
How much more does individual therapy cost with Medicare?
In 2022, you pay $233 for your Part B. . After you meet your deductible for the year, you typically pay 20% of the. for these: Most doctor services (including most doctor services while you're a hospital inpatient) Outpatient therapy. , you pay 20% of the. Medicare-Approved Amount.
How long should a psychotherapy session be?
Dec 27, 2021 · The program must include at least 20 hours per week of counseling and therapy services. Treatment must be supervised by a licensed physician. The program must offer multiple types of therapy, including individual and group counseling. Therapy …
Does Medicare cover therapy and counseling services?
May 13, 2019 · Most mental health services are provided at an outpatient facility. Medicare Part B benefits offer coverage for a range of psychotherapy services, which can include individual or group therapy sessions. However, the therapist or doctor administering these services must meet the state’s requirement for licensing.
What is the Medicare reimbursement rate for 60 minute therapy?
Apr 08, 2022 · Medicare no longer caps medically necessary physical therapy coverage. For outpatient therapy in 2022, if you exceed $2,150 with physical therapy and speech-language pathology services combined, your therapy provider must add a modifier to their billing to show Medicare that you continue to need and benefit from therapy.
How many minutes is a therapy unit?
Unlike service-based CPT codes, time-based CPT codes can be billed as multiple units in 15-minute increments. Meaning that one unit would represent 15 minutes of therapy. A therapist must provide direct one-to-one therapy for at least 8 minutes to receive reimbursement for a time based treatment code.
How many PT sessions will Medicare pay for?
A person's doctor recommends 10 physical therapy sessions at $100 each. The individual has not paid their Part B deductible for the year. They will pay the Part B deductible of $203. Part B will pay 80% of the expense after the $203 deductible payment.Mar 6, 2020
How many therapy units is 45 minutes?
3 billable unitsTimed Minutes: 45 However, billing is based ultimately on total timed minutes – 45 in this case, and equivalent to 3 billable units. Those 7 minutes spent on therapeutic activity still count toward timed minutes because Therapeutic Activity is a timed code.Dec 16, 2019
How many therapy units is 35 minutes?
I. If you perform an initial evaluation that lasts 35 minutes and a 7-minute therapeutic exercise, you can only bill one units for the initial evaluation.Oct 31, 2016
Does Medicare pay for PT at home?
Yes, Medicare will cover physical therapy at home if it is medically necessary. Medicare covers a variety of home health care services, including physical therapy, although they are usually covered under Part A rather than Part B.May 18, 2020
What will the Medicare premium be in 2021?
The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.Nov 12, 2021
How are therapy minutes calculated?
To calculate the number of billable units for a date of service, providers must add up the total minutes of skilled, one-on-one therapy and divide that total by 15. If eight or more minutes remain, you can bill one more unit.Sep 13, 2018
Do Medicare Advantage plans follow 8-minute rule?
Medicare requires providers to adhere to the 8-Minute Rule; MA plans may not.Nov 9, 2018
Does the 8-minute rule apply to Medicare Part A?
Please note that this rule applies specifically to Medicare Part B services (and insurance companies that have stated they follow Medicare billing guidelines, which includes all federally funded plans, such as Medicare, Medicaid, TriCare and CHAMPUS). The rule does not apply to Medicare Part A services.Aug 12, 2019
How many minutes is 7 units of therapy?
1 unit: ≥ 8 minutes through 22 minutes 2 units: ≥ 23 minutes through 37 minutes 3 units: ≥ 38 minutes through 52 minutes 4 units: ≥ 53 minutes through 67 minutes 5 units: ≥ 68 minutes through 82 minutes 6 units: ≥ 83 minutes through 97 minutes 7 units: ≥ 98 minutes through 112 minutes 8 units: ≥ 113 minutes through 127 ...Mar 21, 2011
What is the AMA 8 minute rule?
The AMA uses similar guidelines as Medicare in that 1 unit equals 8 minutes. Where the AMA differs is that there is no cumulative restriction or adding of minutes, even for time-based codes. Every code will be allowed 1 unit for each 8 minutes performed.Nov 21, 2019
What is the rule of 8?
If eight or more minutes are left over, you can bill for one more unit; if seven or fewer minutes remain, you cannot bill an additional unit.Jan 11, 2019
When Does Medicare Cover Counseling Services?
Medicare has comprehensive mental health care benefits for both inpatient and outpatient counseling services. In order to be covered, your counseling or therapy must be provided by a licensed healthcare professional, such as:
Does Medicare Cover Counseling if You Have Medicare Advantage?
Medicare Advantage is private insurance, which means that your coverage may be different depending on the specific plan you choose. At a minimum, Medicare Advantage must provide the same level of counseling and therapy coverage as Original Medicare.
Does Medicare Cover Therapy with Prescription Drugs?
If you receive mental health care services in an inpatient setting, Part A covers the medications your doctor prescribes.
Getting the Counseling You Need
You don’t have to wait for your annual wellness visit or depression screening to talk to your doctor about mental health care. Medicare pays for visits with your primary care doctor if you want to talk about your mental health concerns now.
What are the different types of mental health treatment?
In other cases, your therapist may specialize in one or two styles of therapy that address specific types of mental health needs. The most common forms of therapy include: 1 Cognitive behavioral therapy. CBT has broad applicability and focuses on the personalized development of effective coping skills to counteract harmful patterns of thought and behaviors. 2 Dialectical behavior therapy. DBT, like CBT, address mental health needs through identifying problematic patterns and creating healthier habits to replace them, but it is typically better suited for people who struggle with frequent suicidal ideation, certain personality disorders and PTSD. 3 Interpersonal therapy. IPT helps you adjust to difficult or new circumstances as it relates to your social experiences and relationships with others. This can involve practicing important communication skills and developing better situational awareness. 4 Psychoanalysis and psychodynamic therapy. Both of these techniques focus on your childhood and past experiences in order to illustrate deeply ingrained behaviors and beliefs that contribute to mental illness or emotional difficulties. Psychoanalysis is the more intense of the two styles and may involve several sessions in a week. 5 Supportive therapy. This patient-led style of therapy encourages you to identify personal obstacles and the resources necessary to help you overcome them. The therapist provides guidance and information to help you structure a plan and maintain your goals.
What is the most common form of therapy?
The most common forms of therapy include: Cognitive behavioral therapy . CBT has broad applicability and focuses on the personalized development of effective coping skills to counteract harmful patterns of thought and behaviors. Dialectical behavior therapy.
What is psychotherapy?
As described by the American Psychiatric Association (APA), psychotherapy uses a number of techniques to help patients improve their mental health by addressing troublesome behaviors and emotional difficulties.
Why do you need a diagnostic test?
Other tests may be required in order to monitor any medication’s impact on the body , such as checking blood pressure or liver and kidney function.
Does Medicare cover psychotherapy?
Most mental health services are provided at an outpatient facility. Medicare Part B benefits offer coverage for a range of psychotherapy services, which can include individual or group therapy sessions . However, the therapist or doctor administering these services must meet the state’s requirement for licensing.
Which is more intense, psychoanalysis or supportive therapy?
Both of these techniques focus on your childhood and past experiences in order to illustrate deeply ingrained behaviors and beliefs that contribute to mental illness or emotional difficulties. Psychoanalysis is the more intense of the two styles and may involve several sessions in a week. Supportive therapy.
Why is Physical Therapy Valuable?
According to the American Physical Therapy Association (APTA), physical therapy can help you regain or maintain your ability to move and function after injury or illness. Physical therapy can also help you manage your pain or overcome a disability.
Does Medicare Cover Physical Therapy?
Medicare covers physical therapy as a skilled service. Whether you receive physical therapy (PT) at home, in a facility or hospital, or a therapist’s office, the following conditions must be met:
What Parts of Medicare Cover Physical Therapy?
Part A (hospital insurance) covers physical therapy as an inpatient service in a hospital or skilled nursing facility (SNF) if it’s a Medicare-covered stay, or as part of your home health care benefit.
Does Medicare Cover In-home Physical Therapy?
Medicare Part A covers in-home physical therapy as a home health benefit under the following conditions:
What Are the Medicare Caps for Physical Therapy Coverage?
Medicare no longer caps medically necessary physical therapy coverage. For outpatient therapy in 2021, if you exceed $2,150 with physical therapy and speech-language pathology services combined, your therapy provider must add a modifier to their billing to show Medicare that you continue to need and benefit from therapy.
What is OT in Medicare?
Occupational therapy (OT) is a form of rehabilitative care that can help people regain strength, dexterity, and skill after surgery, illness, or injury. For people on Medicare, OT can be used to enhance or restore the fine and basic motor skills that make daily living tasks easier. Medicare covers OT services when they’re medically necessary.
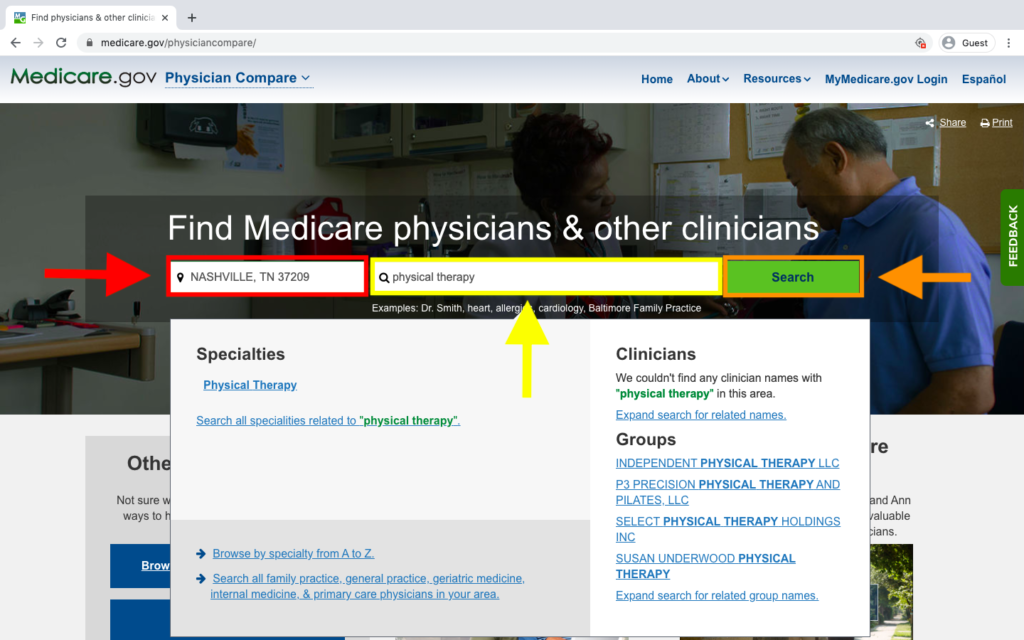
What is Medicare Part B?
Medicare Part B covers the cost of outpatient OT services. These may be received at a therapist’s office, doctor’s office, hospital, clinic, or other medical facility. To receive coverage, you must get OT from a Medicare-approved provider. You can search for approved providers in your area here.
How much is Part B deductible?
Part B costs. If your claim is covered under Part B, you must meet an annual deductible of $203 before coverage for OT services starts. Once you’ve met this deductible, you’ll be responsible for paying 20 percent of the Medicare-approved costs of OT services.
What are some good exercises to help with memory?
Some of these will also use props, such as light weights or balls. OT exercises also may be geared toward memory enhancement. Tools that support memory — such as crossword puzzles, jigsaw puzzles, and matching games — may be used. OT may be beneficial for a wide range of conditions including: Parkinson’s disease.
What is the purpose of exercise for caregivers?
exercises to enhance range of motion. training for you and your caregivers on how to use durable medical equipment, such as canes and walkers. training for your caregivers on safety techniques for your care, such as safe car transfers.
Why is OT important?
For example, with training received through OT, you may be better able to open pill bottles, removing a barrier between you and the medications you need. By increasing muscle strength, stability, and balance, OT can help you avoid accidents after hospital discharge.
Does Medicare cover OT?
It can be used to treat many common conditions such as arthritis, Parkinson’s disease, and dementia. Medicare covers the costs of OT. Medicare Part A covers inpatient OT, while Medicare Part B covers OT services received as an outpatient.
How long does a HCPCS code have to be in a day?
CMS requires that when you provide only one 15-minute timed HCPCS code in a day, that you do not bill that service if performed for less than 8 minutes. When providing more than one unit of service, the initial and subsequent service must each total at least 15 minutes, and the last unit may count as a full unit of service if it includes at least 8 minutes of additional services. Do not count all treatment minutes in a day to one HCPCS code if more than 15 minutes of one or more other codes are furnished.
How long does a POC last?
The physician’s/NPP’s signature and date on a correctly written POC (with or without an order) satisfies the certification requirement for the duration of the POC or 90 calendar days from the date of the initial treatment, whichever is less. Include the initial evaluation indicating the treatment need in the POC.
What is CERT contractor?
The Comprehensive Error Rate Testing (CERT) Part A and Part B (A/B) Contractor Task Force is independent from the Centers for Medicare & Medicaid Services (CMS) CERT team and CERT contractors, which are responsible for calculation of the Medicare fee-for-service improper payment rate.
How often do you need to recertify a POC?
Sign the recertification, documenting the need for continued or modified therapy whenever a significant POC modification becomes evident or at least every 90 days after the treatment starts. Complete recertification sooner when the duration of the plan is less than 90 days, unless a certification delay occurs. CMS allows delayed certification when the physician/NPP completes certification and includes a delay reason. CMS accepts certifications without justification up to 30 days after the due date. Recertification is timely when dated during the duration of the initial POC or within 90 calendar days of the initial treatment under that plan, whichever is less.
What is a POC in rehabilitation?
Outpatient rehabilitation therapy services must relate directly and specifically to a written treatment plan (also known as the POC). You must establish the treatment plan/POC before treatment begins, with some exceptions. CMS considers the treatment plan/POC established when it is developed (written or dictated) by a PT, an OT, an SLP, a physician, or an NPP. Only a physician may establish a POC in a Comprehensive Outpatient Rehabilitation Facility (CORF).
Why should therapy sessions be under an hour?
Keeping therapy sessions under an hour may also motivate both parties to make the best of the time allotted. Advertisement. “It can encourage both therapist and client to get to the heart of the problem rather quickly,” Stuempfig noted.
Why is it important to sit with pain for a long time?
First of all, the length of time feels more contained, so it lessens the risk of over-exposure to painful emotions. “It could feel traumatic to a client to sit with their pain for an extended period of time, risking emotional harm and causing the client to not return due to fear of retraumatization,” Stuempfig said.
Why do therapists suggest meeting more frequently?
Giving people increments of information and allowing them to process it in sections is good for the best possible outcome for treatment.”. This is why therapists often suggest meeting more frequently, rather than extending sessions, when clients express a desire for more time.
How long is a therapy session?
While therapists take many different approaches to meeting frequency and length, the norm for individual therapy (i.e., therapy with one client) tends to be weekly 45- or 50-minute sessions.
How long should a client have a clear endpoint?
Having a clear endpoint after less than an hour can help create a safe space for the client to feel, process and contain intense emotions, rather than go into it with the sense that there’s no end in sight. There are practical, psychological and insurance-related reasons to limit session length to 45 or 50 minutes.
What is the importance of therapy?
The important thing to keep in mind is that therapy is an ongoing conversation, and the real change happens when the clients practice what they learn in their lives outside the therapist’s office. The focus should be on the skills and insights they gain during sessions and how they’ll implement them ― not the length of the sessions.
How long is a 45 minute session?
A common billing code is 90834, which denotes 45 minutes of individual psychotherapy but can be used for sessions ranging from 38 to 52 minutes.
What is CPT code 90837?
CPT Code 90837 is a procedure code that describes a 60 minute individual psychotherapy session performed by a licensed mental health provider. 90837 is considered a routine outpatient CPT Code and is one of the most common CPT codes used in mental health insurance claims coding and billing. We’ll teach you the ins and outs ...
What is the add on code for CPT?
Add-on CPT Code 99354 is defined as a prolonged services code and is defined as an extra 30-74 minutes of therapy. 99354 used to only be allowed by Medical Doctor’s, but has since expanded and is applicable to 90837 and 90487.
How long is 90837?
90837 is defined as a session of 60 minutes, ranging from 53 minutes to longer. The only difference between 90834 (the other commonly used CPT code) and 90837 is the time. 90837 is 60 minutes and 90834 is 45 minutes. Not every therapist does sessions at these exact time intervals.
How much more does 90837 cost than 90834?
Due to the extended length, 90837 does indeed pay more than 90834. Depending on your credentials, we’ve found that 90837 can pay between $9-20 more on average than a 90834 appointment. This amounts to typically ~13-20% more per session. Medicare has published their 60 minute individual therapy reimbursement rates.
Is a 90837 preauthorization required?
Typically no, authorization is not required. Up until very recently one of the largest insurers, United Healthcare required authorization for 90837. The pre-authorization requirement was not extended onto the other frequently used procedure codes, 90791 or 90834.
Does United Healthcare cover 90387?
Still, the vast majority of insurance companies consider 90387 to be routine and will cover it as they would other mental health procedure codes. Thankfully, United Healthcare has reversed course and as of 2019 has started accepting 90837 without prior authorization.
What is telehealth in Medicare?
Medicare telehealth services include office visits, psychotherapy, consultations, and certain other medical or health services that are provided by a doctor or other health care provider who’s located elsewhere using interactive 2-way real-time audio and video technology.
What do you call Medicare if you suspect fraud?
If you suspect fraud, call 1-800-MEDICARE.
How much does Medicare pay for telehealth?
You pay 20% of the Medicare-approved amount for your doctor or other health care provider’s services, and the Part B Deductible applies. For most telehealth services, you'll pay the same amount that you would if you got the services in person.
When can telehealth be used?
Due to the Coronavirus (COVID-19) Public Health Emergency, doctors and other health care providers can use telehealth services to treat COVID-19 (and for other medically reasonable purposes) from offices, hospitals, and places of residence (like homes, nursing homes, and assisted living facilities) as of March 6, 2020.
Does Medicare offer telehealth?
Starting in 2020, Medicare Advantage Plans may offer more telehealth benefits than Original Medicare. These benefits can be available in a variety of places, and you can use them at home instead of going to a health care facility. Check with your plan to see what additional telehealth benefits it may offer.
How long is a delayed NPP certification good for?
Certifications are acceptable without justification for 30 days after they are due. Delayed certification should include one or more certifications or recertification's on a single signed and dated document.”
Does mandatory assignment apply to therapy?
The mandatory assignment provision does not apply to therapy services furnished by a physician/NPP or "incident to" a physician's/NPP’s service. However, when these services are not furnished on an assignment-related basis; the limiting charge applies.
