How long does it take for Medicare to respond to appeals?
Keep a copy of everything you send to Medicare as part of your appeal. In most cases, the QIC will send you a written response called a “Medicare Reconsideration Notice” about 60 days after the QIC gets your appeal request. If the QIC doesn’t issue a timely decision, you may ask the QIC to move your case to the next level of appeal.
What happens if I miss the deadline for appealing my Medicare claim?
If you missed the deadline for appealing, you may still file an appeal and get a decision if you can show good cause for missing the deadline. Fill out a " Redetermination Request Form [PDF, 100 KB] " and send it to the company that handles claims for Medicare.
How long do I have to appeal a health insurance decision?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide a reason for filing late.
How do you write a letter of Appeal for Medicare?
A written request to appeal should include: ■ Your name, address, and Medicare Number or member number. ■ The name of the drug you want your plan to cover. ■ Reason(s) why you’re appealing. ■ If you’ve appointed a representative, include the name of your representative and proof of representation.

How long does Medicare have to respond to an appeal for redetermination?
You'll generally get a decision from the MAC (either in a letter or an MSN) called a "Medicare Redetermination Notice" within 60 days after they get your request. If you disagree with this decision, you have 180 days after you get the notice to request a reconsideration by a Qualified Independent Contractor (QIC).
How often are Medicare appeals successful?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
Can I appeal a Medicare decision?
The plan must tell you, in writing, how to appeal. After you file an appeal, the plan will review its decision. Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
What should I say in a Medicare appeal?
What are the steps for filing an appeal for original Medicare?your name and address.your Medicare number (as shown on your Medicare card)the items you want Medicare to pay for and the date you received the service or item.the name of your representative if someone is helping you manage your claim.More items...•
How do I win a Medicare appeal?
Appeals with the best chances of winning are those where something was miscoded by a doctor or hospital, or where there is clear evidence that a doctor advised something and the patient followed that advice and then Medicare didn't agree with the doctor's recommendation.
Who has the right to appeal denied Medicare claims?
You have the right to appeal any decision regarding your Medicare services. If Medicare does not pay for an item or service, or you do not receive an item or service you think you should, you can appeal. Ask your doctor or provider for a letter of support or related medical records that might help strengthen your case.
What is appeal process?
Appeals are decided by panels of three judges working together. The appellant presents legal arguments to the panel, in writing, in a document called a "brief." In the brief, the appellant tries to persuade the judges that the trial court made an error, and that its decision should be reversed.
How do I correct a denied Medicare claim?
File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think Medicare's decision is wrong. You can write on the MSN or attach a separate page.
What is the timely filing limit for Medicare?
12 monthsMedicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
How long does Dwihn have to decide an expedited fast appeal request?
72 hoursDWIHN has 72 hours from the receipt of the expedited MI Health Link first level request to review and make a determination and within 30 calendar days from receipt of the non-expedited MI Health Link first level internal/local appeal request to the enrollee.
Which of the following are reasons a claim may be denied?
Here are the top 5 reasons why claims are denied, and how you can avoid these situations.Pre-Certification or Authorization Was Required, but Not Obtained. ... Claim Form Errors: Patient Data or Diagnosis / Procedure Codes. ... Claim Was Filed After Insurer's Deadline. ... Insufficient Medical Necessity. ... Use of Out-of-Network Provider.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
What is a home health change of care notice?
The “Home Health Change of Care Notice” is a written notice that your home health agency should give you when your home health plan of care is changing because of one of these:
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What happens if you disagree with a decision?
If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you’ll get instructions on how to move to the next level of appeal.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
How long does it take for Medicare to issue a decision?
The Office of Medicare Hearings and Appeals should issue a decision in 90 to 180 days. If you don’t agree with the decision, you can apply for a review by the Medicare Appeals Council.
How long does it take to get a response from Medicare?
You should have a response from the qualified independent contractor within 60 days. If they didn’t decide in your favor, you can ask for a hearing before an administrative law judge or an attorney adjudicator at the Office of Medicare Hearings and Appeals.
What happens if Medicare Appeals Council isn't in your favor?
If the decision of the Medicare Appeals Council isn’t in your favor, you can present your case to a judge in federal district court. The amount of money you’re asking Medicare to pay must meet a set amount to proceed with an appeal in court.
What to do if Medicare won't pay for your care?
If Medicare won’t cover your care, you can start the appeals process then. Pay for your continued care out of pocket.
What is the Medicare number?
your Medicare number (as shown on your Medicare card) the items you want Medicare to pay for and the date you received the service or item. the name of your representative if someone is helping you manage your claim. a detailed explanation of why Medicare should pay for the service, medication, or item.
What happens if Medicare refuses to pay for medical care?
If Medicare refuses to cover care, medication, or equipment that you and your healthcare provider think are medically necessary, you can file an appeal. You may also wish to file an appeal if Medicare decides to charge you with a late enrollment penalty or premium surcharge.
How many levels of appeal are there for Medicare?
There are five levels of appeal for services under original Medicare, and your claim can be heard and reviewed by several different independent organizations. Here are the levels of the appeal process: Level 1. Your appeal is reviewed by the Medicare administrative contractor. Level 2.
What to do if you decide to appeal a health care decision?
If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. If you think your health could be seriously harmed by waiting for a decision about a service, ask the plan for a fast decision.
What happens if my Medicare plan doesn't decide in my favor?
Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.
Whats The Point Of It
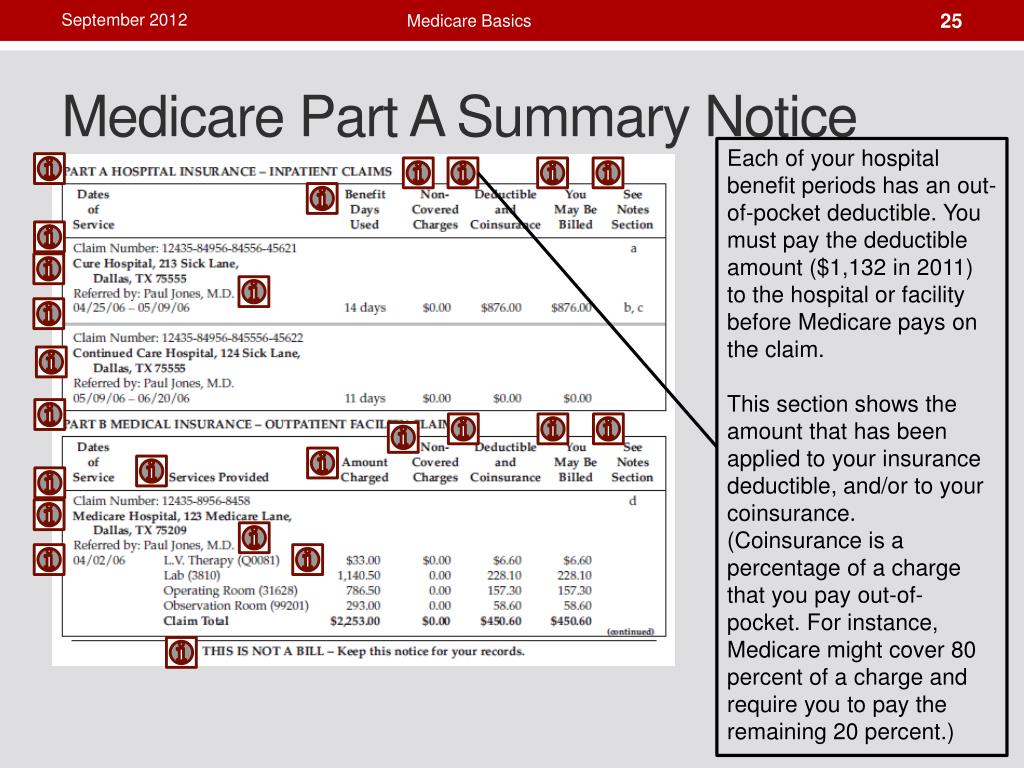
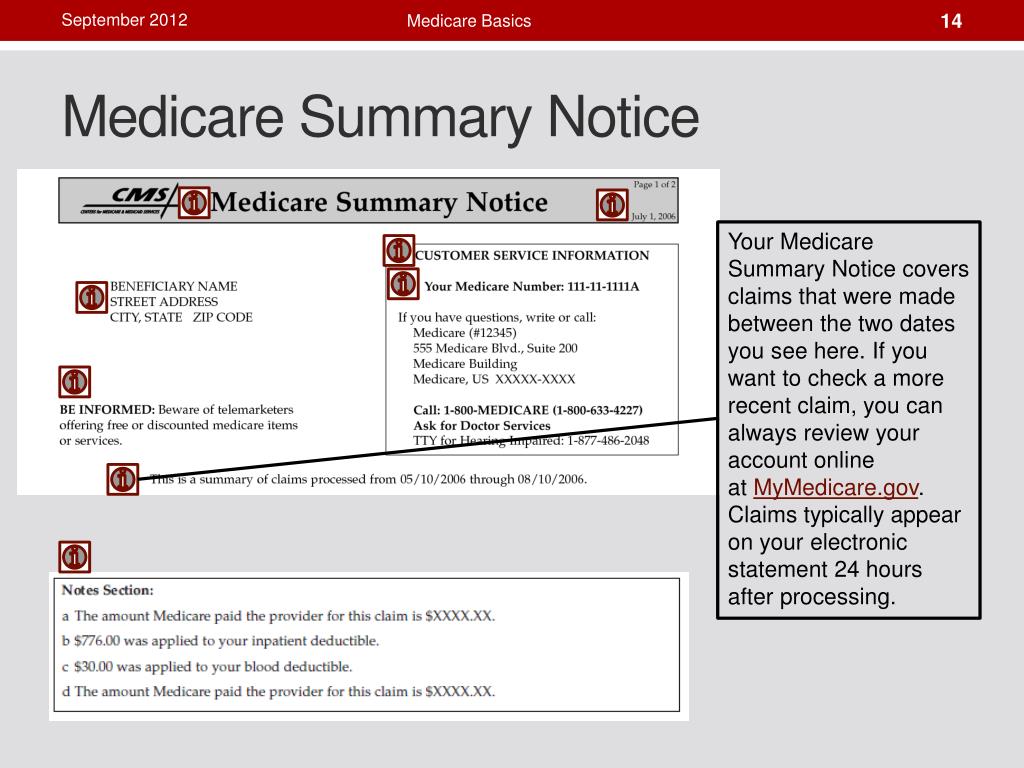
The Medicare Summary Notice helps you see your medical expenses and what Medicares been billed on your behalf. Its a secondary piece of information to put with your bills and other documents as part of your at-home medical records.
How Long Should You Keep Eobs
Experts recommend keeping medical EOBs for a set period of time, but how long depends on the individual circumstances of the patient in question.
How Long Should I Keep The Medicare Summary Notices And Supplemental Insurance Summary Of Benefits Documents I Receive In The Mail
There is no hard and fast rule for saving medical payment records. Certainly, they need to be kept while the medical services that are summarized on the forms are in the process of payment by Medicare and supplemental insurance policies.
How Long Should I Keep Medicare Summary Notices
Holding on to your MSNs for at least 12 months is a good rule of thumb. It allows you to keep track of Medicares payment activity. The main reason to save your MSM for 1 year is because Medicare requires that all claims for health care services need to be filed with Medicare within 12 months after the date of service.
Standardized Notices And Forms
A CMS Form number and Office of Management and Budget approval number, which must appear on the notice, identify OMB-approved, standardized notices and forms. CMS has developed standardized notices and forms for use by plans, providers and enrollees as described below:
What To Do With The Notice
If you have other insurance, check to see if it covers anything that Medicare didnt.
Do You Have To Do Anything Once You Get A Medicare Summary Notice
You should read through it and check for errors or potential fraud. If your list of services doesnt match up with the care you remember receiving, then you should follow up with the Medicare program.