Where to get help in making a Medicare appeal?
an appeal no matter how you get your Medicare. For more information, visit Medicare.gov/appeals, or call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. Can someone file an appeal for me? If you want help filing an appeal, you can appoint a representative. Your representative can help you with the appeals steps explained
Who can assist with a Medicare appeal?
You can get help filing your appeal from your doctor, family members, attorneys, or advocates. As a Medicare beneficiary, you have certain rights. One of them is the right to appeal a Medicare decision that you think is unfair or will jeopardize your health. The Medicare appeals process has several levels.
When can I file an appeal to a Medicare claim?
You must file this appeal within 180 days of getting the denial of your first appeal. Medicare Advantage. With Medicare Advantage plans, you're dealing not only with Medicare, but with the rules set by the private insurance company that runs your program.
How to appeal a higher Medicare Part B premium?
There are 7 qualifying life-changing events:
- Death of spouse
- Marriage
- Divorce or annulment
- Work reduction
- Work stoppage
- Loss of income from income producing property
- Loss or reduction of certain kinds of pension income
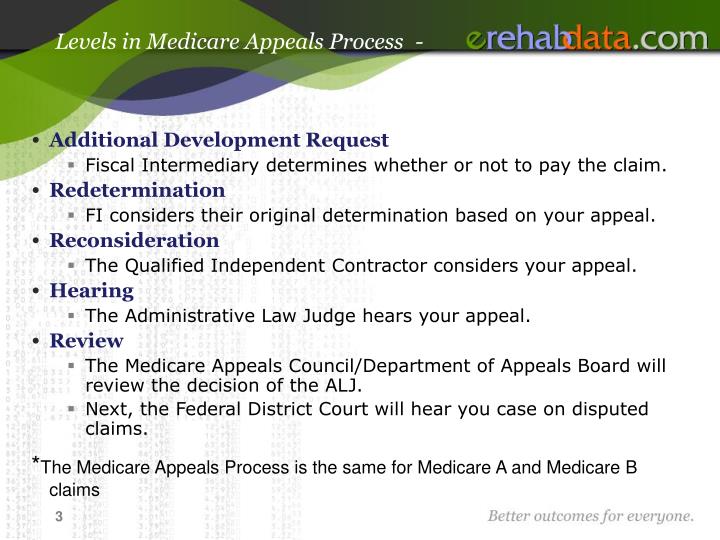
What are the 5 levels of appeals?
The 5 potential levels of appeal are described below.Level 1: Redetermination. ... Level 2: Reconsideration by Qualified Independent Contractor (QIC) ... Level 3: Administrative Law Judge (ALJ) Review. ... Level 4: Medicare Appeals Council (MAC) ... Level 5: Federal Court.
How many steps are there in the Medicare appeal process?
The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.
What is a Level 1 appeal?
Appeal the claims decision. Level 1 Appeal: "redetermination" The first level of an appeal for Original Medicare is called a redetermination. A redetermination is performed by the same contractor that processed your Medicare claim.
What is the last level of appeal for Medicare?
The levels are: First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC) Third Level of Appeal: Decision by the Office of Medicare Hearings and Appeals (OMHA)
What are 5 levels of Medicare appeals?
Medicare FFS has 5 appeal process levels:Level 1 - MAC Redetermination.Level 2 - Qualified Independent Contractor (QIC) Reconsideration.Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition.Level 4 - Medicare Appeals Council (Council) Review.
What is a Level 2 appeal?
Second Level of Appeal: Reconsideration by a Qualified Independent Contractor. Any party to the redetermination that is dissatisfied with the decision may request a reconsideration.
What is Level 3 Medicare?
Appeals Level 3: Decision by the Office of Medicare Hearings and Appeals (OMHA) You may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
What are the five steps of the appeals process?
The 5 Steps of the Appeals ProcessStep 1: Hiring an Appellate Attorney (Before Your Appeal) ... Step 2: Filing the Notice of Appeal. ... Step 3: Preparing the Record on Appeal. ... Step 4: Researching and Writing Your Appeal. ... Step 5: Oral Argument.
How many levels of an appeal can a member exercise?
There are 5 levels of appeals available to you: Redetermination. Reconsideration. Administrative Law Judge (ALJ)
When a Medicare claim is appealed the final fifth level of the appeal process is the quizlet?
Rationale: The fifth level of appeal is the Federal District Court. If the provider or the patient is not satisfied with the Council's decision, a request for a hearing before a federal district court can be requested within 60 days as long as the amount of the appeal meets or exceeds $1460 for 2015.
What percentage of Medicare appeals are successful?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
What is a lower level of care denial?
Lower level of care" is a denial that applies when the following occurs: • Care provided on an inpatient basis is typically provided on an outpatient basis. • Outpatient procedure could have been done in the provider's office. • Skilled nursing care could have been performed by a home health agency.
Overview Of Medicare Appeals Process
If you disagree with a decision by Medicare on whether to provide coverage or payment for a certain medical service, then you have certain appeal rights. You can make an appeal request for Medicare to reconsider their decision. There are five levels to the appeals process although they may not all be necessary for your specific appeal.
Five Levels Of Medicare Appeals
Similar to the court system, there are different levels of appeals in Medicare. If you are unsuccessful at one level, then you can appeal to the next level. If you go all the way to the top, you could end up in Federal court. In practice though, very few appeals make it that far. Here are the different levels and what you need to know about each.
How Long Do You Have To File An Appeal?
The answer depends on which stage of the process you are currently in. Initially, you should look at your Medicare Summary Notice (MSN) for the claim that you wish to appeal. It will have a date printed on it by which you must file your first level appeal. Generally, this date is 120 days from the date you received the initial determination.
Tips For Winning Your Appeal
We know that you want to win your appeal or else you would not be filing it in the first place. There are some things that you should keep in mind when filing appeals with the Centers for Medicare & Medicaid Services. If you keep these tips in mind, it can greatly increase your odds of being successful.
The Bottom Line
If you disagree with a decision by Medicare whether to cover a service or how much to pay, then you have a right to file an appeal. It could be nearly any decision that they make from whether to pay for care in a skilled nursing facility to whether a prescription drug is medically necessary.
How successful are Medicare appeals?
Medicare appeals are actually quite successful. In fact, data has shown that roughly 80% to 90% of appeals are won by the claimant who is appealing the decision. If you do not win your appeal at the first or second level, do not give up. Keep going as far in the appeals process as possible to increase your odds of ultimately winning your appeal.
How long does Medicare have to respond to an appeal?
It depends on which stage of the appeals process you are on. For Level 1, the general timeframe to respond to the appeal is 60 days. At level 2, the decision is again made within 60 days. If a decision cannot be reached in this timeframe, you will still receive notice of your rights in the appeals process.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
How many levels of appeals are there?
The appeals process has five levels. Each level is a different review process with a different timetable. You’ll need to request an appeal at each level. If your appeal is successful at the first level, or if you agree with Medicare’s reasoning for denying your appeal, you can stop there. However, if your appeal was denied ...
What is Medicare appeal?
It helps to provide evidence that supports your appeals case from a doctor or other provider. There might be times when Medicare denies your coverage for an item, service, or test. You have the right to formally disagree with this decision and encourage Medicare to change it. This process is called a Medicare appeal.
Why is Medicare denying my coverage?
There are a few reasons Medicare might deny your coverage, including: Your item, service, or prescription isn’t medically necessary.
What is a fast appeal?
In a few cases, you’ll file what’s called a fast appeal. Fast appeals apply when you’re notified that Medicare will no longer cover care that’s: at a hospital. at a skilled nursing facility. at a rehabilitation facility. in hospice.
Why do you appeal Medicare?
Reasons for appeal. Appeals process. Takeaway. You’ll receive a notice when Medicare makes any decisions about your coverage. You can appeal a decision Medicare makes about your coverage or price for coverage. Your appeal should explain why you don’t agree with Medicare’s decision. It helps to provide evidence that supports your appeals case ...
How long does it take to get a decision from Medicare?
You’ll hear a decision about your appeal within 60 days.
How long does a hospital have to decide on a BFCC QIO?
In the case of a hospital, the BFCC-QIO will have 72 hours to make its decision. A hospital can’t discharge you while your case is being reviewed by the BFCC-QIO. In the case of nursing facilities or other inpatient care settings, you’ll receive a notice at least 2 days before your coverage ends.
What is the entry point for Medicare appeals?
The entry point of the appeals process depends on the part of the Medicare program that covers the disputed benefit or whether the beneficiary is enrolled in a Medicare Advantage plan. There are five levels in the Medicare claims appeal process: Level 1: Your Health Plan.
What is the level 1 of Medicare?
Level 1: Your Health Plan. If you disagree with a Medicare coverage decision, you may request your health plan to redetermine your claim. Level 2: An Independent Organization. If you disagree with the decision in Level 1, you may request a reconsideration by an independent organization. Level 3: Office of Medicare Hearings and Appeals (OMHA).
What is the decision of Medicare?
In most cases, the decision is whether or not a medical service or item is covered and how much the Medicare program will pay for the service or item. There are different names for these decisions depending on the part of the Medicare program covering the benefits.
What is level 3 in Medicare?
Level 3 is filing an appeal with the Administrative Law Judge (ALJ). ALJs hold hearings and issue decisions related to Medicare coverage determination that reach Level 3 of the Medicare claims appeal process. Level 4 is the Department Appeals Board (DAB) Review.
What is level 1 DME?
Level 1 is a Redetermination, which is conducted by the DME MAC. A Redetermination is a completely new, critical re-examination of a disputed claim or charge. You should not request a Redetermination if you have identified a minor error or omission when you first filed your claim. In that case, you should request a "Reopening".
How long does it take to get a reconsideration letter from the QIC?
All Reconsideration requests must be submitted in writing to the QIC within 180 days of receiving the redetermination letter. The QIC has 60 days to render a reconsideration decision.
How long does it take to redetermine a CGS?
CGS has 60 days to complete a redetermination. If additional documentation is required, the processing time is 74 days from the date of the initial receipt. Level 2 is a Reconsideration. This appeal is conducted by the Quality Independent Contractor (QIC).
