
Does Medicare pay for custodial care?
The most common question regarding payment options is if the care is covered by Medicaid or Medicare. Medicare may pay for short term custodial care that lasts for 99 days or less if requested by a medical professional and paired with skilled nursing care. In general, custodial care benefits are not provided for the long term.
Does Medicare cover long-term care?
Medicare doesn’t cover long-term care (also called Custodial care), if that's the only care you need. Most nursing home care is custodial care. Your costs in Original Medicare You pay 100% for non-covered services, including most long-term care.
Does Medicare pay for 24 hour care?
Medicare doesn't pay for: 1 24-hour-a-day care at home 2 Meals delivered to your home 3 Homemaker services (like shopping, cleaning, and laundry), when this is the only care you need 4 Custodial or personal care (like bathing, dressing, or using the bathroom), when this is the only care you need
Does the VA pay for custodial care?
Veterans benefits will cover some if not all custodial care services. When those services are given in the home or in a VA hospital, 100% of care is covered. In some cases, SSI disability recipients are able to avail custodial care benefits. The most common question regarding payment options is if the care is covered by Medicaid or Medicare.
How long does Medicare Part A pay for hospital stay?
90 daysDoes the length of a stay affect coverage? Medicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.
Does Medicare cover any portion of long term care?
Medicare doesn't cover long-term care (also called custodial care) if that's the only care you need. Most nursing home care is custodial care, which is care that helps you with daily living activities (like bathing, dressing, and using the bathroom).
What is the maximum period of time that Medicare will pay for any part of a Medicare beneficiary's costs associated with care delivered in a skilled nursing facility?
100 daysMedicare covers up to 100 days of "skilled nursing care" per illness, but there are a number of requirements that must be met before the nursing home stay will be covered.
Does Medicare Part A pay for everything?
Original Medicare (Parts A & B) covers many medical and hospital services. But it doesn't cover everything.
What is the 100 day rule for Medicare?
You can get up to 100 days of SNF coverage in a benefit period. Once you use those 100 days, your current benefit period must end before you can renew your SNF benefits. Your benefit period ends: ■ When you haven't been in a SNF or a hospital for at least 60 days in a row.
What is the benefit period for Medicare Part A?
A benefit period begins when you are admitted to the hospital and ends when you have been out of the hospital for 60 days, or have not received Medicare-covered care in a skilled nursing facility (SNF) or hospital for 60 consecutive days from your day of discharge.
Can Medicare benefits be exhausted?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
What is not covered by Medicare Part A?
A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care. A television or telephone in your room, and personal items like razors or slipper socks, unless the hospital or skilled nursing facility provides these to all patients at no additional charge.
What is the 3 day rule for Medicare?
The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay. The 3-consecutive-day count doesn't include the discharge day or pre-admission time spent in the Emergency Room (ER) or outpatient observation.
Does Medicare Part A cover 100 percent?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
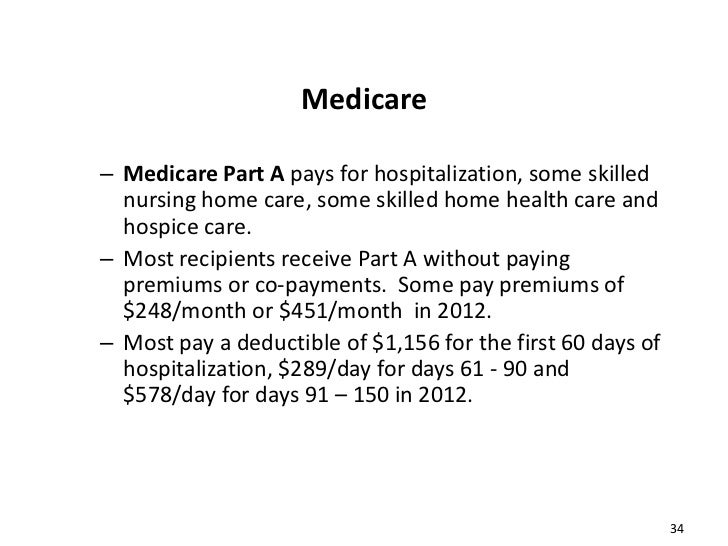
What is the difference between Medicare Part A and Part B?
Part A is hospital coverage, while Part B is more for doctor's visits and other aspects of outpatient medical care. These plans aren't competitors, but instead are intended to complement each other to provide health coverage at a doctor's office and hospital.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
How can I pay for assisted living with no money?
Medicaid. There are several different Medicaid programs that provide financial assistance for assisted living. Home and Community Based Services (HCBS) Waivers and 1915 Waivers are the most common form of this assistance and, as of 2019, are available in 44 states.
Which of the following is not a benefit trigger under long-term care policies?
Which of the following is not a benefit trigger under long-term care policies? Financial need is not a benefit trigger for long-term care policy benefits.
What can a nursing home take for payment?
We will take into account most of the money you have coming in, including:state retirement pension.income support.pension credit.other social security benefits.pension from a former employer.attendance allowance, disability living allowance (care component)personal independence payment (daily living component)
Custodial Care Services Covered by Medicare
Neither Medicare Part A, Medicare Part B, nor Medicare Part C (also called a Medicare Advantage plan) covers custodial care, even short-term.
What Medicare Pays for Custodial Care
Neither Medicare Part A, Medicare Part B, nor a Medicare Part C Medicare Advantage plan pays anything for custodial care services. Options to consider for receiving this type of care include Medicaid and long-term care insurance.
What is skilled nursing?
Skilled nursing care is for seniors who are in need of medical assistance while they are recovering from a procedure or a senior who is receiving hospice or palliative care. Skilled nurses are trained in medical procedures and have been licensed to provide limited medical services to seniors or other patients.
How long does Medicaid pay for custodial care?
Medicare may pay for short term custodial care that lasts for 99 days or less if requested by a medical professional and paired with skilled nursing care. In general, custodial care benefits are not provided for the long term.
Why do people hire caregivers?
Many families will hire a caregiver to supplement the care they provide for their loved ones in their own homes. In addition to home-based custodial care, it is also available in long term care facilities, retirement homes and assisted living communities.
How much does a custodial caregiver pay?
On average, you can expect to pay around $1,500 monthly for custodial care in an adult day care facility while a custodial caregiver who works in the home averages around $4,000 monthly for non-medical custodial care.
How many levels of custodial care are there?
There are four basic levels of custodial care: full-time, live-in, as-needed and part-time. Each level will have a different rate. You should also decide if you plan to search for a caregiver for your loved one on your own or if you take help from a professional agency.
How much does assisted living cost?
An assisted living home can range from $2,900 a month up to $6,000 a month depending on the location and other provided services. Nursing homes with private rooms that offer custodial care are more on the higher end of the charge scale at around $8,000 a month.
Why do elderly people need custodial care?
Seniors who are suffering from a medical condition or who are recovering from a medical procedure may be good candidates for custodial care.
Custodial care
Long-term care can be described as a wide range of services and support you may need to address your personal care needs. Most long-term care is assistance with the basic personal tasks of everyday life. Custodial care is a type of long-term care, defined by Medicare as “non-skilled personal care, like help with activities of daily living.”
Skilled nursing care
In contrast to custodial care, skilled care is for short-term medical conditions delivered by licensed medical professionals, usually in a skilled nursing facility (SNF). You may qualify for Medicare coverage of SNF inpatient care if your physician certifies that it is medically necessary.
Home health services
Medicare coverage also includes home health services. To qualify, your doctor must perform a face-to-face evaluation, determine that you are homebound, certify that home health services are medically necessary and order the services through a Medicare-certified home health agency.
What is long term care?
What it is. Long-term care is a range of services and support for your personal care needs. Most long-term care isn't medical care. Instead, most long-term care is help with basic personal tasks of everyday life like bathing, dressing, and using the bathroom, sometimes called "activities of daily living.".
What is custodial care?
custodial care. Non-skilled personal care, like help with activities of daily living like bathing, dressing, eating, getting in or out of a bed or chair, moving around, and using the bathroom. It may also include the kind of health-related care that most people do themselves, like using eye drops.
What is custodial care?
Custodial care is non-medical care that helps individuals with activities of daily living and basic care needs. Custodial care is typically recommended by a medical professional, even though the actual providers of custodial care are not medical professionals themselves. Custodial care is a popular form of long-term support for seniors whose ...
What is skilled nursing?
Skilled nursing professionals are medically trained, licensed and work under the supervision of a team of medical providers. There are many levels of medical skilled nursing providers such as certified nursing assistants, registered nursing assistants and registered nurses who are often employed for specialized care and terminal patient needs. These types of caregivers are essential for those who need medication dispensed, wound care, physical therapy, intravenous injections, catheters, etc.
What is the best insurance for senior care?
Long Term Care Insurance : Long term care insurance (LTC) is one of the best options for paying for senior custodial care, especially when combined with supplemental Medicare coverage. These fixed-priced policies vary in coverage, but often provide reimbursement for care for several years.
How much does adult day care cost?
Adult Day Care — $1,517 per month (depending upon hours) While not commonly utilized for non-medical custodial care situations, some seniors opt to start with these options to maintain continuity in care. These are the average costs associated with facility style living arrangements.
Does health insurance cover custodial care?
Paying for Custodial Care. Those with traditional health insurance plans may have benefits available for informal caregivers that provide custodial care, but will need to check their policy carefully to determine whether they offer this coverage, as many only reimburse costs associated with skilled nursing care.
Do custodial caregivers need certification?
Most custodial caregivers do opt for some type of training and certification to become Homemakers, Personal Care Assistants and Home Health Aides, yet their services are still limited to non-medical roles.
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
What is intermittent skilled nursing?
Intermittent skilled nursing care (other than drawing blood) Physical therapy, speech-language pathology, or continued occupational therapy services. These services are covered only when the services are specific, safe and an effective treatment for your condition.
What is an ABN for home health?
The home health agency should give you a notice called the Advance Beneficiary Notice" (ABN) before giving you services and supplies that Medicare doesn't cover. Note. If you get services from a home health agency in Florida, Illinois, Massachusetts, Michigan, or Texas, you may be affected by a Medicare demonstration program. ...
What is the eligibility for a maintenance therapist?
To be eligible, either: 1) your condition must be expected to improve in a reasonable and generally predictable period of time, or 2) you need a skilled therapist to safely and effectively make a maintenance program for your condition , or 3) you need a skilled therapist to safely and effectively do maintenance therapy for your condition. ...
Can you get home health care if you attend daycare?
You can still get home health care if you attend adult day care. Home health services may also include medical supplies for use at home, durable medical equipment, or injectable osteoporosis drugs.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.
How do I contact Medicare for home health?
If you have questions about your Medicare home health care benefits or coverage and you have Original Medicare, visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) . TTY users can call 1-877-486-2048. If you get your Medicare benefits through a Medicare Advantage Plan (Part C) or other
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
Why is home health important?
In general, the goal of home health care is to provide treatment for an illness or injury. Where possible, home health care helps you get better, regain your independence, and become as self-sucient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
Can Medicare take home health?
In general, most Medicare-certified home health agencies will accept all people with Medicare . An agency isn’t required to accept you if it can’t meet your medical needs. An agency shouldn’t refuse to take you because of your condition, unless the agency would also refuse to take other people with the same condition.
