
Overall, 68.4% of Medicare beneficiaries had 2 or more chronic conditions and 36.4% had 4 or more chronic conditions (Table 2). The prevalence of multiple chronic conditions (≥2) increased with age and was higher for women than men across all age groups.
Full Answer
What is considered a chronic condition for Medicare beneficiaries?
A Medicare beneficiary is considered to have a chronic condition if the CMS administrative data have a claim indicating that the beneficiary received a service or treatment for the specific condition. Chronic conditions are identified by diagnoses codes on the Medicare claims. On October 1, 2015 the conversion
Why does Medicare spend so much on chronic conditions?
Mar 18, 2021 · Chronic conditions are common among the Medicare population, with a significant share living with at least one chronic disease (Exhibit 1). 5 Of all non-dual-eligible Medicare beneficiaries in 2017, 66 percent were living with two or more chronic conditions. 6 Individuals with multiple chronic conditions are at an even higher risk for experiencing severe illness from …
What is the prevalence of multiple chronic conditions?
Nov 11, 2002 · “Our research shows that 82 percent of Medicare beneficiaries have at least one chronic condition; 65 percent have multiple chronic conditions and account for 95 percent of all Medicare expenditures,” explained co-author Gerard Anderson, PhD, professor of Health Policy and Management and International Health at the Johns Hopkins Bloomberg School of Public …
How many Medicare beneficiaries enrolled in the fee-for-service program in 2010?
Jan 16, 2014 · Medicare Part A beneficiaries had more chronic conditions on average in 2010 than in 2008. The percentage increase in the average number of chronic conditions was larger for dual-eligible beneficiaries (2.8%) than for nondual-eligible beneficiaries (1.2%).
What are the chronic conditions that Medicare covers?
The increase in chronic health conditions among Medicare beneficiaries has far-reaching implications for the Medicare system (1,2). Among Medicare beneficiaries, not only are hypertension, high cholesterol, heart disease, and diabetes highly prevalent, but most beneficiaries have multiple chronic conditions. Medicare beneficiaries with multiple chronic conditions are the heaviest users of health care services, including such high-cost services as hospitalizations and emergency department visits, which translates into increased Medicare spending. For example, the two-thirds of beneficiaries with 2 more chronic conditions accounted for 93% of Medicare spending, and the one-third with 4 or more chronic conditions accounted for almost three-fourths of Medicare spending (3).
What percentage of Medicare beneficiaries are younger than 65?
Among our population of fee-for-service Medicare beneficiaries, 17.1% percent were younger than 65, who receive Medicare primarily as a result of having a disability, and 82.9% were aged 65 or older ( Table 1 ). Female beneficiaries were older than male beneficiaries, particularly in the group aged 85 or older (17.8% of women compared with 10.7% of men). Our study population was 81.2% non-Hispanic white, 9.6% non-Hispanic black, 5.7% Hispanic, and 2.2% Asian or Pacific Islander. Race/ethnicity did not vary greatly between men and women. Approximately one-fifth (21.6%) of Medicare beneficiaries were also eligible for Medicaid; more female beneficiaries were dual-eligible than men.
What is the HHS initiative?
Although research has focused on chronic conditions such as hypertension, diabetes, and heart conditions (1), the US Department of Health and Human Services (HHS) Initiative on multiple chronic conditions calls for the need to enhance the understanding of chronic condition comorbidities.
What is CMS obligated to do?
Section 552a and the HIPAA Privacy Rule, 45 C.F.R Parts 160 and 164, to protect the privacy of individual beneficiaries and other persons. All direct identifiers have been removed and information is suppressed that is based upon one (1) to ten (10) beneficiaries. Suppressed data are noted by an asterisk “*”. Counter or secondary suppression is applied in cases where one sub-group (e.g. age group) is suppressed, then the other sub-group is suppressed.
What is CMS CCW?
The CMS CCW database includes pre-defined indicators for chronic conditions and mental health conditions. To be consistent with the parameters outlined in the Department of Health and Human Services Initiative on Multiple Chronic Conditions (MCC)3,4, we examined the following conditions:
What are the risks of Medicare?
They are at an increased risk for contracting the virus, experiencing disruptions in routine disease management, and being unable to access care through telemedicine. Policy options to mitigate these impacts include ensuring equity in the scale-up ...
How long does Medicare Part D last?
The Coronavirus Aid, Relief, and Economic Security (CARES) Act, for example, required that Medicare Part D plans provide up to 90-day refills of prescriptions, allowing beneficiaries enrolled in Part D to access an extended supply of medications and avoid traveling to the pharmacy as frequently. 20.
How much did telemedicine increase in 2020?
In the last week of March 2020, telemedicine visits increased by 154 percent, compared with the same period in 2019. 17 Telemedicine use increased by 13,000 percent among fee-for-service Medicare beneficiaries between March 2020 and April 2020. Dual-eligible beneficiaries exhibited higher rates of telemedicine use ...
Is CMS extending waivers?
In the future, continued regulatory flexibility and extension of CMS waivers could help improve chronic condition management in the Medicare population. Although Congress has instituted many regulatory changes to improve access to care during COVID-19, the vast majority of these policies are temporary and set to expire. 37 CMS has stated that it will likely remove these policies gradually as the pandemic comes to an end. Yet at the same time, some policymakers have discussed permanently implementing certain popular policies, such as expanded reimbursements for telemedicine.
What is the Hospital Without Walls initiative?
In response to the critical shortage of inpatient beds during the COVID-19 pandemic, CMS advanced the Hospital Without Walls initiative, a series of waivers that have allowed acute care to be delivered outside of hospitals. These waivers have allowed ambulatory surgical centers to become temporarily certified as hospitals to provide postoperative recovery for patients closer to home.
Who is the Empress EMS paramedic?
Community paramedic Karine Casciano assesses a patient, 88, during a home wellness check on December 23, 2020, in Hawthorne, New York. Contracted by local hospitals, Empress EMS sends paramedics for follow-up visits to patients, some still COVID-19-positive, after their discharge from hospital stays. Photo: John Moore/Getty Images
Does telemedicine help with health disparities?
An important policy consideration will be to ensure that any telemedicine solution does not exacerbate the immense health disparities exposed by the COVID-19 pandemic. Older adults, who make up the majority of Medicare beneficiaries, may not have the digital literacy or technology to easily navigate telemedicine services. One survey from 2015, for example, found that more than one-third of U.S. households headed by a person age 65 or older did not have a desktop or laptop, and more than half did not have a smartphone. 29
Abstract
Introduction#N#Medicare beneficiaries who have chronic conditions are responsible for a disproportionate share of Medicare fee-for-service expenditures.
Introduction
Medicare beneficiaries who have chronic conditions are responsible for a disproportionate share of Medicare fee-for-service expenditures (1,2). The amount of research on rising health care costs and the deteriorating health of the US population is considerable.
Methods
We conducted a retrospective analysis of the prevalence of chronic conditions among Medicare fee-for-service beneficiaries enrolled in Part A (hospital insurance).
Results
The average number of chronic conditions increased by 2.0% between 2008 and 2010 (1.2% for nondual-eligible beneficiaries and 2.8% for dual-eligible beneficiaries) ( Table 1 ). The increase in average number of chronic conditions for nondual-eligible women (1.5%) was larger than the increase for nondual-eligible men (1.0%).
Discussion
This study compared the health of Medicare beneficiaries enrolled in Medicare Part A for a full year in 2008 and 2010 by using data on 11 chronic conditions from the CMS Chronic Conditions PUFs.
Acknowledgments
I thank Kimberly Lochner, Christine Cox (CMS, Office of Information Products and Data Analytics), and Samuel “Chris” Haffer (CMS, Office of Minority Health), Michael Davern (NORC at the University of Chicago), and Holly Korda (Health Systems Research Associates) for their thorough review of and comments on this article.
Author Information
Erkan Erdem, PhD, Senior Manager, KPMG, LLP, 1676 International Dr, Ste 1200, McLean, VA 22102. Telephone: 703-286-8188. E-mail: [email protected].

Abstract
Introduction
- The increase in chronic health conditions among Medicare beneficiaries has far-reaching implications for the Medicare system (1,2). Among Medicare beneficiaries, not only are hypertension, high cholesterol, heart disease, and diabetes highly prevalent, but most beneficiaries have multiple chronic conditions. Medicare beneficiaries with multiple chronic con…
Analysis
- Medicare is the US federal health insurance program for people aged 65 or older, people younger than 65 with certain disabilities, and people of any age with end-stage renal disease. We examined Centers for Medicare and Medicaid Services (CMS) administrative enrollment and claims data for Medicare beneficiaries enrolled in the fee-for-service program for 2010. These CMS data are ava…
Results
- Among our population of fee-for-service Medicare beneficiaries, 17.1% percent were younger than 65, who receive Medicare primarily as a result of having a disability, and 82.9% were aged 65 or older (Table 1). Female beneficiaries were older than male beneficiaries, particularly in the group aged 85 or older (17.8% of women compared with 10.7% of men). Our study population was 81.…
Summary
- The magnitude of CMS data allowed us to examine multiple chronic conditions by relevant sociodemographic characteristics to identify the Medicare beneficiaries who may benefit most from targeted interventions and health care management strategies aimed at delivering health care in a more effective and efficient manner. More than 21 million Medicare...
Acknowledgments
- The authors gratefully acknowledge Anand Parekh, Rick Goodman, Sam Posner, and members of the HHS Multiple Chronic Conditions Data Initiative Work Group for the discussions and collaborations leading to the development of this article. This research received no specific grant from any funding agency in the public, commercial, or nonprofit sectors. Top of Page
Author Information
- Corresponding Author: Kimberly A. Lochner, ScD, Centers for Medicare and Medicaid Services, Office of the Regional Administrator, 61 Forsyth St SW, Ste 4T20, Atlanta, GA 30303-8909. Telephone: 404-562-7140. E-mail: [email protected]. Author Affiliation: Christine S. Cox, Centers for Medicare and Medicaid Services, Baltimore, Maryland. Top of Page
References
- Anderson GF. Medicare and chronic conditions. N Engl J Med 2005;353(3):305–9. CrossRef PubMed
- Thorpe KE, Ogden LL, Galactionova K. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Aff (Millwood) 2010;29(4):718–24. CrossRef PubMed
- Centers for Medicare and Medicaid Services. Chronic conditions among Medicare beneficiari…
- Anderson GF. Medicare and chronic conditions. N Engl J Med 2005;353(3):305–9. CrossRef PubMed
- Thorpe KE, Ogden LL, Galactionova K. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Aff (Millwood) 2010;29(4):718–24. CrossRef PubMed
- Centers for Medicare and Medicaid Services. Chronic conditions among Medicare beneficiaries, chart book. Office of Information Products and Data Analytics; 2011. https://www.cms.gov/Research-Statis...
- US Department of Health and Human Services. HHS Initiative on Multiple Chronic Conditions. Office of the Assistant Secretary for Health; 2012. http://www.hhs.gov/ash/initiatives/mcc/. Accessed May...
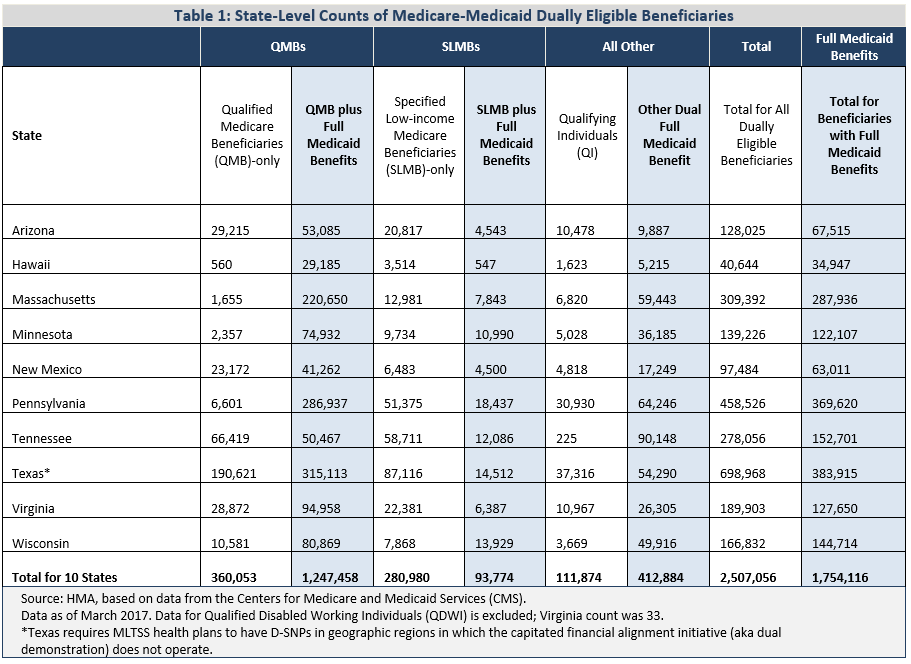
Tables
- Abbreviation: NA, not applicable. aRefers to Medicare beneficiaries who also were eligible for Medicaid. aDual eligibility refers to beneficiaries that are eligible to receive benefits under both the Medicare and Medicaid programs. aMedicare beneficiaries had to have at least 2 of the chronic conditions listed. aMedicare beneficiaries had to have at least 3 of the chronic conditions listed…