
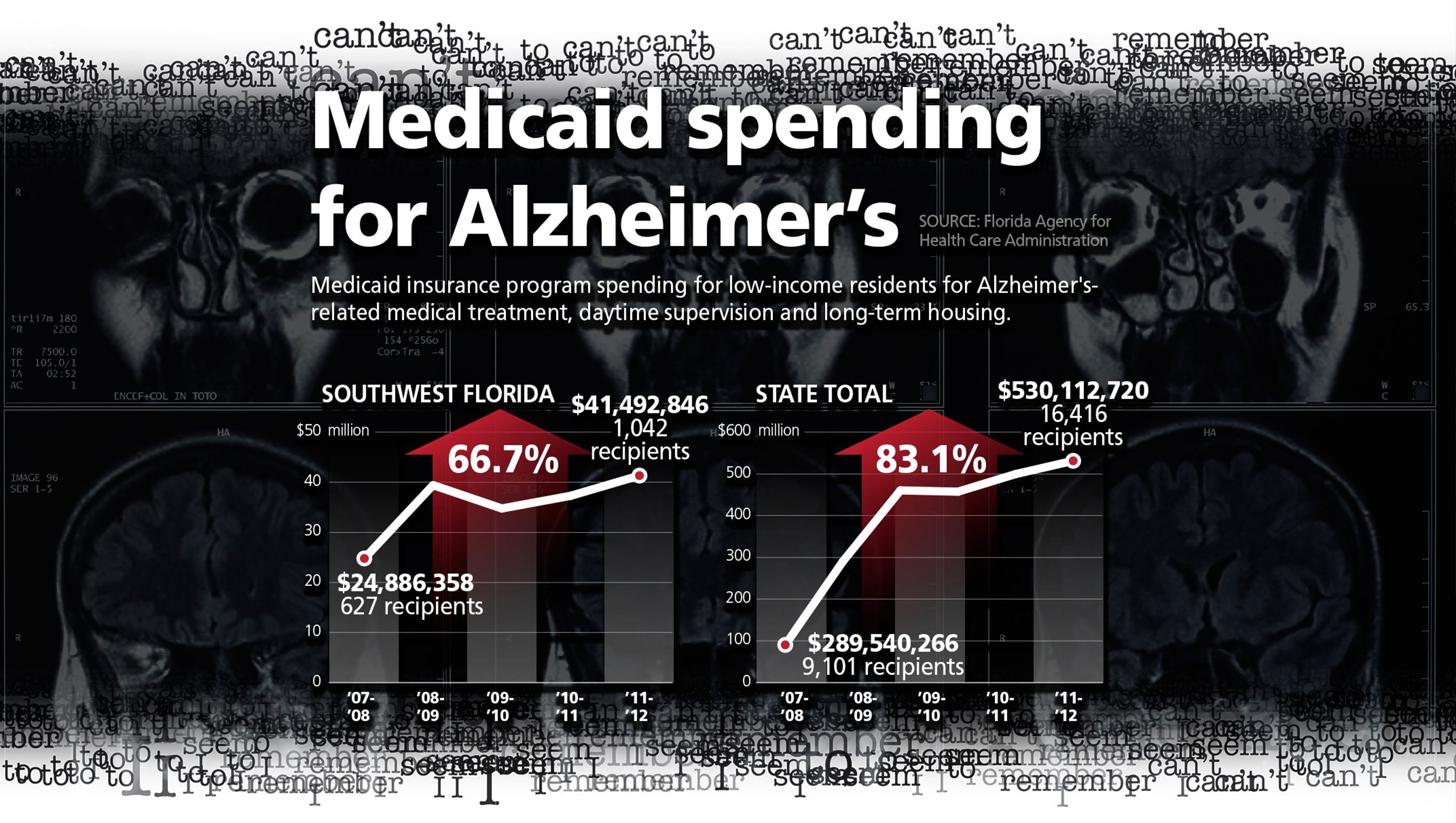
If you have Medicare, the Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If you have Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
When does my Medicare coverage start?
Medicare coverage starts based on when you sign up and which sign-up period you’re in. Generally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
How often does Medicare send you a bill?
If you have original Medicare and aren’t yet collecting Social Security, you’ll receive a bill from Medicare either monthly or once every 3 months in these cases: If you don’t have premium-free Part A, you’ll receive a monthly bill for your Part A premium.
How long do I have to file a Medicare claim?
You should only need to file a claim in very rare cases. Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
When does Medicare Part A or Part B start?
If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65. (If your birthday is on the first of the month, coverage starts the month before you turn 65.) Part B (and Premium-Part A): Coverage starts based on the month you sign up: You can sign up for Part A any time after you turn 65.
What is the billing process for Medicare?
Billing for Medicare When a claim is sent to Medicare, it's processed by a Medicare Administrative Contractor (MAC). The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days.
Is Medicare billed monthly or quarterly?
If you pay by credit or debit card, you must provide your signature and return the payment information in the return envelope we sent you. BILL TYPE Some people with Medicare are billed either monthly or quarterly. If you are billed for Part A or IRMAA Part D, you will be billed monthly.
Does Medicare send you a bill each month?
When does Medicare not send a bill? Some people receive Social Security retirement benefits or RRB benefits. In these cases, Medicare premiums come out of the benefits, so Medicare will not send the person a monthly bill.
Does Medicare send quarterly bills?
This bill will typically be for 3 months' worth of Part B premiums. So, it's known as a quarterly bill. If you have original Medicare (parts A and B), you'll continue to receive bills directly from Medicare until you start collecting either Social Security or RRB benefits.
How often is Medicare billed?
Medicare will issue Part A bills monthly and Part B bills every 3 months. There are several ways to pay the premiums, including: through the Medicare account. online through a bank's bill payment service.
Why is my Medicare bill for 5 months?
You have been charged for 5 months of Medicare Part B premiums because you are not receiving a Social Security check to have your Medicare premiums deducted.
Is there a grace period for Medicare premium payments?
Under rules issued by the Centers for Medicare and Medicaid Services (CMS), consumers will get a 90-day grace period to pay their outstanding premiums before insurers are permitted to drop their coverage.
Why is Medicare sending me a bill?
You may have to pay an additional premium if you're enrolled in a Medicare Prescription Drug Plan, Medicare Supplement (Medigap) plan, or Medicare Advantage plan. In this case, your Medicare plan will send you a bill for your premium, and you'll send the payment to your plan, not the Medicare program.
How often are Medicare Part B premiums paid?
Part B premiums You pay a premium each month for Part B. Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these: Social Security. Railroad Retirement Board.
Is Medicare paid in advance or arrears?
Social Security benefits are paid in arrears, while Medicare premiums are paid in advance, so it's important to recognize the timing of these events. 1. The individual is collecting Social Security benefits for the months of November and December of the year prior to the COLA increase to Medicare.
Are Medicare premiums tax deductible?
Since 2012, the IRS has allowed self-employed individuals to deduct all Medicare premiums (including premiums for Medicare Part B – and Part A, for people who have to pay a premium for it – Medigap, Medicare Advantage plans, and Part D) from their federal taxes, and this includes Medicare premiums for their spouse.
What month is Medicare deducted from Social Security?
The Medicare premium that will be withheld from your Social Security check that's paid in August (for July) covers your Part B premium for August. So, if you already have Part B coverage you'll need to pay your Medicare premiums out of pocket through July.
Your first chance to sign up (Initial Enrollment Period)
Generally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65.
Between January 1-March 31 each year (General Enrollment Period)
You can sign up between January 1-March 31 each year. This is called the General Enrollment Period. Your coverage starts July 1. You might pay a monthly late enrollment penalty, if you don’t qualify for a Special Enrollment Period.
Special Situations (Special Enrollment Period)
There are certain situations when you can sign up for Part B (and Premium-Part A) during a Special Enrollment Period without paying a late enrollment penalty. A Special Enrollment Period is only available for a limited time.
Joining a plan
A type of Medicare-approved health plan from a private company that you can choose to cover most of your Part A and Part B benefits instead of Original Medicare. It usually also includes drug coverage (Part D).
Answer a few questions to find out
These questions don’t apply if you have End-Stage Renal Disease (ESRD).
Do you have health insurance now?
Are you or your spouse still working for the employer that provides your health insurance coverage?
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
What is an itemized bill?
The itemized bill from your doctor, supplier, or other health care provider. A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare.
What happens after you pay a deductible?
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). , the law requires doctors and suppliers to file Medicare. claim. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
How long does it take to pay Medicare premiums?
If you enroll in Medicare before you begin collecting Social Security benef it s, your first premium bill may surprise you. It will be due, paid in full, 1 month before your Medicare coverage begins. This bill will typically be for 3 months’ worth of Part B premiums. So, it’s known as a quarterly bill.
How often do you get Medicare payments?
If you have original Medicare and aren’t yet collecting Social Security, you’ll receive a bill from Medicare either monthly or once every 3 months in these cases: If you don’t have premium-free Part A, you’ll receive a monthly bill for your Part A premium.
What happens to Medicare premiums once you start?
Once your benefits begin, your premiums will be taken directly out of your monthly payments. You’ll also receive bills directly from your plan’s provider if you have any of the following types of plans: Medicare Part C, also known as Medicare Advantage. Medicare Part D, which is prescription drug coverage.
What does it mean when you receive a Social Security check in August?
This means that the benefit check you receive is for the previous month. For example, the Social Security benefit check you receive in August is for July benefits. The Medicare premium deducted from that check will also be for July.
How much is Medicare Part B 2021?
Medicare Part B costs. Most people pay the standard Part B premium. In 2021, that amount is $148.50. If the modified adjusted gross income you reported on your taxes from 2 years ago is higher than a certain limit, though, you may need to pay a monthly IRMAA in addition to your premium.
What is Medicare Part D?
Medicare Part D, which is prescription drug coverage. Medigap, also called Medicare supplement insurance. The structure of these bills and their payment period may vary from insurer to insurer. Social Security and RRB benefits are paid in arrears. This means that the benefit check you receive is for the previous month.
Do Medicare payments go into advance?
These bills are paid in advance for the coming month or months, depending on the parts of Medicare you’re paying for. If you’re already receiving retirement benefits, your premiums may be automatically deducted from your check. Part C, Part D, and Medigap bills are sent directly from the insurance company that provides your plan.
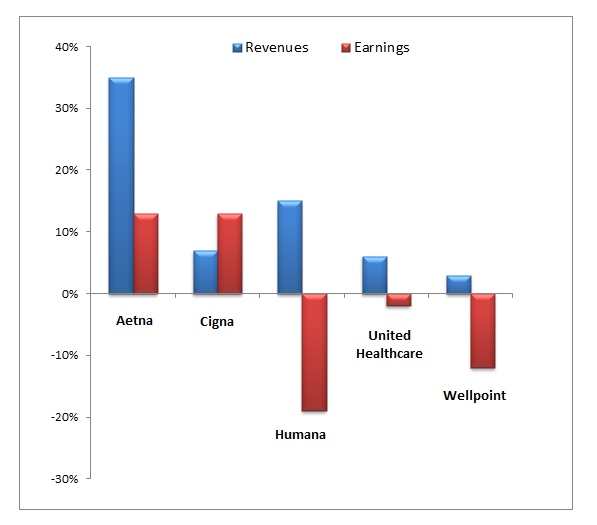
How long do you have to file a Medicare claim?
There may also be a timely filing requirement for hospitals, depending on what type of medical insurance plan you have: 1 If you have Medicare, the Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. 2 If you have Medicaid, the provider must file the claim three months following the month the service is provided. If you have Medicaid and a third-party insurance plan, in general, your provider will bill the third-party insurance plan first, and then to Medicaid for consideration of payment not to exceed the sum of the deductible, copayment, and coinsurance. If you have Medicaid and a third-party insurance plan, effective July 1, 2011, Medicaid must receive the claim after the third-party insurance, but within 12 months of the date of the month of service. 3 If you have private health insurance, the insurance company may only accept claims submitted by health care professionals within a specific period of time. For example, Cigna only considers in-network claims submitted within 3 months after the date of service. This timeline may be longer if the treating physician is out-of-network. You should read your insurance company’s Explanation of Benefits (EOB) to see if it has a similar timely filing requirement. You can also contact your insurance company to find out whether your hospital has already provided it with your medical bills.
How long does it take for a Cigna insurance company to accept a claim?
For example, Cigna only considers in-network claims submitted within 3 months after the date of service.
Does Medicaid bill third party insurance?
If you have Medicaid and a third-party insurance plan, in general, your provider will bill the third-party insurance plan first, and then to Medicaid for consideration of payment not to exceed the sum of the deductible, copayment, and coinsurance.
What is Medicare benefit period?
Medicare benefit periods mostly pertain to Part A , which is the part of original Medicare that covers hospital and skilled nursing facility care. Medicare defines benefit periods to help you identify your portion of the costs. This amount is based on the length of your stay.
How long does Medicare Advantage last?
Takeaway. Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of the facility for at least 60 days.
How much coinsurance do you pay for inpatient care?
Days 1 through 60. For the first 60 days that you’re an inpatient, you’ll pay $0 coinsurance during this benefit period. Days 61 through 90. During this period, you’ll pay a $371 daily coinsurance cost for your care. Day 91 and up. After 90 days, you’ll start to use your lifetime reserve days.
How long does Medicare benefit last after discharge?
Then, when you haven’t been in the hospital or a skilled nursing facility for at least 60 days after being discharged, the benefit period ends. Keep reading to learn more about Medicare benefit periods and how they affect the amount you’ll pay for inpatient care. Share on Pinterest.
What facilities does Medicare Part A cover?
Some of the facilities that Medicare Part A benefits apply to include: hospital. acute care or inpatient rehabilitation facility. skilled nursing facility. hospice. If you have Medicare Advantage (Part C) instead of original Medicare, your benefit periods may differ from those in Medicare Part A.
Why is it important to check deductibles each year?
It’s important to check each year to see if the deductible and copayments have changed, so you can know what to expect. According to a 2019 retrospective study. Trusted Source. , benefit periods are meant to reduce excessive or unnecessarily long stays in a hospital or healthcare facility.
How much is Medicare deductible for 2021?
Here’s what you’ll pay in 2021: Initial deductible. Your deductible during each benefit period is $1,484. After you pay this amount, Medicare starts covering the costs. Days 1 through 60.
When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar… - If your claims aren't being filed in a timely way:
1. Contact your doctor or supplier, and ask them to file a claim. 2. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and yo…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…