What would happen to Medicare if the Affordable Care Act is overturned?
Likewise, the acceleration of the insolvency of the Part A trust fund caused by overturning the ACA would result in a 10 percent cut in hospital benefits when reserves are exhausted. Congress must reenact the Medicare provisions in the ACA if the Supreme Court upholds the 2018 District Court decision.
How many Medicare Advantage organizations overturn denials each year?
When beneficiaries and providers appealed preauthorization and payment denials, Medicare Advantage Organizations (MAOs) overturned 75 percent of their own denials during 2014-16, overturning approximately 216,000 denials each year.
How many Supreme Court rulings have been overturned?
"The Supreme Court has overturned more than 300 rulings. Is Roe next?". CNN. Retrieved 2020-01-17. Brandon J. Murrill, The Supreme Court's Overruling of Constitutional Precedent, Congressional Research Service, September 24, 2018.
How many Medicare Advantage decisions were issued during 201416?
Source: OIG analysis of 201416 Medicare Advantage annual performance data, 2018. Using the annual performance data for contracts with validated data, we examined the outcomes of the 1.3 billion initial preauthorization and payment decisions and the 863,217 appeal decisions that MAOs issued during 201416.

Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
How many steps are there in the Medicare appeal process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
How does Medicare handle disputes over claims?
You'll get a “Medicare Redetermination Notice” from the MAC, which will tell you how they decided your appeal. If you disagree with the decision made, you have 180 days to request a Reconsideration by a Qualified Independent Contractor (QIC), which is level 2 in the appeals process.
Why do Medicare claims get denied?
If the claim is denied because the medical service/procedure was “not medically necessary,” there were “too many or too frequent” services or treatments, or due to a local coverage determination, the beneficiary/caregiver may want to file an appeal of the denial decision. Appeal the denial of payment.
How successful are Medicare appeals?
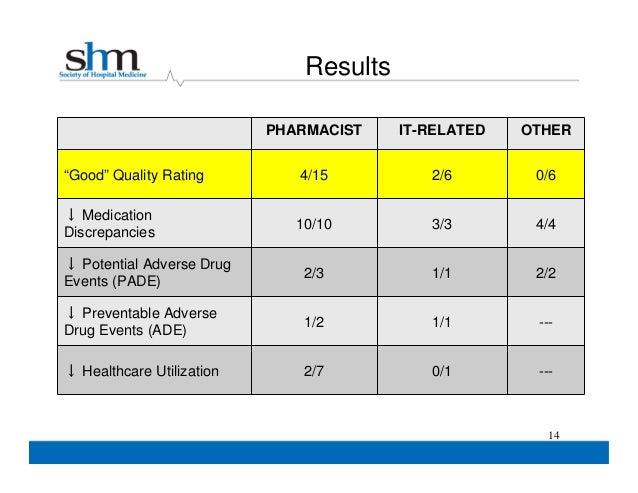
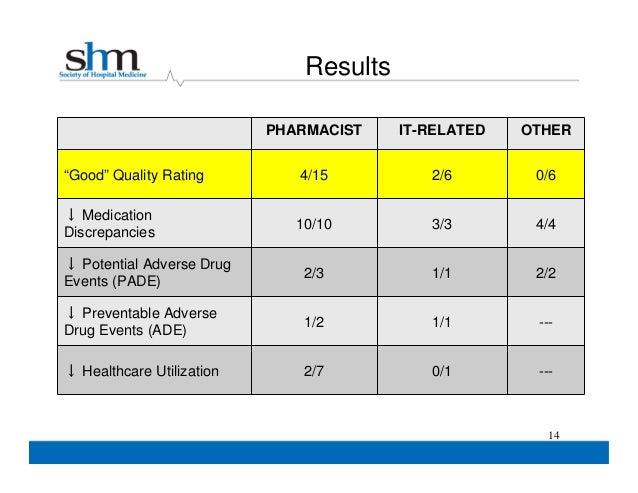
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
What is the difference between reconsideration and redetermination?
Any party to the redetermination that is dissatisfied with the decision may request a reconsideration. A reconsideration is an independent review of the administrative record, including the initial determination and redetermination, by a Qualified Independent Contractor (QIC).
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
Can you be denied Medicare coverage?
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan. If a Medicare Advantage plan gave you prior approval for a medical service, it can't deny you coverage later due to lack of medical necessity.
What are the four levels of Medicare appeals?
First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC) Third Level of Appeal: Decision by the Office of Medicare Hearings and Appeals (OMHA) Fourth Level of Appeal: Review by the Medicare Appeals Council.
What percentage of Medicare claims are denied?
The amount of denied spending resulting from coverage policies between 2014 to 2019 was $416 million, or about $60 in denied spending per beneficiary. 2. Nearly one-third of Medicare beneficiaries, 31.7 percent, received one or more denied service per year.
Which health insurance denies the most claims?
An Inspector General report found Medicare Advantage plans deny 8% of claims, on average. By contrast, HealthCare.gov plans, on average, report denying about 17% of in-network claims; with some issuers fewer than 10% of in-network claims while others deny one-third or more.
How do I fight Medicare denial?
Fill out a "Redetermination Request Form [PDF, 100 KB]" and send it to the company that handles claims for Medicare. Their address is listed in the "Appeals Information" section of the MSN. Or, send a written request to company that handles claims for Medicare to the address on the MSN.
What types of Medicare decisions can I appeal?
You have the right to dispute decisions from Medicare, a Medicare health plan, or a Medicare Part D prescription drug plan that involve:
How do I start the appeals process?
Where you begin in the appeals process depends on the nature of your Medicare problem and the urgency of the needed solution.
How do I appeal if I have original Medicare?
Original Medicare includes Part A (hospital insurance) and Part B (medical insurance).
How do I appeal if I have Medicare Advantage?
Medicare Advantage plans — also known as Part C — which bundle Medicare Parts A, B, and, usually, D together, are alternative ways to get Medicare benefits. Medicare Advantage plans are sold by private insurers that Medicare approves.
How do I appeal if I have a Medicare drug plan?
Prescription drug coverage is available as an add-on to original Medicare called Medicare Part D, or as a prescription drug benefit included with a Medicare Advantage plan or other Medicare plan.
How do I maximize my chances of winning an appeal?
There are several ways to increase your chances of winning an appeal, including:
Where can I find help for my Medicare appeal?
In addition to consulting your provider, the Centers for Medicare & Medicaid Services (CMS) offers many online Medicare resources for appeals. CMS also provides a Medicare telephone helpline at 1-800-MEDICARE ( 1-800-633-4227 ).
How many beneficiaries does Medicare Advantage cover?
Because Medicare Advantage covers so many beneficiaries (more than 20 million in 2018), even low rates of inappropriately denied services or payment can create significant problems for many Medicare beneficiaries and their providers.
What percentage of denials were appealed in 2014-16?
During 2014-16, beneficiaries and providers appealed only 1 percent of denials to the first level of appeal.
How did the ACA affect Medicare?
The ACA reduced the rate of increase in Medicare payments to providers and, over a six-year period, reduced payments to Medicare Advantage plans to bring them closer to the costs of care for a beneficiary in traditional Medicare. These reductions in Medicare spending, estimated by the Congressional Budget Office (CBO) to be $802 billion over ten years, are lowering costs for Medicare beneficiaries. The Part A deductible and copayments for inpatient hospital and skilled nursing facility care are based on hospital payments; lower payments mean lower out-of-pocket costs. The Medicare Part B premium, which covers 25 percent of program costs, and the Part B deductible, which increases at the same rate as the Part B premium, are lower than they were projected to be before passage of the ACA due to lower increases in program spending.
When will the Supreme Court rule on the ACA?
The case could be argued at the Supreme Court as early as October 2020. If the lower court decision is upheld, Medicare benefit improvements in the ACA would be eliminated, ...
What would happen if the ACA was invalidated?
Most seniors would be significantly burdened by cuts to their drug and preventive care benefits if the ACA is invalidated since half of all Medicare beneficiaries live on incomes of $29,650 or less per year and spend an average of 24 percent of their Social Security check on out-of-pocket health care expenses,.
What is CMMI in Medicare?
The ACA established the Center for Medicare and Medicaid Innovation (CMMI) to develop and test new ways of delivering and paying for care that are intended to improve quality while reducing the rate of growth in Medicare spending. These include Accountable Care Organizations, bundled payments and medical homes all of which are intended to provide incentives to physicians and others to provide high-quality, coordinated care for beneficiaries, especially those with multiple chronic conditions and those dually eligible for Medicare and Medicaid. The ACA also aims to improve care and save costs through programs to reduce unnecessary hospital readmissions by coordinating care and services for patients when they leave the hospital and to reduce hospital-acquired infections.
What would happen if the ACA was upheld?
If the lower court decision is upheld, Medicare benefit improvements in the ACA would be eliminated, including closing the Medicare Part D prescription drug coverage gap, known as the “donut hole;” preventive benefits and annual wellness exams with no deductibles or copayments; and improvements in the quality of care beneficiaries receive.
How much has Medicare saved on prescription drugs?
Lower-Cost Prescription Drugs. Since passage of the ACA, nearly 12 million people with Medicare have saved over $26.8 billion on prescription drugs, an average of $2,272 per beneficiary. The ACA reduces prescription drug prices for seniors and closes the coverage gap, known as the “donut hole.”. Prior to passage of the ACA, Medicare beneficiaries ...
How many seniors received preventive care in 2016?
Because of the ACA, over 40 million seniors received at least one preventive service with no out-of-pocket costs in 2016, and over 10 million beneficiaries had an annual wellness visit.
How to contact Medicare about ALJ hearing?
You can find more information about the ALJ hearing process at the Office of Medicare Hearings and Appeals website, or call us at 1-800-MEDICARE (1-800-633-4227).
What happens if you ask OMHA for a decision without a hearing?
If you have asked OMHA for a decision without a hearing, but the ALJ decides a hearing is necessary, the ALJ will let you know when the hearing will be. If no hearing is held, either an ALJ or attorney adjudicator will review the information in your appeal record and issue a decision.
Can an OMHA make a decision without a hearing?
You can ask OMHA to make a decision without holding a hearing (based only on the information that's in your appeal record). The ALJ or attorney adjudicator may also issue a decision without holding a hearing if evidence in the hearing record supports a decision that's fully in your favor.
How many levels of appeals are there for Medicare Advantage?
The Medicare Advantage appeals process includes four levels of administrative review by several entities. At the first level, most appeals are reviewed by the MAO that issued the denial, while appeals for certain types of services are independently reviewed by Quality Improvement Organizations.
Does MAO pay for hospice?
42 CFR §§ 422.101(a) and (b); 422.102. MAOs are not responsible for paying hospice care costs for their beneficiaries—these costs are paid by Medicare fee-for-service.
How long is the shortest time to overrule a decision?
The shortest period is 11 months, for the constitutional law Fourth Amendment (re: search and seizure) cases Robbins v. California, 453 U.S. 420 decision in July 1981, overruled by the United States v. Ross, 456 U.S. 798 decision in June 1982. There have been 16 decisions which have simultaneously overruled more than one earlier decision; of these, ...
What is Supreme Court overrule?
This is a list of decisions of the Supreme Court of the United States that have been explicitly overruled, in part or in whole, by a subsequent decision of the Court. It does not include decisions that have been abrogated by subsequent constitutional amendment or by subsequent amending statutes. As of 2018, the Supreme Court had overruled more ...
How long did the Supreme Court rule on the Minturn v. Maynard case?
As of 2018, the Supreme Court had overruled more than 300 of its own cases. The longest period between the original decision and the overulling decision is 136 years, for the common law Admiralty cases Minturn v. Maynard, 58 U.S. (17 How.) 476 decision in 1855, overruled by the Exxon Corp. v. Central Gulf Lines Inc., 500 U.S. 603 decision in 1991.