep after someone dies? Copies of the following bills will be needed: Utility bills. Cell phone bills. Credit card bills. Mortgages and personal loans (including lines of credit) Real estate tax bills. Storage unit bills. Medical bills. Funeral bill.
Do I need to shred Medicare summary notices?
When the time comes to dispose of the hardcopy of your MSN's, treat this information as valuable personal information that needs to be protected. There are unscrupulous people who will steal your identity and use your Medicare information. Please shred your old MSN to protect your identity.Sep 30, 2012
Is there any reason to keep Medicare summary notices?
If you have a Medicare Supplement plan, your MSN will note that the claim was sent to the Medicare Supplement for processing. MSNs are helpful because they establish a record of your care, separate from billing purposes.
What is a Medicare Summary Notice?
It's a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services. The MSN shows: All your services or supplies that providers and suppliers billed to Medicare during the 3-month period. What Medicare paid. The maximum amount you may owe the provider.
Can I see my Medicare Summary Notice Online?
Log into (or create) your Medicare account. Select "Get your Medicare Summary Notices (MSNs) electronically" under the "My messages" section at the top of your account homepage.
Does Medicare send a year end statement?
A Medicare benefit tax statement is mailed each year between December and January. It shows Medicare Part A as qualifying healthcare coverage, meaning Part A meets the Affordable Care Act rules for health insurance.Aug 31, 2020
Can I go paperless with Medicare?
Medicare has been improving its paperless billing options, and you can now choose to receive your Medicare Summary Notices and the Medicare & You handbook electronically.
What is a valid Medicare statement?
A Medicare Summary Notice (MSN) is the statement that shows all the services or supplies billed to Medicare on your account, how much of the bill Medicare paid and how much you still owe the provider or supplier.
Does Medicare send out Explanation of Benefits?
Each month you fill a prescription, your Medicare Prescription Drug Plan mails you an "Explanation of Benefits" (EOB). This notice gives you a summary of your prescription drug claims and costs.
How do providers check Medicare claim status?
How do Medi-Cal providers check the status of a claim online?Click the Transactions tab on the Medi-Cal website home page.On the "Login To Medi-Cal" page, enter the user ID and password.Under the "Elig" tab, click the Automated Provider Service (PTN) link.Click the “Perform Claim Status Request” link.More items...•Feb 25, 2022
How do I get a copy of my Medicare statement?
If you have lost your MSN or you need a duplicate copy, call 1-800-MEDICARE or go to your account on www.mymedicare.gov.
How do I get my Medicare Part B statement?
You can ask the provider for an itemized statement for any service or claim. Call 1-800-MEDICARE (1-800-633-4227) for more information about a coverage or payment decision on this notice, including laws or policies used to make the decision.
How long does it take to get Medicare Part B after?
Most Medicare provider number applications are taking up to 12 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health. We assess your application to see if you're eligible to access Medicare benefits.Dec 10, 2021
How long do you keep Medicare records?
Medicare generally recommends that you keep notices for 1 to 3 years. It’s extremely unusual that Medicare would follow up on anything older than that. In any case, Medicare ought to have copies of your records. Tax purposes are generally a good index for document retention.
What is an MSN bill?
The many dollar signs on a Medicare Summary Notice (MSN) might stand out to you – but there’s no need to panic or reach for your checkbook. Medicare Summary Notices are not bills. An MSN gives a detailed list of services you’ve already received. It’s Medicare’s equivalent of the explanation of benefits ...
Why is MSN important?
MSNs are helpful because they establish a record of your care, separate from billing purposes.
What is Medicare Summary Notice?
The Medicare Summary Notice is a report of health care services over 3 months’ time. It’s just a statement of services and items. The eMSNs allow you to follow up with statements electronically and in a timely fashion. In the research below, you’ll learn more about the MSN and what do with it.
How often do you get a summary notice from Medicare?
What is a Medicare Summary Notice? Medicare beneficiaries get an MSN after a service or procedure. MSNs are sent via U.S.P.S. every 3 months. Further, MSNs explain the supplies and services you get, how much Medicare covers, and how much you must pay the doctor. An MSN is not a bill.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
How long does it take to appeal a Medicare claim?
Appeals must be made within 120 days of getting the MSN. Appeal information will be on the notice. Beneficiaries may read Your Medicare Rights and Protections online or call 1-800-MEDICARE to have a paper copy.
How to save a copy of a document on a computer?
The document will now open. Users should save a copy to their computer by clicking “File” and then “ Save a Copy” – from the top menu. Clicking the printer icon or navigate to file and then print allows users to print the document for their safekeeping.
What Is It?
- It's not a bill. It’s a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services. The MSN shows: 1. All your services or supplies that providers and suppliers billed to Medicare during the 3-month period 2. What Medicare paid 3. The maximum amount you may owe the provider
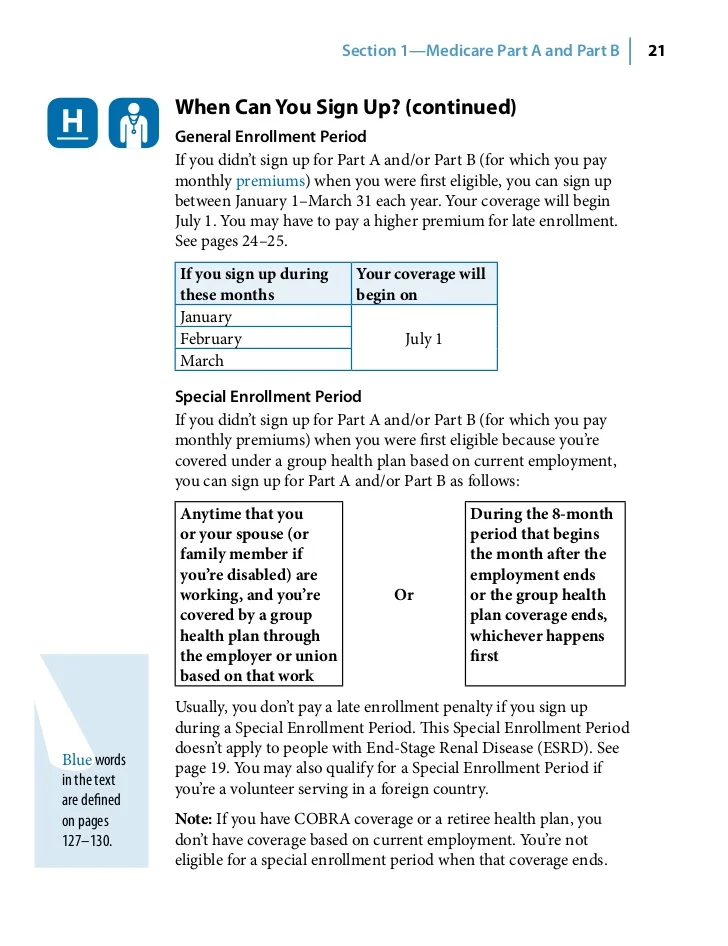
When Should I Get It?
- You’ll get your MSN every 3 months if you get any services or medical supplies during that 3-month period. If you don’t get any services or medical supplies during that 3-month period you won’t get an MSN for that particular 3-month period. If I need to change my address: Contact Social Security. If you get RRB benefits, contact the RRB.
Who Sends It?
- Medicare If you're not sure if your MSN is from Medicare, look for these things on the MSN envelope. [PDF, 380 KB]
What Should I Do If I Get This Notice?
- If you have other insurance, check to see if it covers anything that Medicare didn’t.
- Keep your receipts and bills, and compare them to your MSN to be sure you got all the services, supplies, or equipment listed.
- If you paid a bill before you got your notice, compare your MSN with the bill to make sure you paid the right amount for your services.
- If you have other insurance, check to see if it covers anything that Medicare didn’t.
- Keep your receipts and bills, and compare them to your MSN to be sure you got all the services, supplies, or equipment listed.
- If you paid a bill before you got your notice, compare your MSN with the bill to make sure you paid the right amount for your services.
- If an item or service is denied, call your doctor’s or other health care provider's office to make sure they submitted the correct information. If not, the office may resubmit. If you disagree with...