Medicare has a new initiative that will cover up to eight over-the-counter COVID-19 tests each calendar month, at no cost to you. Who’s eligible? Medicare will cover these tests if you have Part B, including those enrolled in a Medicare Advantage plan.
Full Answer
How much does Medicare Part a cost?
Medicare costs at a glance. Most people don't pay a monthly premium for Part A (sometimes called " premium-free Part A "). If you buy Part A, you'll pay up to $437 each month. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $437. If you paid Medicare taxes for 30-39 quarters, the standard Part A premium is $240.
What does Medicare Part a cover?
What Part A covers. Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
What does Medicare Part A&Part B cover?
What Medicare health plans cover. Medicare health plans include Medicare Advantage, Medical Savings Account (MSA), Medicare Cost plans, PACE, MTM. Preventive & screening services. Part B covers many preventive services. What's not covered by Part A & Part B. Learn about what items and services aren't covered by Medicare Part A or Part B.
What is a Medicare pre-payment amount?
The amount you must pay for health care or prescriptions before Original Medicare, your Medicare Advantage Plan, your Medicare drug plan, or your other insurance begins to pay. applies. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid.
How often can you get a wheelchair through Medicare?
If your equipment is worn out, Medicare will only replace it if you have had the item in your possession for its whole lifetime. An item's lifetime depends on the type of equipment but, in the context of getting a replacement, it is never less than five years from the date that you began using the equipment.
How Much Does Medicare pay for a rollator?
In most cases, Medicare will pay 80% of the rolling walker costs. Be sure to check your supplemental insurance policy for the details of your plan that will cover whatever Medicare does not –minimizing as much out of pocket expense as possible. Walkers covered by Medicare include regular walkers and the rollator type.
How do I get my $144 back from Medicare?
Even though you're paying less for the monthly premium, you don't technically get money back. Instead, you just pay the reduced amount and are saving the amount you'd normally pay. If your premium comes out of your Social Security check, your payment will reflect the lower amount.
How many days per year does Medicare cover?
Medicare covers care in a SNF up to 100 days in a benefit period if you continue to meet Medicare's requirements.
Does Medicare pay for more than one walker?
Q: Will Medicare cover the cost of wheelchairs and walkers? A: Yes. Medicare Part B covers a portion of the cost for medically-necessary wheelchairs, walkers and other in-home medical equipment.
Does Medicare pay for a wheeled walker with a seat?
Does Medicare Cover Walkers With Seats (e.g. Rollators)? Generally, yes, but you can expect to pay about $50 more than you would pay for a regular walker. A walker with a seat has wheels too and is known as a rollator. There are several types of rollators, so you will want to choose one that is specific to your needs.
What is the $16 728 Social Security secret?
1:266:46My Review: Motley Fool's $16,728 Social Security Bonus - YouTubeYouTubeStart of suggested clipEnd of suggested clipIf you've read any of their articles you've probably seen this it says the sixteen thousand sevenMoreIf you've read any of their articles you've probably seen this it says the sixteen thousand seven hundred and twenty eight dollar social security bonus most retirees completely overlook.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Who is eligible for Medicare Part B reimbursement?
1. How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B.
What is the 3 day rule for Medicare?
The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay. The 3-consecutive-day count doesn't include the discharge day or pre-admission time spent in the Emergency Room (ER) or outpatient observation.
What happens when you run out of Medicare days?
Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period. To be eligible for a new benefit period, and additional days of inpatient coverage, you must remain out of the hospital or SNF for 60 days in a row.
Can you run out of Medicare?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
Medicare Allowables
Below is a list of current Medicare allowable for ostomy supplies, urological supplies and wound care supplies . If you have any questions, reach out to our team today! We’re happy to help.
Wound Care Allowables
PLEASE NOTE: AMOUNT SENT IS BASED ON CHANGING FREQUENCY, NUMBER OF WOUNDS, AND DOCTORS ORDERS.
A6196 HCPCS Code Description
The Healthcare Common Procedure Coding System (HCPCS) is a collection of codes that represent procedures, supplies, products and services which may be provided to Medicare beneficiaries and to individuals enrolled in private health insurance programs.
A6196 HCPCS Code Pricing Indicators
Code used to identify instances where a procedure could be priced under multiple methodologies.
A6196 HCPCS Code Manual Reference Section Numbers
Number identifying the reference section of the coverage issues manual.
A6196 HCPCS Code Lab Certifications
Code used to classify laboratory procedures according to the specialty certification categories listed by CMS. Any generally certified laboratory (e.g., 100) may perform any of the tests in its subgroups (e.g., 110, 120, etc.).
A6196 HCPCS Code Cross Reference Codes
An explicit reference crosswalking a deleted code or a code that is not valid for Medicare to a valid current code (or range of codes).
A6196 HCPCS Code Coverage, Payment Groups, Payment Policy Indicators
The 'YY' indicator represents that this procedure is approved to be performed in an ambulatory surgical center. You must access the ASC tables on the mainframe or CMS website to get the dollar amounts.
A6196 HCPCS Code Type Of Service Codes
The carrier assigned CMS type of service which describes the particular kind (s) of service represented by the procedure code.
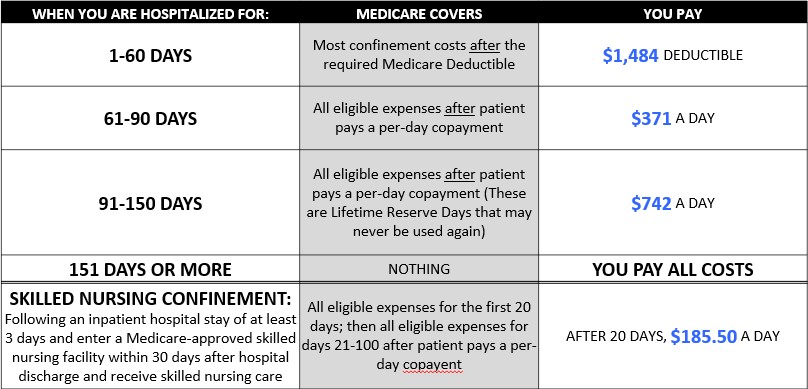
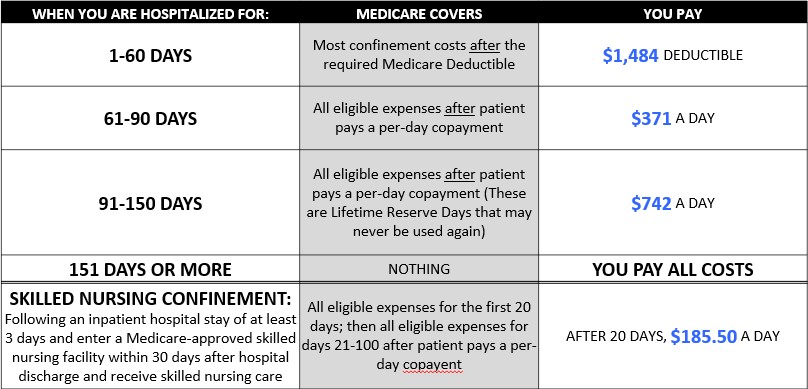
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
What is the HCPCS code for 2021?
A6196 is a valid 2021 HCPCS code for Alginate or other fiber gelling dressing, wound cover, sterile, pad size 16 sq. in. or less, each dressing or just “ Alginate dressing <=16 sq in ” for short, used in Surgical dressings or other medical supplies .
What is a modifier in a report?
Modifiers may be used to indicate to the recipient of a report that: A service or procedure has both a professional and technical component. A service or procedure was performed by more than one physician and/or in more than one location. A service or procedure has been increased or reduced. Only part of a service was performed.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.