
When will Medicare extend telehealth coverage?
The changes were included in the final 2021 Medicare Physician Fee Schedule rule that was published in the Federal Register on Dec. 28, 2020.
When will Medicare start covering mental health?
With a late-breaking addition, the FY 2021 Appropriations and Covid-19 Relief legislation enacted into law on Dec. 27, 2020 includes a provision authorizing Medicare coverage of mental health services via telehealth to beneficiaries in their homes regardless of geographic location. This provision adds mental health to the existing Medicare coverage ...
Does CMS cover telehealth?
In addition, CMS will continue to cover services for residents who are supervised by physicians via telehealth until the end of the PHE. Teaching physicians must use real-time audio-visual technology. This coverage will be extended after the PHE only in rural areas.
Does Medicare cover audio only?
Coverage of Audio-only and Some Other Services Not Extended. Medicare will no longer cover audio-only telehealth visits by physicians (99441-99443) and non-physician practitioners (98966-98968) after the PHE ends. CMS explained that its longstanding interpretation of the statutory provision that authorizes coverage of telehealth refers use ...
What is telehealth in Medicare?
Medicare telehealth services include office visits, psychotherapy, consultations, and certain other medical or health services that are provided by a doctor or other health care provider who’s located elsewhere using interactive 2-way real-time audio and video technology.
When can telehealth be used?
Due to the Coronavirus (COVID-19) Public Health Emergency, doctors and other health care providers can use telehealth services to treat COVID-19 (and for other medically reasonable purposes) from offices, hospitals, and places of residence (like homes, nursing homes, and assisted living facilities) as of March 6, 2020.
How to find out how much a test is?
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like: 1 Other insurance you may have 2 How much your doctor charges 3 Whether your doctor accepts assignment 4 The type of facility 5 Where you get your test, item, or service 6 The type of provider
Does Medicare offer telehealth?
Starting in 2020, Medicare Advantage Plans may offer more telehealth benefits than Original Medicare. These benefits can be available in a variety of places, and you can use them at home instead of going to a health care facility. Check with your plan to see what additional telehealth benefits it may offer.
What is CTBS code?
On the other hand, CTBS codes represent brief communication services conducted over different types of technology to help avoid unnecessary office visits and slow the spread of COVID-19.
What is the ASHA code of ethics?
ASHA guidelines state that the use of telehealth must be equivalent to the quality of in-person services and must adhere to the ASHA Code of Ethics, audiology or speech-language pathology scope of practice , state and federal laws, and ASHA policy.
Can SLPs accept Medicare telehealth?
Medicare’s temporary expansion of telehealth services means that audiologists and SLPs may no longer enter into a private pay arrangement with Medicare beneficiaries for those services that are now included on Medicare’s telehealth list. For codes that are not authorized telehealth services, audiologists and SLPs can continue to accept private payment from Medicare beneficiaries.
Can telehealth be used for established patients?
Although Medicare only allows established patients to receive telehealth services, CMS has said it will not conduct audits to ensure that a prior relationship existed during the public health emergency. This means that clinicians may provide telehealth services to both new and established patients. Clinicians should consider state practice acts or other local laws and regulations before beginning services with new patients. Clinicians may be required to evaluate new patients before providing clinical recommendations or treatment.
Does Medicare cover telehealth?
Medicare is precluded by federal law from covering telehealth services under the Part A home health benefit . In its home health fact sheet [PDF], CMS states that only in-person services can be reported via the home health claim even when the home health plan of care is developed or updated to include the use of telecommunication technology. As noted above, home health agencies may provide telehealth services to Medicare beneficiaries in their homes, but only when the patient is not under an established Medicare Part A home health plan of care.
Can SNFs provide telehealth?
Medicare officials have stated that services provided via audiovisual equipment—such as a smartphone or platforms like FaceTime or Skype— in the same building as the patient or through the patient’s window are allowed but are considered in-person services and not telehealth services. Documentation and billing should follow the same guidelines as services provided in person.
Do telehealth providers report the same CPT codes?
Audiologists and SLPs providing telehealth services should report the same CPT codes and follow the same coding guidelines as they would for in-person services, including same-day billing rules and time requirements. For example, a brief check-in via telecommunication technology should not be reported with an evaluation or treatment CPT code (such as 92507 or 92601) and is not considered a Medicare telehealth service.
What is telehealth in Medicare?
Telehealth, the provision of health care services to patients from providers who are not at the same location, has experienced a rapid escalation in use during the COVID-19 pandemic, among both privately-insured patients and Medicare beneficiaries. Before the pandemic, coverage of telehealth services under traditional Medicare was limited ...
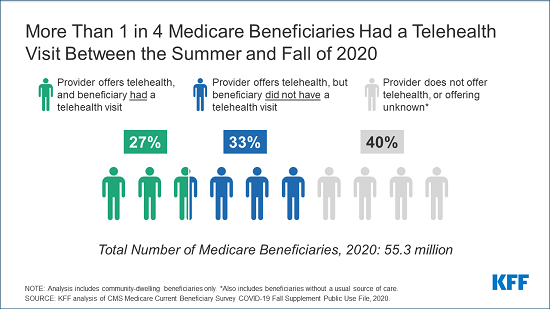
How many Medicare beneficiaries are using telehealth?
Use of Telehealth. Among the two-thirds of Medicare beneficiaries with a usual source of care who reported in the Fall of 2020 that their usual provider offers telehealth during the pandemic (33.6 million beneficiaries), nearly half (45%, or 14.9 million beneficiaries) reported having a telehealth visit since July 2020.
How many services does Medicare cover?
Before the public health emergency, traditional Medicare covered about 100 services that could be administered through telehealth, including office visits, psychotherapy, and preventive health screenings, among other services. During the public health emergency, the list of allowable telehealth services covered under traditional Medicare expanded ...
What is the deductible for telehealth in 2021?
Medicare covers telehealth services under Part B, so beneficiaries in traditional Medicare who use these benefits are subject to the Part B deductible of $203 in 2021 and 20% coinsurance.
Can you use a phone for telehealth?
Under Medicare’s existing telehealth benefit, a telehealth visit must be conducted with two-way audio/video communications and the use of smartphones or audio-only telephone s in lieu of video is not permitted .
Does Medicare cover virtual check ins?
Separate from Medicare’s coverage of telehealth services, traditional Medicare covers brief, “ virtual check-ins ” (also called “brief communication technology-based services”) via telephone or captured video image, and E-visits for all beneficiaries, regardless of whether they live in a rural area .
Can you receive telehealth in your home?
During the public health emergency, beneficiaries in any geographic area can receive telehealth services, and can receive these services in their own home, rather than needing to travel to a “distant site” (i.e., a health care setting).
Medicare Telehealth Services Post-COVID
Telemedicine and digital health technology is becoming an established part of medical practice and is very likely to persist after the COVID-19 pandemic. According to CMS data, before the Public Health Emergency (PHE), 15,000 Medicare patients each week received a telemedicine service.
No New Telehealth Services Proposed For 2022
CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. Unfortunately, none of the requests met CMS’ criteria for permanent addition to the Medicare telehealth services list. The requested services are listed in the table below.
Extended Timeframe for Category 3 Temporary Codes
Last year, CMS created a set of “ Category 3 ” codes to designate telehealth services covered temporarily during the PHE, but for which CMS has not yet developed evidence sufficient to meet the requirements for permanent coverage.
New Virtual Check-In Code Made Permanent
Communication Technology-Based Services (CTBS) are brief communication services conducted over different types of technology to avoid unnecessary in-person office visits. These services, by definition, are virtual and do not replace services that would normally be performed in-person.
Should CMS Continue To Allow Direct Supervision via Telehealth?
CMS seeks comments on whether to adopt a policy to permanently allow provision of direct supervision via telehealth.
How to Submit Comments on the Proposed Rule
Providers, technology companies, and virtual care entrepreneurs interested in telemedicine should consider providing comments to the proposed rule. CMS is soliciting comments until 5:00 p.m. on September 13, 2021. Anyone may submit comments – anonymously or otherwise – via electronic submission at this link.
How many licensed counselors are there in Medicare?
By passing the Mental Health Access Improvement Act, and allowing the well over 100,000 licensed counselors and marriage and family therapists to render services to Medicare beneficiaries, legislators have an opportunity to create significant gains in access to mental health care for millions of Americans.
How long should a letter be?
Keep it brief: Letters should never be longer than one page . State who you are and what you want upfront: In the first paragraph, tell your legislators that you are a constituent and identify the issue about which you are writing. Address your letter correctly. Be sure you use the correct address and salutation.
Can a counselor be billed by Medicare?
Under the current Medicare law, counselors continue to be excluded from being reimbursed by Medicare for providing counseling services. Only psychiatrists, psychologists, clinical social workers, and psychiatric nurses are allowed to bill Medicare for counseling services provided to Medicare beneficiaries. Although many attempts to pass Medicare laws to include counselors as Medicare providers have been attempted over the years, none has been successful. On January 21, 2021, however, Rep. Mike Thompson (CA- 05) and Rep. John Kato (NY-24) reintroduced the Mental Health Access Improvement Act, a bipartisan bill that would allow counselors and marriage and family therapists to become Medicare providers. See
Can seniors qualify for Medicare?
They may want therapy to help cope with the very same physical disabilities that prohibit them from being able to go to a provider’s office . (Click here for more information on helping disabled clients via telehealth). Other clients may also have pre-existing conditions that make them more vulnerable to contracting the virus if they must leave their homes to attend an in-person appointment.
Is section 123 illogical?
While nearly all of the changes that have been made by the federal and state governments to expand telehealth as a result of the pandemic have been helpful in making telehealth more widely available to deliver medical care, section 123 appears to be illogical and care blocking action to behavioral healthcare.
Does Medicare require telehealth visits?
New Medicare Law Requires In-Person Visit for Telehealth Coverage. In December 2020, the Consolidated Appropriations Act of 2020 , section 123 includes language that requires behavioral health providers to have seen their client in person during the prior six months before a telehealth visit will be covered by Medicare.
What is the CPT code for Telehealth?
Medicare increased payments for certain evaluation and management visits provided by phone for the duration of the COVID-19 public health emergency: Telehealth CPT codes 99441 (5-10 minutes), 99442 (11-20 minutes), and 99443 (20-30 minutes)
How much is Medicare reimbursement for 2020?
Reimbursements match similar in-person services, increasing from about $14-$41 to about $60-$137, retroactive to March 1, 2020. In addition, Medicare is temporarily waiving the audio-video requirement for many telehealth services during the COVID-19 public health emergency. Codes that have audio-only waivers during the public health emergency are ...
Does Medicare cover telehealth?
Telehealth codes covered by Medicare. Medicare added over one hundred CPT and HCPCS codes to the telehealth services list for the duration of the COVID-19 public health emergency. Telehealth visits billed to Medicare are paid at the same Medicare Fee-for-Service (FFS) rate as an in-person visit during the COVID-19 public health emergency.
Who is the administrator of the CMS?
Seema Verma, administrator of the CMS, was asked in a May 26 call with reporters about the possibility that the telehealth waivers CMS has provided during the ongoing public health emergency (PHE) would be made permanent under a May 19 executive order.
Does CMS have telehealth waivers?
CMS has issued a range of telehealth waivers that apply to various components of providing and paying for such services, including: Waiving limitations on the types of healthcare professionals eligible to offer telehealth services.
Is telehealth waiver permanent?
Medicare is reviewing whether to make telehealth waivers permanent. Waivers have expanded provider eligibility lists and available payment from Medicare. Hospitals are asking Congress to expand other federal telehealth programs.
Introduction
Key Findings
- Among the vast majority of Medicare beneficiaries with a usual source of care (95%), such as a doctor or other health professional, or a clinic, nearly two-thirds (64% or 33.6 million) say that the...
- Among the 33.6 million Medicare beneficiaries with a usual source of care who reported that their provider currently offers telehealth appointments, nearly half (45%) said they had a teleh…
- Among the vast majority of Medicare beneficiaries with a usual source of care (95%), such as a doctor or other health professional, or a clinic, nearly two-thirds (64% or 33.6 million) say that the...
- Among the 33.6 million Medicare beneficiaries with a usual source of care who reported that their provider currently offers telehealth appointments, nearly half (45%) said they had a telehealth vis...
Who Has Used Telehealth Services During The Covid-19 Public Health Emergency?
- Awareness of Telehealth Availability
As of Fall 2020, six months after the expansion of telehealth benefits in traditional Medicare for the COVID-19 pandemic, nearly two-thirds of community-dwelling Medicare beneficiaries who say they have a usual source of care (64%, or 33.6 million beneficiaries), such as a doctor or health p… - Use of Telehealth
Among the two-thirds of Medicare beneficiaries with a usual source of care who reported in the Fall of 2020 that their usual provider offers telehealth during the pandemic (33.6 million beneficiaries), nearly half (45%, or 14.9 million beneficiaries) reported having a telehealth visit si…
How Did Beneficiaries Access Telehealth Services?
- Among Medicare beneficiaries with a usual source of care whose provider offers telehealth appointments, the majority of those who had a telehealth visit since July 2020 accessed the service by telephone (56%), compared to 28% who reported having a telehealth visit by video and 16% who used both telephone and video (Figure 5; Table3). This may be related to the fact that …