How long does Medicare pay for hospital costs?
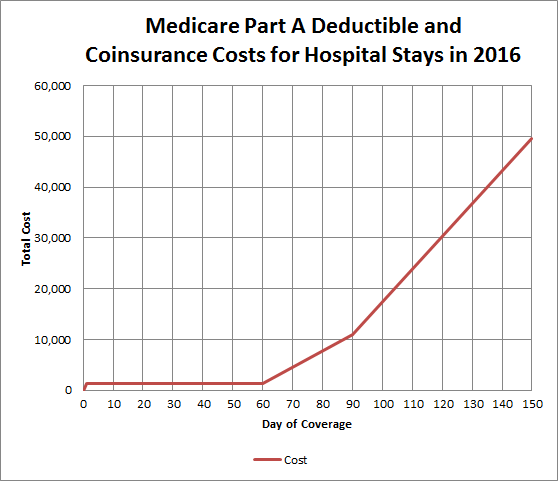
Once the deductible is paid fully, Medicare will cover the remainder of hospital care costs for up to 60 days after being admitted. If you need to stay longer than 60 days within the same benefit period, you’ll be required to pay a daily coinsurance.
How long does Medicare pay for inpatient rehab?
How long does Medicare pay for rehab? Medicare Part A covers 100 days in a skilled nursing facility with some coinsurance costs. After day 100 of an inpatient SNF stay, you are responsible for all costs. Medicare Part A will also cover 90 days of inpatient hospital rehab with some coinsurance costs after you meet your Part A deductible.
Does Medicare pay for hospice care?
Medicare recipients who have Original Medicare Part A, are eligible for the hospice benefit if they have certification from their physician that their life expectancy is no more than six months. Patients must also sign a statement saying they choose hospice care rather than curative treatment for their illness.
How long can you stay out of the hospital on Medicare?
Once you have exhausted all of your lifetime reserve days, you will be responsible for all hospital costs for any stay longer than 90 days. When you have been out of the hospital for 60 days in a row, your benefit period ends and your Part A deductible will reset the next time you are admitted.

Which part of Medicare covers hospital stays up to 60 days?
Medicare Part AWhat Are Medicare Lifetime Reserve Days? Medicare Part A pays for inpatient hospital care. During each benefit period, Medicare covers up to 90 days of inpatient hospitalization. After 90 days, Medicare gives you 60 additional days of inpatient hospital care to use during your lifetime.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
How long can you stay in ICU on Medicare?
Original Medicare covers up to 90 days of inpatient hospital care each benefit period. You also have an additional 60 days of coverage, called lifetime reserve days.
What happens when your Medicare runs out?
These days are nonrenewable, meaning you will not get them back when you become eligible for another benefit period. Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Does Medicare cover hospital stay?
Medicare generally covers 100% of your medical expenses if you are admitted as a public patient in a public hospital. As a public patient, you generally won't be able to choose your own doctor or choose the day that you are admitted to hospital.
Can Medicare kick you out of hospital?
Medicare covers 90 days of hospitalization per illness (plus a 60-day "lifetime reserve"). However, if you are admitted to a hospital as a Medicare patient, the hospital may try to discharge you before you are ready. While the hospital can't force you to leave, it can begin charging you for services.
How long does Medicare cover a ventilator?
If you have Medicare and use oxygen, you can rent oxygen equipment from a supplier for as long as you have a medical need, but payments for the equipment stop after 36 months of continuous use. After 36 months, your supplier must continue to provide oxygen equipment and related supplies for an additional 24 months.
What is the 3 day rule for Medicare?
The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay. The 3-consecutive-day count doesn't include the discharge day or pre-admission time spent in the Emergency Room (ER) or outpatient observation.
How many days will Medicare pay 100% of the covered costs of care in a skilled nursing care facility?
100 daysMedicare covers up to 100 days of care in a skilled nursing facility (SNF) for each benefit period if all of Medicare's requirements are met, including your need of daily skilled nursing care with 3 days of prior hospitalization. Medicare pays 100% of the first 20 days of a covered SNF stay.
Does Medicare cover ICU costs?
(Medicare will pay for a private room only if it is "medically necessary.") all meals. regular nursing services. operating room, intensive care unit, or coronary care unit charges.
What is the cap for Medicare?
The resulting maximum Social Security tax for 2020 is $8,537.40. There is no limit on the amount of earnings subject to Medicare (hospital insurance) tax....2020 Social Security and Medicare Tax Withholding Rates and Limits.Tax2019 Limit2020 LimitMedicare liabilityNo limitNo limit3 more rows
Does Medicare Cover Hospice?
Yes, Medicare will cover hospice, if you meet qualifications to receive the benefits. These include:
How Long Will Medicare Pay for Hospice?
Hospice care is for patients who have a life expectancy of six months or less given the current progression of their illness. Typically, Medicare’s initial hospice benefit is broken down into two 90-day benefit periods. If hospice care is still needed after six months, patients can be re-certified for an unlimited number of 60-day benefits.
Does Medicare pay for hospice in a skilled nursing facility?
Yes, it will. However, it’s important to remember that Medicare does not cover room and board associated with living full-time in a skilled nursing facility or nursing home.
How Can I Maximize My Medicare Benefits?
There are several things you must know to help you maximize your Medicare benefits. These include:
Lower Cape Fear LifeCare Never Refuses Care Based on Ability to Pay
As a non-profit hospice, we understand the difference that proper care can make in the lives of our patients and their families. That’s why Lower Cape Fear LifeCare never refuses anyone care, regardless of their ability to pay.
How long does Medicare cover hospital stays?
Medicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual’s reserve days. Medicare provides 60 lifetime reserve days. The reserve days provide coverage after 90 days, but coinsurance costs still apply.
How long does a psychiatric hospital stay in Medicare?
Medicare provides the same fee structure for general hospital care and psychiatric hospital care, with one exception: It limits the coverage of inpatient psychiatric hospital care to 190 days in a lifetime.
What is the best Medicare plan?
We may use a few terms in this piece that can be helpful to understand when selecting the best insurance plan: 1 Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments. 2 Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. 3 Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is covered by Medicare before a hospital stay?
This coverage includes: general nursing care. a semi-private room. hospital equipment and services. meals. medication that is part of inpatient hospital treatment.
How much does Medicare pay for skilled nursing in 2020?
Others, who may have long-term cognitive or physical conditions, require ongoing supervision and care. Medicare Part A coverage for care at a skilled nursing facility in 2020 involves: Day 1–20: The patient spends $0 per benefit period after meeting the deductible. Days 21–100: The patient pays $176 per day.
What is Medicare Part A?
Medicare Part A. Out-of-pocket expenses. Length of stay. Eligible facilities. Reducing costs. Summary. Medicare is the federal health insurance program for adults aged 65 and older, as well as for some younger people. Medicare pays for inpatient hospital stays of a certain length. Medicare covers the first 60 days of a hospital stay after ...
How much is the deductible for Medicare 2020?
This amount changes each year. For 2020, the Medicare Part A deductible is $1,408 for each benefit period.
What are Medicare covered services?
Medicare-covered hospital services include: Semi-private rooms. Meals. General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
How many days in a lifetime is mental health care?
Things to know. Inpatient mental health care in a psychiatric hospital is limited to 190 days in a lifetime.
What is an inpatient hospital?
Inpatient hospital care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
What does Medicare Part B cover?
If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital. This doesn't include: Private-duty nursing. Private room (unless Medically necessary ) Television and phone in your room (if there's a separate charge for these items)
How many days can you use Medicare in one hospital visit?
Medicare provides an additional 60 days of coverage beyond the 90 days of covered inpatient care within a benefit period. These 60 days are known as lifetime reserve days. Lifetime reserve days can be used only once, but they don’t have to be used all in one hospital visit.
How long does Medicare Part A deductible last?
Unlike some deductibles, the Medicare Part A deductible applies to each benefit period. This means it applies to the length of time you’ve been admitted into the hospital through 60 consecutive days after you’ve been out of the hospital.
What is the Medicare deductible for 2020?
Even with insurance, you’ll still have to pay a portion of the hospital bill, along with premiums, deductibles, and other costs that are adjusted every year. In 2020, the Medicare Part A deductible is $1,408 per benefit period.
How much does Medicare Part A cost in 2020?
In 2020, the Medicare Part A deductible is $1,408 per benefit period.
What is Medicare Part A?
Medicare Part A, the first part of original Medicare, is hospital insurance. It typically covers inpatient surgeries, bloodwork and diagnostics, and hospital stays. If admitted into a hospital, Medicare Part A will help pay for:
How long do you have to work to qualify for Medicare Part A?
To be eligible, you’ll need to have worked for 40 quarters, or 10 years, and paid Medicare taxes during that time.
Does Medicare cover hospital stays?
Medicare Part A can help provide coverage for hospital stays. You’ll still be responsible for deductibles and coinsurance. A stay at the hospital can make for one hefty bill. Without insurance, a single night there could cost thousands of dollars. Having insurance can help reduce that cost.
How long does an acute care hospital stay?
Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days. Most patients are transferred from an intensive or critical care unit. Services provided include comprehensive rehabilitation, respiratory therapy, head trauma treatment, and pain management. .
How long does it take to get discharged from a long term care hospital?
You’re transferred to a long-term care hospital directly from an acute care hospital. You’re admitted to a long-term care hospital within 60 days of being discharged from a hospital.
What is Medicare Part A?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. covers the cost of long-term care in a. long-term care hospital. Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days.
When does the benefit period end?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. ...
Do you have to pay a deductible for long term care?
Each day after the lifetime reserve days: All costs. *You don’t have to pay a deductible for care you get in the long-term care hospital if you were already charged a deductible for care you got in a prior hospitalization within the same benefit period.
How many days do you have to be in hospital to qualify for Medicare?
Having days left in your benefit period. Having a qualifying hospital stay of three inpatient days. Your doctor determining that you need daily skilled care.
How long does Medicare cover nursing home care?
What parts of nursing home care does Medicare cover? Medicare covers up to 100 days at a skilled nursing facility. Medicare Part A and Part B cover skilled nursing facility stays of up to 100 days for older people who require care from people with medical skills, such as sterile bandage changes.
What is covered by Medicare Advantage?
Some of the specific things covered by Medicare include: A semiprivate room. Meals. Skilled nursing care. Physical and occupational therapy. Medical social services. Medications. Medical supplies and equipment. However, if you have a Medicare Advantage Plan, it’s possible that the plan covers nursing home care.
How much does a nursing home cost?
On average, annual costs for nursing homes fall between $90,000 and $110,000, depending on whether you have a private or semi-private room. This can burn through your personal funds surprisingly quickly. It’s best to pair your personal funds with other financial aid to help you afford nursing home care.
How long does functional mobility insurance last?
Most policies will also require you to pay out of pocket for a predetermined amount of time, usually between 30 and 90 days, before coverage kicks in.
Does Medicare cover dementia care?
Does Medicare cover nursing home care for dementia? Medicare only ever covers the first 100 days in a nursing home, so nursing home coverage is not significantly different for people with dementia. Medicaid can help cover memory care units and nursing home stays beyond 100 days, though. Can older people rely on Medicare to cover nursing home costs? ...
Does Medicare cover nursing home room and board?
It also doesn’t cover room and board for any long-term nursing home stay, including hospice care or the cost of a private room. Lastly, Medicare won’t cover your skilled nursing facility stay if it’s not in an approved facility, so it’s important to know what institutions it has approved in your area.
How long does Medicare cover SNF?
After day 100 of an inpatient SNF stay, you are responsible for all costs. Medicare Part A will also cover 90 days of inpatient hospital rehab with some coinsurance costs after you meet your Part A deductible. Beginning on day 91, you will begin to tap into your “lifetime reserve days.".
How long do you have to be out of the hospital to get a deductible?
When you have been out of the hospital for 60 days in a row, your benefit period ends and your Part A deductible will reset the next time you are admitted.
How long does rehab last in a skilled nursing facility?
When you enter a skilled nursing facility, your stay (including any rehab services) will typically be covered in full for the first 20 days of each benefit period (after you meet your Medicare Part A deductible). Days 21 to 100 of your stay will require a coinsurance ...
How much is Medicare Part A deductible for 2021?
In 2021, the Medicare Part A deductible is $1,484 per benefit period. A benefit period begins the day you are admitted to the hospital. Once you have reached the deductible, Medicare will then cover your stay in full for the first 60 days. You could potentially experience more than one benefit period in a year.
How much is coinsurance for inpatient care in 2021?
If you continue receiving inpatient care after 60 days, you will be responsible for a coinsurance payment of $371 per day (in 2021) until day 90. Beginning on day 91, you will begin to tap into your “lifetime reserve days,” for which a daily coinsurance of $742 is required in 2021. You have a total of 60 lifetime reserve days.
What day do you get your lifetime reserve days?
Beginning on day 91 , you will begin to tap into your “lifetime reserve days.". You may have to undergo some rehab in a hospital after a surgery, injury, stroke or other medical event. The rehab may take place in a designated section of a hospital or in a stand-alone rehabilitation facility. Medicare Part A provides coverage for inpatient care ...
Does Medicare cover outpatient treatment?
Medicare Part B may cover outpatient treatment services as part of a partial hospitalization program (PHP), if your doctor certifies that you need at least 20 hours of therapeutic services per week.
