Full Answer
Does Medicare require you to rent or buy durable medical equipment?
Renting and buying DME Depending on the type of durable medical equipment (DME) you need, Medicare may require that you either rent or buy it. Most equipment is initially rented, including many manual and power wheelchairs. Original Medicare covers 80% of the cost of a monthly rental fee for 13 months.
Does Medicare cover durable medical equipment (DME)?
Durable medical equipment (DME) coverage. Medicare Part B (Medical Insurance) covers Medically necessary DME if your doctor prescribes it for use in your home. DME that Medicare covers includes, but isn't limited to: Blood sugar meters. Blood sugar test strips.
Does Medicare pay for home health care equipment?
Medicare Part B (Medical Insurance) covers the cost of. Medically necessary. durable medical equipment (DME) if your doctor prescribes it for use in your home. Medicare DME coverage includes, but isn't limited to: Blood sugar monitors. Blood sugar test strips. Canes.
What does Medicare Part B cover for medical equipment?
Medicare Part B (Medical Insurance) covers medically necessary durable medical equipment (DME) that your doctor prescribes for use in your home. Only your doctor can prescribe medical equipment for you.

How long is an order good for Medicare?
To ensure that an item is still medically necessary, the delivery date/date of service must be within 3 months from the "Initial Date" of the CMN or DIF or 3 months from the date of the physician's signature. The DME MACs and UPICs have the authority to request to verify the information on a CMN or DIF at any time.
Does Medicare pay for used equipment?
It includes a variety of items, such as walkers, wheelchairs, and oxygen tanks. Medicare usually covers DME if the equipment: Is durable, meaning it is able to withstand repeated use.
Does Medicare have a warranty?
Owning DME: If you purchased your equipment or otherwise own it, Medicare covers needed repairs and maintenance when a professional is required and the services are not covered by a warranty.
Does Medicare have to be paid back?
The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later. You're responsible for making sure Medicare gets repaid from the settlement, judgment, award, or other payment.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
How often does Medicare pay for DME?
Note: The equipment you buy may be replaced if it's lost, stolen, damaged beyond repair, or used for more than the reasonable useful lifetime of the equipment, which is generally 5 years from the date you start using the item. If you rent DME and other devices, Medicare makes monthly payments for use of the equipment.
Does Medicare pay for CPAP machine repairs?
After the trial period, Medicare may continue to cover longer CPAP therapy if you meet with your doctor in person, and your doctor documents in your medical record that you meet certain conditions and the therapy is helping you.
What is meant by durable medical equipment?
Equipment and supplies ordered by a health care provider for everyday or extended use. Coverage for DME may include: oxygen equipment, wheelchairs, crutches or blood testing strips for diabetics.
Does Medicare pay for walkers and shower chairs?
Q: Will Medicare cover the cost of wheelchairs and walkers? A: Yes. Medicare Part B covers a portion of the cost for medically-necessary wheelchairs, walkers and other in-home medical equipment.
How far back can Medicare recoup payments?
(1) Medicare contractors can begin recoupment no earlier than 41 days from the date of the initial overpayment demand but shall cease recoupment of the overpayment in question, upon receipt of a timely and valid request for a redetermination of an overpayment.
How do you qualify to get $144 back on your Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
Who is the largest Medicare Advantage provider?
AARP/UnitedHealthcareAARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.
What is assignment in Medicare?
Assignment —An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare pay for DME repairs?
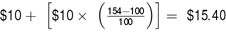
Medicare will pay 80% of the Medicare-approved amount (up to the cost of replacing the item) for repairs. You pay the other 20%. Your costs may be higher if the supplier doesn’t accept assignment.
How long does Medicare Advantage last?
Takeaway. Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of the facility for at least 60 days.
How long does Medicare benefit last after discharge?
Then, when you haven’t been in the hospital or a skilled nursing facility for at least 60 days after being discharged, the benefit period ends. Keep reading to learn more about Medicare benefit periods and how they affect the amount you’ll pay for inpatient care. Share on Pinterest.
How much coinsurance do you pay for inpatient care?
Days 1 through 60. For the first 60 days that you’re an inpatient, you’ll pay $0 coinsurance during this benefit period. Days 61 through 90. During this period, you’ll pay a $371 daily coinsurance cost for your care. Day 91 and up. After 90 days, you’ll start to use your lifetime reserve days.
What facilities does Medicare Part A cover?
Some of the facilities that Medicare Part A benefits apply to include: hospital. acute care or inpatient rehabilitation facility. skilled nursing facility. hospice. If you have Medicare Advantage (Part C) instead of original Medicare, your benefit periods may differ from those in Medicare Part A.
What is Medicare benefit period?
Medicare benefit periods mostly pertain to Part A , which is the part of original Medicare that covers hospital and skilled nursing facility care. Medicare defines benefit periods to help you identify your portion of the costs. This amount is based on the length of your stay.
Why is it important to check deductibles each year?
It’s important to check each year to see if the deductible and copayments have changed, so you can know what to expect. According to a 2019 retrospective study. Trusted Source. , benefit periods are meant to reduce excessive or unnecessarily long stays in a hospital or healthcare facility.
How much is Medicare deductible for 2021?
Here’s what you’ll pay in 2021: Initial deductible. Your deductible during each benefit period is $1,484. After you pay this amount, Medicare starts covering the costs. Days 1 through 60.
How many levels of DME coverage does Medicare have?
It is best to think of Medicare’s durable medical equipment coverage as having 2 levels. DME that is covered when determined to be medically necessary, and DME that is never covered despite being medically necessary.
What is Medicare Participating Supplier?
Medicare Participating Suppliers are suppliers that have agreed to accept “assignment”. Assignment is the Medicare approved price for a specific item of DME. Purchasing from a Medicare Participating Supplier ensures the individual will not pay more than the 20% co-pay of the Medicare approved price for an item.
What is Medicare Part D?
Medicare Part D is for prescription drugs and is not relevant to the discussion of DME. Part A covers medical equipment for individuals who are in a skilled nursing facility or in the hospital.
Does Medicare pay for a walker?
For example, Medicare may approve the purchase of a walker, but not one with wheels and a hand brake; this would be considered “upgraded equipment”. It is possible that an upgrade is medically necessary, and if so, Medicare will pay for its part of the upgrade cost.
Does Medicare cover grab bar rails?
For example, grab bar rails may be completely necessary for an individual, but Medicare does not consider them to be medical equipment and therefore, will not cover the cost. Durable Medical Equipment vs. Home Care Supplies. Commonly, persons cannot make the distinction between medical equipment and home care supplies.
Can you make the distinction between medical supplies and home care supplies?
Commonly, persons cannot make the distinction between medical equipment and home care supplies. Medicare has a completely different policy for home and/or disposable medical supplies as opposed to durable, multiple use equipment. Read more. Read more.
Does Medicare approve durable medical equipment?
Typically, when Medicare approves an item of durable medical equipment, they will approve only the most basic item available.
What is Medicare Advantage Part C?
Some Medicare Advantage Plans (Part C) offer extra benefits that Original Medicare doesn’t cover - like vision, hearing, or dental. Contact the plan for more information. Return to search results.
What does Medicare Part B cover?
Supplies. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. usually doesn’t cover common medical supplies, like bandages and gauze, which you use at home.
How long does Medicare pay for a wheelchair?
Most equipment is initially rented, including many manual and power wheelchairs. Original Medicare covers 80% of the cost of a monthly rental fee for 13 months. You pay a 20% coinsurance. After 13 months, ownership is typically given to you automatically.
Does Medicare pay for oxygen equipment?
Note: There are different rules for oxygen equipment. If you have Original Medicare, you will typically pay the least if you order your DME from a Medicare-approved supplier who takes assignment . If you have a Medicare Advantage Plan, make sure to follow your plan’s coverage rules.
What does it mean when a company sells medical equipment?
When a company that sells medical equipment is a Medicare supplier, they’ve agreed to charge Medicare-approved prices for an item. This means if you are purchasing a cane from a certain medical supplier, the price should be similar to that of other suppliers. Some suppliers will bill Medicare directly for you.
How long does a durable medical device last?
Medically needed. Not useful to a person who isn’t injured or has a chronic medical condition. Will usually last at least three years. Medicare Part B (the part that pays for doctor’s visits) pays for DME.
What is Medicare Advantage?
Medicare Advantage plans are when you choose a private insurance company to fulfill your Medicare benefits. Medicare requires all Medicare Advantage plans to cover DME at the same level as Original Medicare plans. However, the specific costs and suppliers may depend on your plan.
What is covered by Medicare Part B?
If you have Medicare Part B, your plan covers certain medically necessary durable medical equipment 1 Medicare will pay for a portion of durable medical equipment (DME), including wheelchairs, canes and hospital beds. 2 Medicare defines what qualifies as DME, including items used repeatedly, needed for a medical reason, and will usually last at least three years. 3 You’ll usually need a doctor’s “prescription” and must purchase the items from a Medicare-approved supplier to get reimbursement. 4 Medicare will typically pay 80 percent for renting or purchasing DME, and you’ll pay the remaining 20 percent.
How to get DME approved by Medicare?
You can get Medicare-approved DME in several ways: from your doctor, in-person at a supplier, or online. First, your doctor may supply it, such as a k nee or ankle brace they keep on-site. Second, your doctor may give you a list of Medicare suppliers in your area. Third, you can obtain a list of Medicare-approved suppliers from Medicare’s website . ...
What is DME in Medicare?
What is DME Medicare? Durable medical equipment or DME is the equipment you need to use in your home to support your health and keep you safe. Examples of DME include walkers, oxygen, blood sugar monitors, patient lifts, sleep apnea devices, and more. Medicare has a long list of DME it will cover, but you have to go through a Medicare-approved ...
How long does a DME last?
Medicare defines what qualifies as DME, including items used repeatedly, needed for a medical reason, and will usually last at least three years. You’ll usually need a doctor’s “prescription” and must purchase the items from a Medicare-approved supplier to get reimbursement.
What is the eligibility for a maintenance therapist?
To be eligible, either: 1) your condition must be expected to improve in a reasonable and generally predictable period of time, or 2) you need a skilled therapist to safely and effectively make a maintenance program for your condition , or 3) you need a skilled therapist to safely and effectively do maintenance therapy for your condition. ...
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
When does the SNF benefit period end?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. You must pay the inpatient hospital deductible for each benefit period.
What is a benefit period?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF.
How many days do you have to stay in a hospital to qualify for SNF?
Time that you spend in a hospital as an outpatient before you're admitted doesn't count toward the 3 inpatient days you need to have a qualifying hospital stay for SNF benefit purposes. Observation services aren't covered as part of the inpatient stay.
What services does Medicare cover?
Medicare-covered services include, but aren't limited to: Semi-private room (a room you share with other patients) Meals. Skilled nursing care. Physical therapy (if needed to meet your health goal) Occupational therapy (if needed to meet your health goal)
How long do you have to be in the hospital to get SNF?
You must enter the SNF within a short time (generally 30 days) of leaving the hospital and require skilled services related to your hospital stay. After you leave the SNF, if you re-enter the same or another SNF within 30 days, you don't need another 3-day qualifying hospital stay to get additional SNF benefits.
Can you get SNF care without a hospital stay?
If you’re not able to be in your home during the COVID-19 pandemic or are otherwise affected by the pandemic, you can get SNF care without a qualifying hospital stay. Your doctor has decided that you need daily skilled care. It must be given by, or under the supervision of, skilled nursing or therapy staff. You get these skilled services in ...