What is the timely filing for Medicare?
Claims processing by Medicare is quick and can be as little as 14 days if the claim is submitted electronically and it’s clean. In general, you can expect to have your claim processed within 30 calendar days. However, there are some exceptions, such as …
What is the timely filing limit for medical claims?
Feb 16, 2022 · A Medicare claim filed electronically could take up to 24 hours to be processed. An average receipt has 14 days to date. According to a healthcare plan the most effective methods are given a treatment claims that are submitted on behalf of a patient, and coverage of the services is denied. If a claim is submitted on behalf of the patient, and coverage of the services …
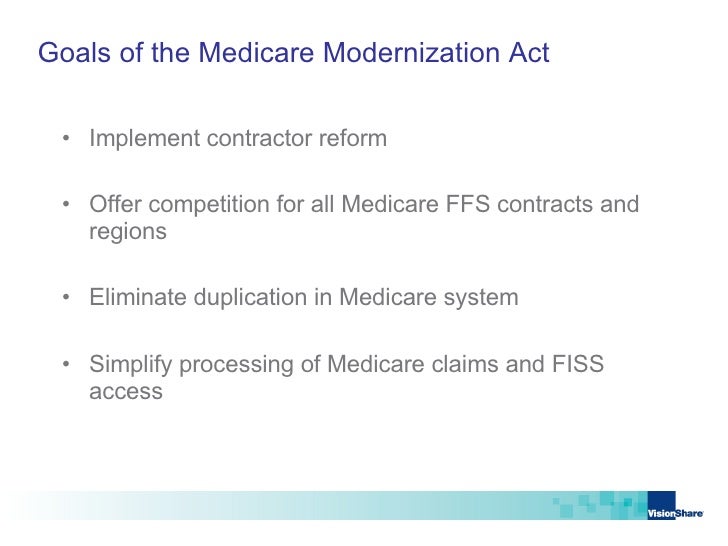
Which processes traditional Medicare claims?
Feb 16, 2022 · It typically takes 30 days for Medicare to process a claim. The government pays Part A claims to the providers directly (such as hospital stay, skilled nursing facility care, long-term care facility and home health care), rather than through a private insurance provider.
How are Medicare claims processed?
The healthcare provider submits Medicare Part A and B claims directly to Medicare. Each claim is then processed and settled by Medicare, which takes about 30 days. The process will take much longer if there are any questions or problems with the argument.
How long does a Medicare claim take?
12 monthsMedicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
How are Medicare claims processed?
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.Sep 1, 2016
How long does Medicare have to pay a clean claim?
Suppliers who file paper claims will not be paid before the 29 day after the date of receipt of their claims, i.e., a 28-day payment floor. However, clean claims filed electronically can be paid as early as 14 days after receipt, i.e., a 13-day payment floor.Oct 16, 2018
How long does it take to process a Medicare claim Australia?
7 daysIt can take us up to 7 days to process your claim. When you've submitted your claim, you can select: Download claim summary to view a PDF of the claim you just made. Make another claim.Dec 10, 2021
How are claims processed?
How Does Claims Processing Work? After your visit, either your doctor sends a bill to your insurance company for any charges you didn't pay at the visit or you submit a claim for the services you received. A claims processor will check it for completeness, accuracy and whether the service is covered under your plan.Apr 13, 2018
Can claims be mailed to Medicare?
The Administrative Simplification Compliance Act (ASCA) requires that Medicare claims be sent electronically unless certain exceptions are met. Providers meeting an ASCA exception may send their claims to Medicare on a paper claim form.Jan 1, 2022
How long does it typically take to receive payment with a clean claim?
These laws typically require the company to pay within 30 days of receiving a “clean claim” that contains all of the information that the payer needs to process the claim.
Why does Medicare deny claims?
If the claim is denied because the medical service/procedure was “not medically necessary,” there were “too many or too frequent” services or treatments, or due to a local coverage determination, the beneficiary/caregiver may want to file an appeal of the denial decision. Appeal the denial of payment.
How does Medicare reimbursement work?
Medicare reimbursement is the process by which a doctor or health facility receives funds for providing medical services to a Medicare beneficiary. However, Medicare enrollees may also need to file claims for reimbursement if they receive care from a provider that does not accept assignment.Dec 9, 2021
How long does Medicare card take to come?
If you're the only person listed on the Medicare card, you'll be the contact person for the card. We'll send your card in 3 to 4 weeks. You can use a digital copy of your Medicare card as soon as you enrol. You'll need to sign into the Express Plus Medicare mobile app to use it.Feb 24, 2022
How do I check my Medicare claim status Australia?
If you already have a Medicare online account, sign in through myGov. If you don't have a myGov account or a Medicare online account, you'll need to set them up. You can use your Medicare online account to manage details and claims, access statements and get letters online.Dec 20, 2021
How long does it take Centrelink to assess a claim?
The time it takes us to assess your claim doesn't affect your waiting period. You can expect to hear from us within 21 days of submitting your claim. It's best to submit your claim as soon as possible after your circumstances change or you stop getting another payment from us.Feb 8, 2022
How much does Medicare pay for Part B?
If the provider accepts assignment (agrees to accept Medicare’s approved amount as full reimbursement), Medicare pays the Part B claim directly to him/her for 80% of the approved amount. You are responsible for the remaining 20% (this is your coinsurance ). If the provider does not accept assignment, he/she is required to submit your claim ...
What happens if a provider does not accept assignment?
If the provider does not accept assignment, he/she is required to submit your claim to Medicare, which then pays the Part B claim directly to you. You are responsible for paying the provider the full Medicare-approved amount, plus an excess charge . Note: A provider who treats Medicare patients but does not accept assignment cannot charge more ...
Is MSN a bill?
How much Medicare approved and paid. How much you owe. Previously known as the Explanation of Medicare Benefits, the MSN is not a bill. You should not send money to Medicare after receiving an MSN. Your provider will bill you separately.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Does Medicare cover nursing home care?
Your doctors will usually bill Medicare, which covers most Part A services at 100% after you’ve met your deductible.
Does Medicare reimburse doctors?
Medicare Reimbursement for Physicians. Doctor visits fall under Part B. You may have to seek reimbursement if your doctor does not bill Medicare. When making doctors’ appointments, always ask if the doctor accepts Medicare assignment; this helps you avoid having to seek reimbursement.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.