How long does it take to get approved for Medicare?
Your IEP for Medicare is the three months before your 65 th birthday, the month of your 65 th birthday, and the three months after your 65 th birthday. Signing up for Medicare at any time during this seven-month window will keep you from facing financial penalties. Once you sign up for Medicare, you will get a red, white and blue Medicare card in the mail.
How long does it take LCA to get approved for?
Medicare applications generally take between 30-60 days to obtain approval. How do I get a Medicare card for the first time? Getting a Medicare card starts with a phone call: Social Security: 1-800-772-1213, Monday through Friday, from 7AM to 7PM. If …
What documents are needed for Medicare application?
Jan 01, 2022 · Medicare applications generally take between 30-60 days to obtain approval. You May Like: Does Medicare Cover Mental Health Visits. Documents Needed If You Sign Up In Person. An original or certified copy of your birth certificate or other proof of birth; Proof of United States citizenship or legal residency if not born in the U.S.
When is the deadline to apply for Medicare?
Jan 31, 2020 · You are able to begin applying for Medicare three months before your 65th birthday. This date marks the beginning of your Initial Enrollment Period. This period lasts for a total of seven months, and you must apply for Medicare coverage during this period to avoid having to pay late enrollment penalties.
How To Sign Up For Medicare Part B
Beneficiaries collecting Social Security benefits when they age into Medicare at 65 will automatically be enrolled. Youll receive your Medicare card the month before your birthday. If youre not collecting Social Security benefits, youll need to enroll yourself. You can apply online, over the phone, or in-person.
Exact Answer: Up To 30 Days
The Medicare application can be applied to online websites. The application process is quite easy. The process of application will not ask for many documents in major steps. The applicants may not have to sign in any documents while applying for the Medicare part B. The application doesnt charge any fees from the applicant.
What Medicare Part B Covers
First, lets take a look at what Medicare Part B actually covers. Medicare Part B covers medical treatments and services under two classifications: medically necessary services and preventive services.
When To Enroll In Medicare If I Am Receiving Disability Benefits
If you are under 65 and receiving certain disability benefits from Social Security or the Railroad Retirement Board, you will be automatically enrolled in Original Medicare, Part A and Part B, after 24 months of disability benefits. The exception to this is if you have end-stage renal disease .
What Happens After I Register For Medicare Online
Once you have submitted your application, it will be reviewed by Medicare to ensure all the information is accurate and complete. You should double-check your contact information to make sure it is correct.
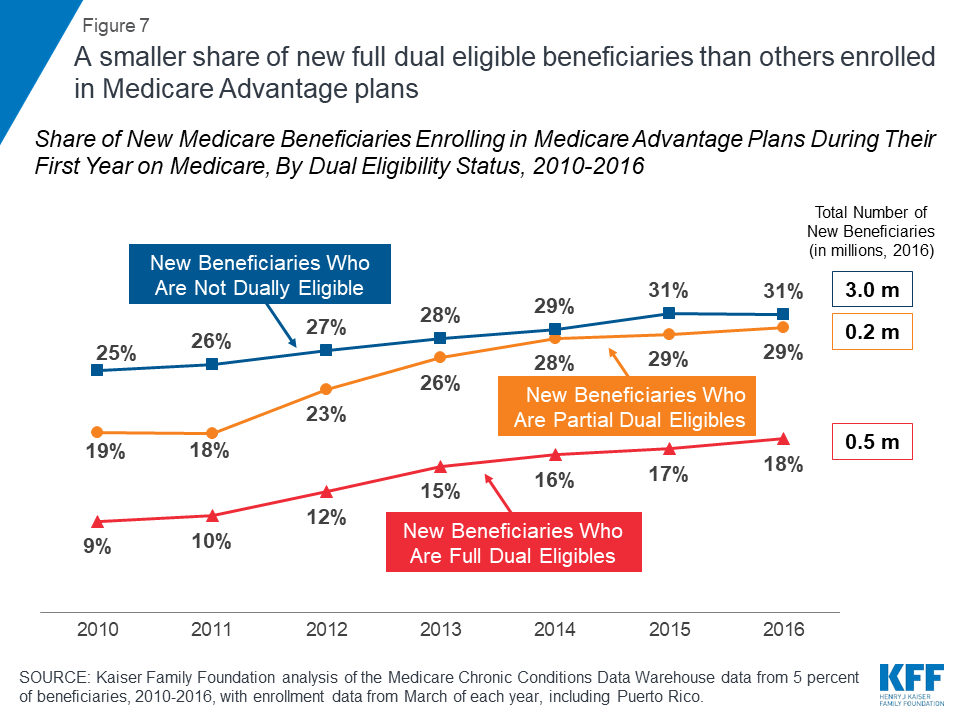
Medicare Advantage Open Enrollment Period
Medicare Advantage Open Enrollment happens every year from Jan. 1 to March 31. If youre enrolled in a Medicare Advantage plan and want to make changes, you can do one of these:
How Do You Apply By Phone
Call 772-1213 or TTY 325-0778 between 7 a.m. and 7 p.m. from Monday through Friday. 5 Keep in mind that this process takes longer because forms have to be mailed to you, which you then complete and send back. At peak times, applying for Medicare by phone could take a month or more.
How long does it take to get Medicare?
This date marks the beginning of your Initial Enrollment Period. This period lasts for a total of seven months , and you must apply for Medicare coverage during this period to avoid having to pay late enrollment penalties. The seven months encompass the three months prior to your birthday, your birth month, and the three months following your birth month.
How many months are you eligible for Medicare?
The seven months encompass the three months prior to your birthday, your birth month, and the three months following your birth month. You are able to apply for Medicare in a few different ways. If you prefer to apply in person, you can do so at your local Social Security office.
What happens after you enroll in Medicare?
After enrolling in Medicare, you will receive your Medicare identification card so that you can use it to receive healthcare coverage at a variety of different facilities across the United States. Since Medicare is a government-run entity, applications for insurance coverage are handled by the Social Security Administration.
Is Medicare dependent on Social Security?
Unlike Social Security benefits, Medicare eligibility is not dependent on retirement. However, if you are already receiving Social Security benefits at the age of 65, you will automatically be enrolled in Medicare. It is important to note that even if you are automatically enrolled in Part A and Part B, you still must apply to Part D separately ...
Does Medicare cover prescription drugs?
Original Medicare encompasses both Part A and Part B. At the time you apply for Original Medicare, you also have the ability to sign up for Medicare Part D coverage, which covers prescription drugs.
Exact Answer: Up to 30 days
The Medicare application can be applied to online websites. The application process is quite easy. The process of application will not ask for many documents in major steps. The applicants may not have to sign in any documents while applying for the Medicare part B. The application doesn’t charge any fees (Application fees) from the applicant.
Why It Take This Long To Get Medicare Part B After Applying?
The Medicare application takes time for approval and before that, no one is eligible to enjoy the benefits. There are certain rules, regulations, and procedures to be followed while applying for Medicare part B. If someone has all the information in the favour of the application and satisfies the eligibility criteria.
Conclusion
The time for the medicare part B would be around 30 days. The individuals should know about the enrollment (deadlines). Checking and learning all the eligibility criteria is vital. Avoiding any misrepresentation of information would call for a fair application process.
How long does it take to get a Medicare card?
You’ll receive your card within about 3 weeks from the date you apply for Medicare. You should carry your card with you whenever you’re away from home.
When do you start receiving Medicare benefits?
Your benefits may not start until 3 months after applying, so it’s important to apply 3 months before your 65th birthday to start receiving coverage that day. If you already collect Social Security income benefits or Railroad Retirement Benefits, you will automatically be enrolled in Medicare when you turn 65.
How to check my Medicare application?
How to check your Medicare application online. If you applied for Medicare online, you can check the status of your application through your Medicare or Social Security account. You can also visit the Check Enrollment page on Medicare.gov and find information about your enrollment status by entering your: ZIP code. Medicare number.
How to check Medicare Part D enrollment?
date of birth. Medicare Part A effective date. You can also check the status of your application by visiting or calling a Social Security office. You can ask your pharmacy to check the status of your Medicare Part D enrollment by sending a test claim. You can also call the Member Services department ...
How to change Medicare plan when you get it in mail?
When you get your Medicare card in the mail, make sure the information is correct. Contact Social Security if you want to change your plan. There may be fees included in changing plans or adding additional coverage if you didn’t do it when you were eligible.
What to do if your application has been denied?
Once your application has been reviewed, you should receive a letter in the mail to confirm whether you’ve been enrolled in the program or not. If your application has been denied, the letter will explain why this decision was made and what to do next.
Is the application process free?
The application is completely free. Once you apply, you’ll be able to check on the status of your application at any time. This article explains how to check on your application to make sure it’s being processed.
What does prior authorization mean?
Prior authorization means your doctor must get approval before providing a service or prescribing a medication. Now, when it comes to Advantage and Part D, coverage is often plan-specific. Meaning, you should contact your plan directly to confirm coverage.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
Do you need prior authorization for Medicare Part B?
Part B covers the administration of certain drugs when given in an outpatient setting. As part of Medicare, you’ll rarely need to obtain prior authorization. Although, some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form. Your doctor will provide this form.
Does Medicare Advantage cover out of network care?
Unfortunately, if Medicare doesn’t approve the request, the Advantage plan typically doesn’t cover any costs, leaving the full cost to you.
Does Medicare require prior authorization?
Medicare Part A Prior Authorization. Medicare, including Part A, rarely requires prior authorization. If it does, you can obtain the forms to send to Medicare from your hospital or doctor. The list mostly includes durable hospital equipment and prosthetics.
Does Medicare cover CT scans?
If your CT scan is medically necessary and the provider (s) accept (s) Medicare assignment, Part B will cover it. Again, you might need prior authorization to see an out-of-network doctor if you have an Advantage plan.
How long does it take for Medicare to start?
On the other hand, for disability applicants who apply for benefits only when they become disabled, and not before, the date that their Medicare coverage will start is more likely to be two years and five months after they apply for disability.
How long do you have to wait to get Medicare?
You have to wait two years after you are entitled to disability benefits to get Medicare unless you fit into an exception. All Social Security disability insurance (SSDI) recipients can receive Medicare coverage two years after the first month they are eligible for their monthly disability benefits. This does not mean that every individual who is ...
How long is the waiting period for Medicare?
In general, the two-year waiting period for Medicare is calculated from your date of SSDI entitlement—when you are eligible to start receiving monthly benefits. This is usually the date your disability began, plus five months (due to the five-month waiting period for SSDI).
When will Makayla get her SSDI?
Makayla applies for disability on August 1, 2019, the day after she quit work due to her disability. Thirteen months later, on September 1, 2020, she is approved for SSDI benefits with a disability onset date of August 1, 2019. She is eligible for retroactive benefits only going back to January 1, 2020, five months after her disability onset date. Because her date of entitlement is January 1, 2020, she'll be eligible for Medicare on January 1, 2022. Note that her eligibility for Medicare starts two years and five months after her application date.
When will Isaiah be eligible for Medicare?
But he is eligible for retroactive benefits only going back to October 1, 2018, five months after his disability onset date. Because his date of entitlement is October 1, 2018, he'll be eligible for Medicare on October 1, 2020. Note that his eligibility for Medicare starts only 14 months after his application date, and only one month after his decision date.
When does Medicare cover end stage renal disease?
If you require ongoing dialysis or a kidney transplant, Medicare coverage can begin the third month after the month in which your dial ysis began. Amyotrophic lateral sclerosis (ALS). Individuals with amyotrophic lateral sclerosis (ALS) qualify for Medicare as soon as they are eligible ...
Can I get medicaid with low income?
Those with low income and low assets may qualify for the Medicaid program during the two-year waiting period for Medicare. States set their own rules regarding Medicaid eligibility, but those granted SSI at the same time as SSDI automatically qualify for Medicaid.
How long does it take to switch to another Medicare Advantage plan?
If you permanently move out of your Medicare Advantage plan’s coverage area or move to an area with more available plans, you may switch to another Medicare Advantage plan beginning the month before your move and lasting for two months.
How long does Medicare Advantage coverage last?
If you had a Medicare Advantage plan with prescription drug coverage which met Medicare’s standards of “creditable” coverage and you were to lose that coverage through no fault of your own, you may enroll in a new Medicare Advantage plan with creditable drug coverage beginning the month you received notice of your coverage change and lasting for two months after the loss of coverage (or two months after receiving the notice, whichever is later).
How long do you have to disenroll from Medicare Advantage?
If you enrolled in a Medicare Advantage plan when you first became eligible for Medicare, you have 12 months to disenroll from the plan and transition back to Original Medicare.
What happens if you don't enroll in Medicare at 65?
If you did not enroll in Medicare when you turned 65 because you were still employed and were covered by your employer’s health insurance plan, you will be granted a Special Enrollment Period.
How often can you change your Medicare Advantage plan?
If you move into, out of, or currently reside in a facility of special care such as a skilled nursing home or long-term care hospital, you may enroll in, disenroll from, or change a Medicare Advantage plan one time per month.
What is a special enrollment period?
A Special Enrollment Period (SEP) is an enrollment period that takes place outside of the annual Medicare enrollment periods, such as the annual Open Enrollment Period. They are granted to people who were prevented from enrolling in Medicare during the regular enrollment period for a number of specific reasons.
What to do if you don't fit into Medicare?
If your circumstances do not fit into any of the Special Enrollment Periods described above, you may ask the Centers for Medicare and Medicaid Services (CMS) for your own Special Enrollment Period based on your situation.
