How long do I have to enroll in Medicare after quitting work?
Join a Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. When? Your chance to join lasts 2 full months after the month you lose your creditable coverage or you're notified that your current coverage is no longer creditable, whichever is later. I had drug coverage through a Medicare Cost Plan and I left the plan.
How long does my chance to join a Medicare plan last?
Join a Medicare Advantage Plan or Medicare drug plan. 2 months after your job-based insurance ends. If you want Medicare plan coverage to start when your job-based insurance ends, sign up for Medicare and join a plan before your job-based insurance ends. Buy a Medicare Supplement Insurance (Medigap) policy
When do I have to join a Medicare drug plan?
Feb 11, 2022 · Even though you have up to eight months after leaving your job to sign up for Medicare and avoid a penalty, you could face expensive coverage gaps if you're 65 or older and you choose to continue your employer's coverage through COBRA — a federal law that allows you to keep your benefits temporarily — rather than sign up for Medicare.
When can I enroll in Medicare Part B?
Mar 12, 2019 · During the eight month period after your employer-based coverage ends or the employment ends, whichever occurs first. Can my Medicare Part B Enrollment Start the Day my Work Coverage Ends? Yes, you should be able to enroll in your Medicare Part B a few months in advance and select a future Part B start date.
How do I rejoin Medicare?
To switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins. To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE.
Can my Medicare be reinstated?
You can also ask for reinstatement under the Medicare Good Cause policy. If you prove there's “good cause” (or reason) for not paying premiums — typically an emergency, chronic illness, or other related situation — you'll still have to pay all owed premiums within a specified period of time to resume coverage.Aug 11, 2020
How do I switch back to Original Medicare?
There are three ways you can make the change:Visit your local Social Security Office and ask to be disenrolled from Medicare Advantage;Call 1-800-MEDICARE (1-800-633-4227) and process your disenrollment over the phone; or.Contact your Medicare Advantage insurer directly and request a disenrollment form.
When can I re enroll in Medicare?
When you first get Medicare (Initial Enrollment Periods for Part C & Part D)If you joinYour coverage beginsDuring one of the 3 months before you turn 65The first day of the month you turn 65During the month you turn 65The first day of the month after you ask to join the plan1 more row
Can Medicare coverage be terminated?
You stop paying your premiums If your premiums are still not paid by the date specified on the delinquent notice, your Medicare coverage may be terminated. For private Medicare plans, the guidelines for terminating coverage because of missed payments will depend on the plan's terms and conditions.Feb 19, 2021
Is there a grace period for Medicare premium payments?
Under rules issued by the Centers for Medicare and Medicaid Services (CMS), consumers will get a 90-day grace period to pay their outstanding premiums before insurers are permitted to drop their coverage.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan; if you decide to switch to Medigap, there often are lifetime penalties.
Can I have Original Medicare and Medicare Advantage at the same time?
If you're in a Medicare Advantage Plan (with or without drug coverage), you can switch to another Medicare Advantage Plan (with or without drug coverage). You can drop your Medicare Advantage Plan and return to Original Medicare. You'll also be able to join a Medicare drug plan.
Does getting a Medicare Advantage plan make you lose original Medicare?
If you join a Medicare Advantage Plan, you'll still have Medicare but you'll get most of your Part A and Part B coverage from your Medicare Advantage Plan, not Original Medicare. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What changes are coming to Medicare in 2021?
The Medicare Part B premium is $148.50 per month in 2021, an increase of $3.90 since 2020. The Part B deductible also increased by $5 to $203 in 2021. Medicare Advantage premiums are expected to drop by 11% this year, while beneficiaries now have access to more plan choices than in previous years.Sep 24, 2021
How long before you turn 65 do you apply for Medicare?
3 monthsGenerally, you're first eligible starting 3 months before you turn 65 and ending 3 months after the month you turn 65. If you don't sign up for Part B when you're first eligible, you might have to wait to sign up and go months without coverage. You might also pay a monthly penalty for as long as you have Part B.
What changes are coming to Medicare in 2022?
Changes to Medicare in 2022 include a historic rise in premiums, as well as expanded access to mental health services through telehealth and more affordable options for insulin through prescription drug plans. The average cost of Medicare Advantage plans dropped while access to plans grew.
How does Medicare work with my job-based health insurance when I stop working?
Once you stop working, Medicare will pay first and any retiree coverage or supplemental coverage that works with Medicare will pay second.
When & how do I sign up for Medicare?
You can sign up anytime while you (or your spouse) are still working and you have health insurance through that employer. You also have 8 months after you (or your spouse) stop working to sign up.
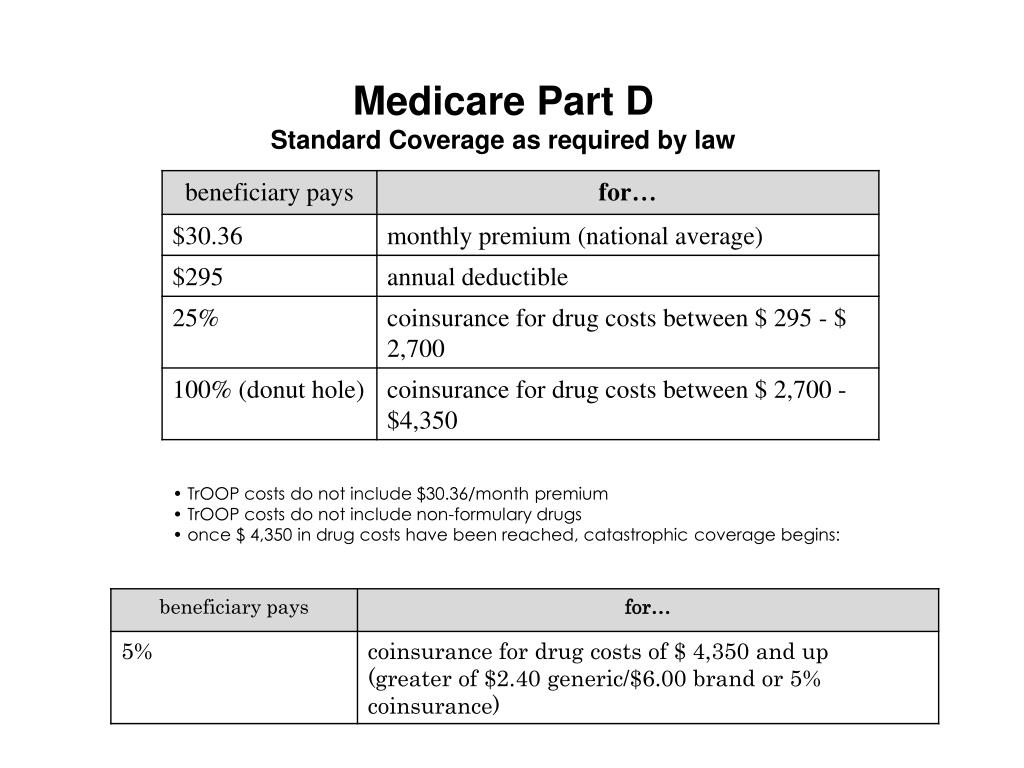
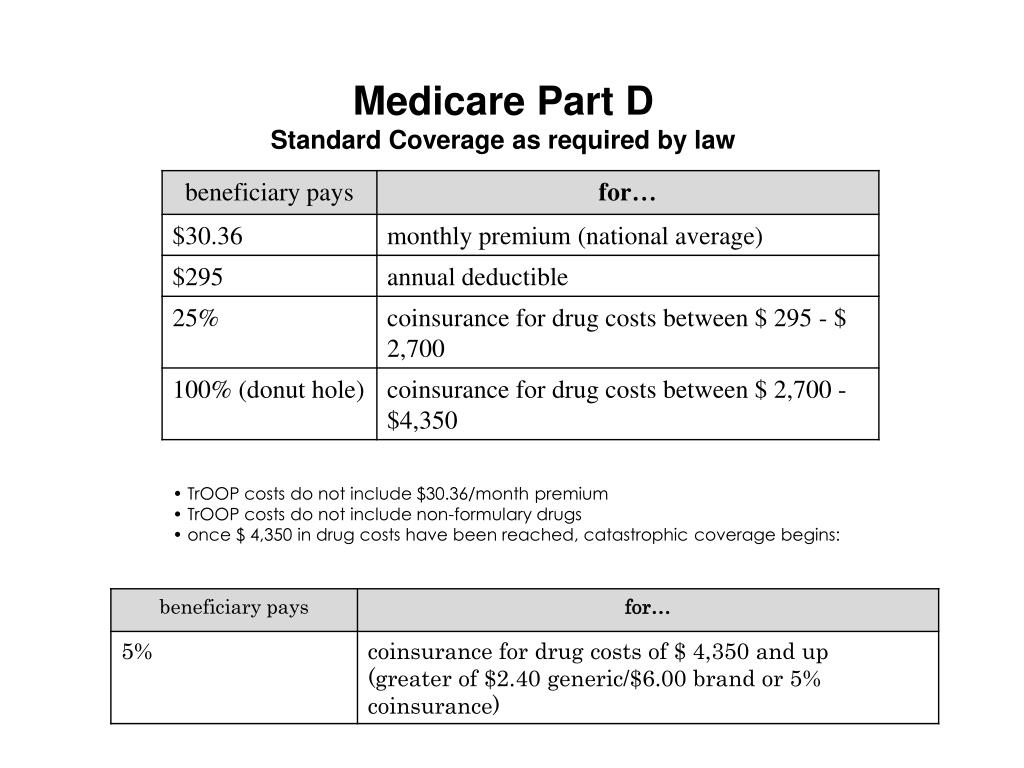
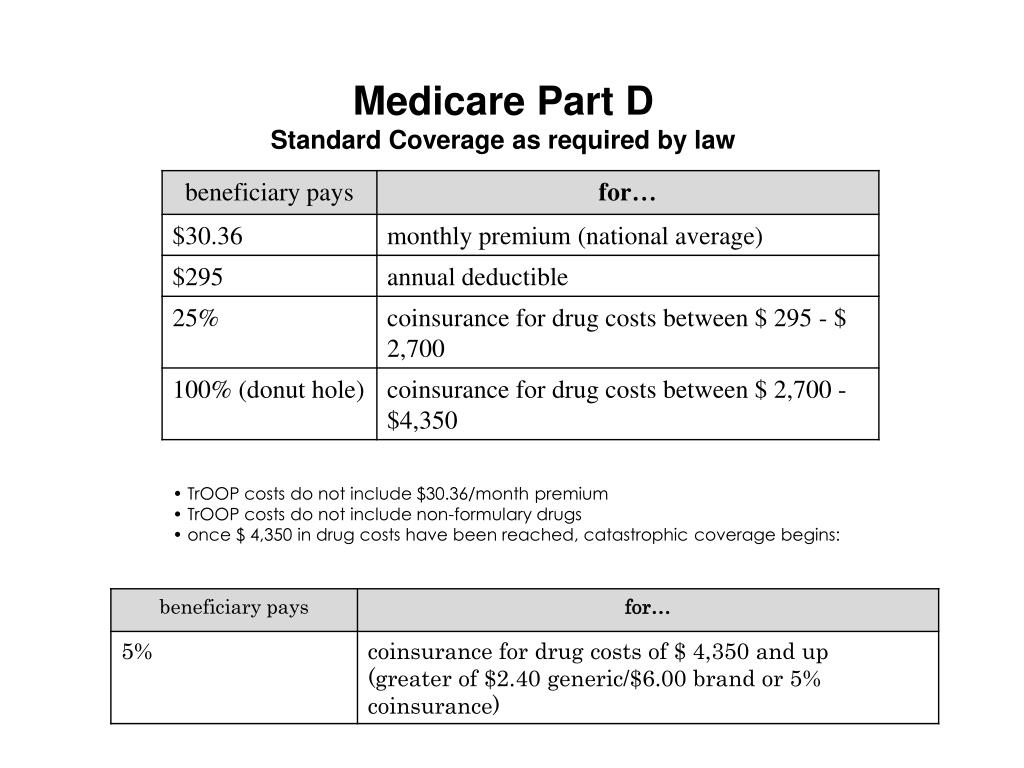
Do I need to get Medicare drug coverage (Part D)?
Prescription drug coverage that provides the same value to Medicare Part D. It could include drug coverage from a current or former employer or union, TRICARE, Indian Health Service, VA, or individual health insurance coverage.
How long do you have to wait to sign up for Medicare?
If you wait more than eight months , you may have to pay a lifetime penalty of 10 percent of the cost of Part B for every 12 months you should have been enrolled in Medicare but were not. You'll also have to wait until the next general enrollment period to sign up for Medicare, which runs from January through March with coverage starting July 1.
What happens if you don't sign up for Medicare?
If you don't sign up for Medicare when you leave your job, you could end up with big coverage gaps and big bills.
When does Medicare become primary?
If you keep your coverage through COBRA, Medicare becomes the primary coverage when you turn 65. This rule also applies to people who work for companies with fewer than 20 employees, with a few exceptions, and those who have retiree health insurance. The rules for coordinating Medicare with COBRA can be confusing because COBRA looks exactly like ...
Who owns Giardini Medicare?
Last year, Joanne Giardini-Russell, owner of Giardini Medicare in Howell, Michigan, which helps people with Medicare issues and supplemental coverage, helped a 70-year-old man who lost his job in late May and had coverage until the end of the month.
Who is Kimberly Lankford?
Kimberly Lankford is a contributing writer who covers personal finance and Medicare. She previously wrote for Kiplinger's Personal Finance magazine, and her articles have also appeared in U.S. News & World Report, The Washington Post and The Boston Globe.
Is Medicare primary or secondary?
But as soon as you leave your job, Medicare becomes your primary coverage and COBRA is secondary. If you haven't signed up for Medicare, you could face expensive coverage gaps. The problem: Even though COBRA coverage looks exactly like your employer's coverage, Medicare rules don't see it that way. As soon as you leave your job ...
Do employers warn about cobra?
Most employers don't warn people about this issue. “Human resources always seems to hand everybody a packet and say, ‘Here's your COBRA,’ and they never bring up the Medicare piece, even though they know how old they are,” Giardini-Russell says.
What is the phone number for Medicare?
If you have an urgent matter or need enrollment assistance, call us at 800-930-7956. By submitting your question here, you agree that a licensed sales representative may respond to you about Medicare Advantage, Prescription Drug, and Medicare Supplement Insurance plans.
How long do you have to enroll in Part B?
There are two main times when you can enroll in part B when you are over 65 and covered by your employer’s insurance: 1 While your work coverage is still active 2 During the eight month period after your employer-based coverage ends or the employment ends, whichever occurs first.
How long does health insurance last after termination?
There is no specific timeframe for how long an employer must keep your health insurance coverage after a job termination. Instead, the business makes that decision. Some companies may end health insurance on the day of termination. Another may wait until the end of the month. Still others may give you a few months of coverage to help ...
How long does it take to get Cobra insurance after termination?
You’ll receive COBRA benefits information after termination. You then have 60 days to decide whether to take the coverage. Coverage is retroactive to your termination. You can take all of those 60 days to decide whether to enroll in a COBRA plan. You’ll have to pay the full 60 days of premiums, whether you enroll the first day or ...
What is the poverty level for medicaid?
In those states, people with incomes up to 138% of the federal poverty level are eligible for Medicaid. Premiums are based on your income. Millions of Americans are eligible for Medicaid and can be a low-cost, comprehensive health plan option if you lose your job.
How long does Cobra last?
COBRA insurance can last longer depending on the situation. Someone with a total disability can keep it for 29 months. Also, other instances can allow people to keep COBRA for 36 months.
How long do you have to pay Cobra insurance?
You’ll have to pay the full 60 days of premiums, whether you enroll the first day or the 60th day once you sign up. You can cancel COBRA at any time within your benefit period, which is usually 18 months.
How long does a short term health insurance last?
These plans can also have high out-of-pocket costs. However, short-term plans can serve as a bridge to future health coverage once. These plans last one year and you can request two extensions. A handful of states don’t allow short-term plans and others have length limitations.
How many employees can you have with Cobra?
COBRA, which stands for the Consolidated Omnibus Budget Reconciliation Act, requires that private employers with at least 20 employees offer COBRA benefits to former employees. One exception is if the employee is fired for “gross misconduct.”. Former employees get to keep the health insurance coverage through COBRA, ...
How long can you keep Medicare after you return to work?
As long as your disabling condition still meets our rules, you can keep your Medicare coverage for at least 8 ½ years after you return to work. (The 8 ½ years includes your nine month trial work period.)
When did Medicare extend to 4 1/2 years?
On October 1, 2000, a new law extended Medicare coverage for an additional 4 1/2 years beyond the current limit. This law is for people who receive Social Security disability benefits and who go to work.
How old do you have to be to get Medicare Part A?
To be eligible for this help, you must be: Under age 65. Continue to have a disabling impairment. Sign up for Premium Hospital Insurance (Part A). Have limited income.
What is special enrollment period?
The special enrollment period is a period of time, during which you may enroll. If you did not enroll during your initial enrollment period because you are covered under a group health plan based on your own current employment or the current employment of any family member.
Does Part B change enrollment?
Yes, this law did not change the enrollment periods. If you did not sign up for Part B when you first could, you can only sign up for it during a general enrollment period (January 1st through March 31st of each year) or a special enrollment period.
Is Medicare a second payer?
Medicare is often the "secondary payer" when you have health care coverage through your work. Notify your Medicare contractor right away. Prompt reporting may prevent an error in payment for your health care services.
How long does it take to reenroll in Medicare?
Special enrollment period — 8 months following a qualifying event. If you qualify, you may be granted this 8-month window to reenroll in original Medicare or change your Medicare coverage after a significant life event, such as a divorce or move. Read on to learn more about how to reenroll in Medicare Part B and what it covers.
What happens if you cancel Medicare Part B?
If you’ve disenrolled from or cancelled your Medicare Part B coverage, you may have to pay a costly late enrollment penalty to reenroll. This is especially true if you have a gap in coverage. If you’re looking to reenroll in Medicare Part B, follow these steps: Go to the Social Security Administration website. Complete the application.
When is Medicare open enrollment?
Medicare open enrollment period — October 15 through December 7. During this time, you can switch from a Medicare Advantage (Part C) plan back to original Medicare. You can also change Part C plans or add, remove, or change a Medicare Part D (prescription drug) plan. Special enrollment period — 8 months following a qualifying event.
How long does it take to enroll in a new health insurance plan?
The initial enrollment period is a 7-month time frame. It includes: the 3 months before the month you turn 65 years old. your birth month. 3 months after your birth month. It’s recommended that you enroll during the first 3 months of initial enrollment so your coverage will begin earlier and you’ll avoid delays.
How long does it take to enroll in Part B?
An 8-month special enrollment period to enroll into Part B insurance also comes into play 1 month after your employment or workplace insurance plan ends. You can even qualify for a special enrollment period if you’re a volunteer in another country. If you miss your initial enrollment and aren’t eligible to sign up during a special enrollment ...
What to do if you didn't sign up for Medicare at 65?
If you did not sign up for any part of Medicare at 65, the best thing to do is either to call Social Security, or to go to your local Social Security office to enroll in Medicare A & B. They’ll ask you when you want Medicare to start, and you can coordinate it with the termination of your group plan as best as you can.
How long do you have to enroll in Medigap?
The enrollment periods for these plans are a bit different than those mentioned above for the MA. For Medigap plans: 1 If you have Part B already, you only have a Medigap Open Enrollment (OE) Period that lasts for 6 months after the time you are both 65 and older and have Part B effective. So if you are retiring after 65 and have had Part B effective for more than 6 months, you’re not in your OE period anymore.#N#This doesn’t mean you can’t get a Medigap plan or have to wait until later to sign up, it just means you’ll have to answer health questions and could possibly be turned down by different insurance companies for different health conditions. However, each Medigap company treats this situation of leaving employer coverage a little bit different, and each company has different health conditions that they will either accept or decline you for, so it’s best to work with an independent insurance agent who can find you the best company to go with depending on your unique situation.#N#Most Medigap companies will allow your plan to start on most days of the month, and not be confined to just starting the first day of the month, as it is with MAs. 2 If you don’t have Part B yet, your Medigap plan can start the day Part B is effective. Most Medigap companies will allow you to enroll in the 6-month period leading up to your Part B effective date.
What is Medicare Supplement?
Medicare Supplement + Prescription Drug Plan (PDP) You can get a Medicare Supplement, which is also known as a Medigap policy, to go along with Medicare Parts A & B. This policy will cover most or all of the Medicare deductibles, coinsurance, and copays. You also can get a PDP to cover your prescriptions.