The Centers for Medicare and Medicaid Services recognize the importance of chronic care management. According to CMS, more than two-thirds of beneficiaries have two chronic conditions, and nearly 14% have more than six chronic conditions. Patients with two or more chronic health conditions need chronic care services.
Full Answer
How many Medicare members have 5 or more chronic conditions?
Consider the nation’s 55 million Medicare members over the age of 65. Roughly 27.5 million have five or more chronic conditions that could be kept under control with proper care, but only 4 million or 5 million of them end up in the first cohort of the top 5% in any given year.
How much does Medicare save with chronic care management?
Overall, the Chronic Care Management program saves Medicare $74 per patient per month or $888 per patient per year. These savings were attributed to the decreased need for more expensive services (hospital care and skilled nursing care) and improved efficiencies in care. 7
What is a Medicare chronic condition?
A Medicare beneficai ry is considered to have a chronic condition if the CMS administrative data have a claim indicating th at the beneficai ry received a service or treatme nt for the specific condition. Chronic conditions are identified by diagnoses codes on the Medicare claims.
How can I help my patient manage chronic problems?
Encourage your patient and his or her caregivers to take an active role in discovering how to manage chronic problems. Think in terms of joint problem solving or collaborative care. Such an approach can increase the patient's satisfaction while decreasing demands on your time.
What percent of Medicare patients have chronic conditions?
Chronic conditions are common among the Medicare population, with a significant share living with at least one chronic disease (Exhibit 1). Of all non-dual-eligible Medicare beneficiaries in 2017, 66 percent were living with two or more chronic conditions.
How many people does Medicare provide benefits to?
In 2020, nearly four in ten (39%) of all Medicare beneficiaries – 24.1 million people out of 62.0 million Medicare beneficiaries overall – are enrolled in Medicare Advantage plans; this rate has steadily increased over time since the early 2000s.
What percentage of patients use Medicare?
18.4 percentMedicare beneficiaries In 2020, 62.6 million people were enrolled in the Medicare program, which equates to 18.4 percent of all people in the United States.
What percentage of Medicare members have at least one chronic condition?
The CDC estimates that 70 percent of all Medicare beneficiaries have at least one chronic condition, which means that the low rate of chronic disease communications between health plans and members affects most beneficiaries.
What is the biggest disadvantage of Medicare Advantage?
The takeaway There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling. Whether you choose original Medicare or Medicare Advantage, it's important to review healthcare needs and Medicare options before choosing your coverage.
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.
Who relies on Medicare?
More than 62 million people, including 54 million older adults and 8 million younger adults with disabilities, rely on Medicare for their health insurance coverage.
How fast is the Medicare population growing?
Among major payers, Medicare is expected to experience the fastest spending growth (7.6 percent per year over 2019-28), largely as a result of having the highest projected enrollment growth. The insured share of the population is expected to fall from 90.6 percent in 2018 to 89.4 percent by 2028.
How many elderly people in the US are covered by Medicare?
Medicare covers 55 million Americans, about 17 percent of the U.S. population. Its beneficiaries are the nation's oldest, sickest, and most disabled citizens. Three-quarters of them have one or more chronic conditions, and one-quarter rate their health as fair or poor.
What percentage of people have at least one comorbid condition?
Overall 45.4% (95% CI 45.1-45.7) of adults reported any of the 6 comorbidities, increasing from 19.8% (19.1-20.4) for ages 18-29 years to 80.7% (79.5-81.8) for ages 80+ years.
What percentage of beneficiary spending was spent on individuals with two or more chronic conditions?
68.4%We defined the prevalence of multiple chronic conditions as having 2 or more chronic conditions. Overall, 68.4% of Medicare beneficiaries had 2 or more chronic conditions and 36.4% had 4 or more chronic conditions.
What percent of Americans have a health condition?
More than 133 million Americans, or 45 percent of the population, have at least one chronic condition. These conditions include arthritis, asthma, cancer, cardiovascular (heart) disease, depression and diabetes, though these are only a few of many chronic illnesses that negatively impact the lives of Americans.
How long does chronic care management last?
These conditions must be expected to last at least 12 months or until the death of the patient. Also, if you’re eligible, you should take advantage ...
Why is chronic care important?
Chronic care management is critical to those with severe health conditions. It can help patients continuously manage these conditions, potentially reducing pain, and increasing relaxation, mobility, and even lifespan.
What are management services?
Management services can include: 1 Creating a plan of care with your doctor 2 At least 20 minutes of care management health services per month 3 Frequent check-ins with your doctor 4 Emergency access to health care providers
What do you need to do after a doctor visit?
After your doctor visit, you will need to give consent to start getting managed care. Finally, you and your doctor will form an in-depth care plan for your future.
Does Medicare cover medical expenses?
Thankfully, Medigap plans can help with these extra costs. While Medicare covers many of your medical needs, it doesn't cover every cost you'll face. When you enroll in a Medigap plan, you can get help with copays, deductibles, and coinsurance.
Is chronic care a Part B benefit?
This type of care is a Part B benefit. If you’re an Advantage beneficiary, you can enroll in chronic care management if you qualify.
Does Medicare cover Advantage?
If you have a Medigap plan, you may pay even less. Since Medicare covers these services, an Advantage plan will also cover you when you need this type of care. The goal of this program is to give you high-quality, coordinated care that will help you gain better health.
What is chronic care management?
Chronic care management offers additional help managing chronic conditions like arthritis and diabetes. This includes a comprehensive care plan that lists your health problems and goals, other providers, medications, community services you have and need, and other information about your health. It also explains the care you need ...
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. and. coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
What does a provider do with urgent care?
If you agree to get this service, your provider will prepare the care plan, help you with medication management, provide 24/7 access for urgent care needs, give you support when you go from one health care setting to another, review your medicines and how you take them, and help you with other chronic care needs.
Does Medicare pay for chronic care?
Chronic care management services. Medicare may pay for a health care provider’s help to manage chronic conditions if you have 2 or more serious chronic conditions that are expected to last at least a year.
How much does chronic care management save Medicare?
Overall, the Chronic Care Management program saves Medicare $74 per patient per month or $888 per patient per year. These savings were attributed to the decreased need for more expensive services (hospital care and skilled nursing care) and improved efficiencies in care. 7
How many people will be on Medicare in 2020?
With more than 61.2 million people on Medicare in 2020 (37.7 million on Original Medicare and 23.5 million on Medicare Advantage), and half of them having two or more chronic conditions, there are billions of dollars in potential savings for Medicare. 8 More importantly, the improvements in care have a real impact on quality of life.
What is chronic care management?
Chronic Care Management is an effective program developed to improve care coordination for the millions of Medicare beneficiaries with chronic medical conditions. It improves access to care, increases patient satisfaction, and decreases long-term medical complications.
What is CCM in Medicare?
This is why Medicare created the Chronic Care Management (CCM) program.
Why was the Chronic Care Management Program created?
The Chronic Care Management program was created by Medicare to close those communication gaps. It also looks to give 24/7 access to care so that people with chronic conditions have better health outcomes. 6
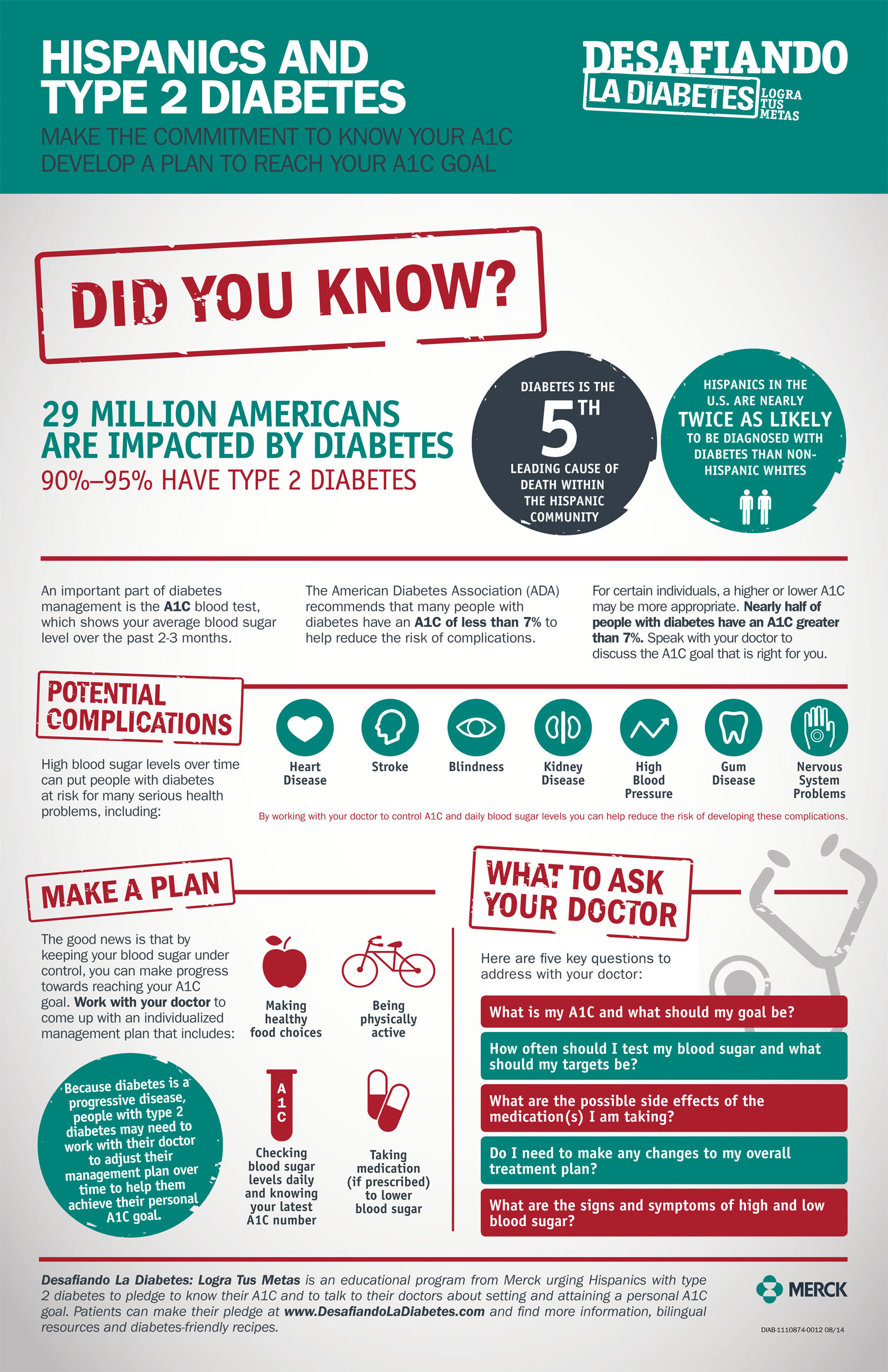
How many people have chronic diseases?
The Centers for Disease Control and Prevention reports that about 60% of adults in the United States have at least one chronic disease. 1 When you break it down by age, 86% of people 65 and older have one or more chronic diseases, 56% have two or more, and 23% have three or more. 2
Why was the Hospital Readmission Reduction Program created?
The Hospital Readmission Reduction Program was created to decrease the risk for hospital stays from common conditions like chronic obstructive pulmonary disease (COPD) and heart failure .
What is Medicare chronic condition?
Medicare is the United States’ Federal health insurance program for persons aged 65 years or older, persons under age 65 years with certain disabilities, and persons of any age with end-stage renal disease (ESRD). The data used in the chronic condition reports are based upon CMS administrative enrollment and claims data for Medicare beneficiaries enrolled in the fee-for-service program. These data are available from the CMS Chronic Condition Data Warehouse (CCW), a database with 100% of Medicare enrollment and fee-for-service claims data1.
What is CMS obligated to do?
Section 552a and the HIPAA Privacy Rule, 45 C.F.R Parts 160 and 164, to protect the privacy of individual beneficiaries and other persons. All direct identifiers have been removed and information is suppressed that is based upon one (1) to ten (10) beneficiaries. Suppressed data are noted by an asterisk “*”. Counter or secondary suppression is applied in cases where one sub-group (e.g. age group) is suppressed, then the other sub-group is suppressed.
How to get help with Medicare?
Seek help in getting Medicare coverage for necessary care by contacting the individual's doctor and the local Health Insurance Counseling Program, legal assistance program, or Area Agency on Aging. Information about htese resources is available through the national ELDER LOCATOR program by calling 1-800-677-1116.
What is skilled care in Medicare?
For care to be covered, the patient must require skilled services which may be designed to: Maintain the status of an individual's condition ; or. Slow or prevent the deterioration of a condition; or. Improve the individual's condition.
Why should Medicare not be denied?
Medicare coverage should not be denied simply because the patient's condition is chronic or expected to last a long time. "Restoration potential" is not necessary.
What is skilled care?
Skilled care is care which must be provided by, or under the supervision of, a qualified professional (nurse or physical, occupational or speech therapist) to be safe and effective.
What to do if MA care provider says maintenance and rehabilitation services are to be terminated?
If the care provider or MA plan says that your maintenance and/or rehabilitation services are to be terminated, request a written notice. The notice should contain the reason for the termination, and should explain the steps and timeliness necessary to contest the decision.
Does Medicare cover chronic conditions?
A chronic or long-term condition or disability requiring skilled services can take many forms. Medicare coverage is not limited to, or prohibited for, any particular disease, diagnosis, or disability.
Can Medicare be used for therapy?
Many beneficiaries and providers often have questions about obtaining Medicare and Medicare Advantage coverage for services provided to individuals with on-going, chronic conditions. Medicare coverage can be available for health care and therapy services even if the patient's condition is unlikely to improve.
How to make a medication plan for a patient?
For example, minimize the number of doses per day. Tailor the plan to the patient's situation and lifestyle, and try to reduce disruption to the patient's routine. Indicate the purpose of each medication. Make it clear which medications must be taken and on what schedule. It is helpful to say which drugs the patient should take only when having particular symptoms.
How to provide information to a patient?
Provide information through more than one channel. In addition to talking to the patient, you can use fact sheets, drawings, models, videos, or audio. In many cases, referrals to websites and support groups can be helpful.
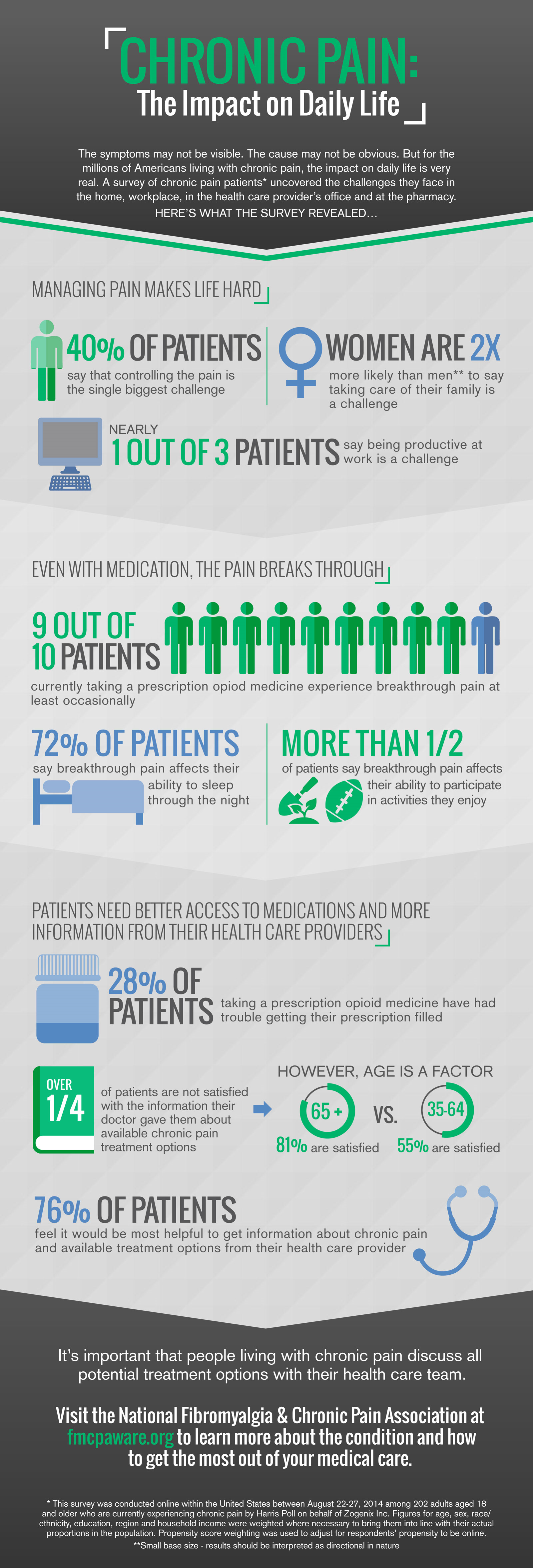
What are the challenges of coping with chronic conditions?
For many older people, coping with multiple chronic conditions is a real challenge. Learning to manage a variety of treatments while maintaining quality of life can be problematic. People with chronic conditions may have different needs, but they also share common challenges with other older adults, such as paying for care or navigating ...
Why do older patients want to know?
Most older patients want to understand their medical conditions and are interested in learning how to manage them. Likewise, family members and other caregivers want this information. Physicians typically underestimate how much patients want to know and overestimate how long they spend giving information to patients.
Why is it important to have a clinic?
Clinicians can play an important role in educating patients and families about chronic health conditions and can connect them with appropriate community resources and services.
How to explain a diagnosis?
In explaining diagnoses, it is helpful to begin by finding out what the patient believes is wrong, what the patient thinks will happen, and how much more he or she wants to know. Based on the patient's responses, you can correct any misconceptions and provide appropriate types of information.
How to encourage a patient to take notes?
Encourage the patient or caregiver to take notes. It's helpful to offer a pad and pencil. Active involvement in recording information may promote your patient's retention and adherence.
How long does a doctor spend with each patient?
In 2018 its physicians spent, on average, 189 minutes with each patient, compared with an average of only 20.9 minutes for all U.S. primary-care doctors.
How does a new primary care model help?
A new primary-care model can lower costs and improve outcomes.
Why do large employers and insurance companies need to change course?
Out of desperation to reduce their health care costs , some large employers and many health plans have contracted with disease-management programs, only to be largely disappointed with the results. It’s time for large employers and insurance companies to change course. By funding more medical assistants and paying for IT systems similar to KP’s, purchasers and insurers could see bottom-line improvements within a few years. The savings will grow even greater over time as outcomes get better for the entire population served and the total cost of caring for the sickest 5% of patients falls.
How does a medical assistant work at KP?
At KP each primary-care doctor is assigned a medical assistant. By communicating with the patient, reviewing information, readying it for the physician, relaying physician orders, and arranging transportation through community services, medical assistants help physicians manage patients’ chronic diseases better— and at a small fraction of the cost of other approaches. They save doctors enormous amounts of time—just extracting all the data from electronic health records, assembling it, and organizing patients’ clinical information could take several hours a day. While their pay varies by geography and union agreements, assistants make $40,000 to $50,000 a year, roughly half what registered nurses or nurse practitioners earn. Their training takes a year and is offered by community colleges, state colleges, and vocational schools.
How do disease management companies work?
Disease-management companies typically organize nurses and social workers into teams that focus on just one disease, which means that patients with several chronic illnesses could be dealing with multiple teams. These interactions occur outside the primary-care physician’s practice and often duplicate its work: Both the teams and the physicians monitor each patient’s laboratory results, medications, and overall health. Most patients like the convenience of disease-management programs, which they can call on for help navigating the complex care-delivery system, scheduling visits with doctors, arranging transportation, and connecting with social services. Many also take advantage of the educational opportunities and coaching that such programs provide. But the dollars the programs consume could be better used to address the needs of far more individuals.
Does Kaiser Permanente have a medical assistant?
Kaiser Permanente has developed a cost-effective model that uses relatively inexpensive medical assistants and technology to help primary-care physicians directly manage people with multiple but improvable chronic conditions—both patients who are already in the top 5% and those who are at risk of moving up into it.