Is a PSA test covered by Medicare?
Under Medicare Part B, an annual PSA screening test is covered every 12 months for free if your doctor accepts Medicare assignment. If your doctor does not accept Medicare, you may pay a fee for the physician services, but not for the blood test itself. Medicare also pays for one digital rectal prostate exam each year.
Does Medicare cover PSA testing?
These tests are generally covered under Medicare benefits outlined in Part B as they are outpatient in nature. If a PSA test is administered while in a hospital or skilled nursing facility, it may be covered by Medicare benefits under Part A instead.
What are the Medicare guidelines for PSA testing?
Screening PSA tests are covered at a frequency of once every 12 months for men who have attained age 50 (i.e., starting at least one day after they have attained age 50), if at least 11 months have passed following the month in which the last Medicare-covered screening prostate specific antigen test was performed.
Will Medicare pay for elevated PSA?
Medicare will cover a PSA test for men over the age of 50. You may even be able to get testing done if you’re under 50. But your doctor must feel it’s medically necessary. A prostate-specific antigen test falls under your Part B benefits. Since the screening is preventive, you won’t pay coinsurance or deductibles.

How often does medicare pay for a PSA test?
How Often Will Medicare Pay for a PSA Test? Medicare Part B pays for one prostate cancer screening test each year. You pay no out-of-pocket cost for a PSA test if your doctor accepts Medicare assignment, and the Part B deductible does not apply. Medicare Advantage plans also cover a yearly PSA test.
How Much Does Medicare pay for PSA?
How Much Does Medicare Pay for? If you're over 50 and visit a participating provider who accepts assignments, you will pay nothing for your annual PSA test. Medicare Part B will cover 100 percent of the approved amount, with no copay or deductible.
When does Medicare stop paying for PSA?
Medicare coverage Medicare covers PSA blood test and a DRE once a year for all men with Medicare age 50 and over. There is no co-insurance and no Part B deductible for the PSA test.
What prostate procedures does Medicare cover?
Medicare covers prostate cancer screenings for the early detection of prostate cancer. Procedures covered include a digital rectal exam (DRE) and a prostate-specific antigen (PSA) test. These two screenings are covered yearly for males that are over 50 years of age.
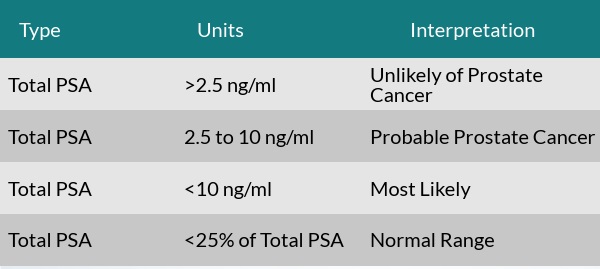
What diagnosis will cover a PSA?
PSA when used in conjunction with other prostate cancer tests, such as digital rectal examination, may assist in the decision making process for diagnosing prostate cancer. PSA also, serves as a marker in following the progress of most prostate tumors once a diagnosis has been established.
What tests are covered by Medicare?
Medicare Part B covers many types of outpatient doctor-ordered tests like urinalysis, tissue specimen tests, and screening tests. There are no copays for these tests, but your deductibles still apply. *Medicare covers diagnostic mammograms more often if your doctor orders them.
Does Medicare pay for a PSA test after age 75?
Under Medicare Part B benefits, men are eligible for rectal exams and PSA blood tests. These screenings are covered every 12 months. Medicare is specific on when you become eligible. This is a benefit “for men over 50 (beginning the day after your 50th birthday).”
How much does a PSA test cost?
The cost for a PSA test is fairly low—about $40. If your result is abnormal, the costs start adding up. Your doctor will usually refer you to a urologist for a biopsy.
Is a PSA test considered preventive?
Aetna considers prostate-specific antigen (PSA) screening a medically necessary preventive service for men 45 years of age and older who are considered average-risk for prostate cancer, and for men 40 years of age and older who are considered at high-risk for prostate cancer.
Is prostate laser surgery covered by Medicare?
Medicare covers the cost of prostate enucleation as well as hospital, anesthesia, and equipment costs. Traditional Medicare plans do not require a referral to see us and do not require pre-authorization to have laser enucleation of the prostate.
Is prostate biopsy covered by Medicare?
As long as they are medically necessary, prostate biopsies are covered by Medicare, just like any other biopsy. Your biopsy will most likely be performed on an outpatient basis, and it will, therefore, fall under Part B's medical coverage.
Does Medicare pay for prostate exams?
Medicare Part B covers one annual prostate cancer screening for individuals age 50+. The prostate screening includes: A digital rectal exam (DRE) And, a prostate-specific antigen (PSA) test.
Why is a PSA test used?
It’s important to keep in mind that a PSA test is used simply to check for levels of proteins, and this means that an irregular test result will not be enough to justify a diagnosis of cancer. There are other reasons for proteins levels to be irregular, including changes in ejaculation frequency, benign prostate hyperplasia and prostatitis.
What is the best test for prostate cancer?
One of the most common tests for prostate cancer is the prostate-specific antigen test, or PSA test. This type of test analyzes a blood sample to check for certain protein levels that may signify the development of prostate cancer. Because this test is fairly sensitive, it can detect small amounts of protein, allowing for earlier detection and treatment.
How to help prostate?
Additionally, frequent bathroom breaks can help to relieve pressure and discomfort in the prostate. Ensuring that you are active on a daily basis is also believed to help the prostate by reducing strain and increasing blood flow. Finally, some medications may be needed to help the prostate retain an optimal size.
Does Medicare cover PSA?
The good news for Medicare recipients is that the program does provide coverage for PSA tests and other screenings, including an annual digital rectal exam. These tests are generally covered under Medicare benefits outlined in Part B as they are outpatient in nature.
Does Medicare cover prostate cancer?
Medicare Part D covers prescription medications, so if drugs are prescribed in the course of treatment for prostate cancer or related prostate conditions, this part of Medicare would apply. Irregular PSA Test Results.
How often do you get a prostate test?
covers digital rectal exams and prostate specific antigen (PSA) blood tests once every 12 months for men over 50 (starting the day after your 50th birthday).
How often does Part B cover prostate?
covers digital rectal exams and prostate specific antigen (PSA) blood tests once every 12 months for men over 50 (starting the day after your 50th birthday).
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
Do you pay for a PSA blood test?
PSA test: You pay nothing for a yearly PSA blood test. If you get the test from a doctor that doesn’t accept
Medicare Coverage For Prostate Specific Antigen Test
Medicare will cover prostate-specific antigen tests for those who need it. Prostate cancer is prevalent among men. About one out of every nine men will receive a prostate cancer diagnosis. The blood test is considered a routine screening for beneficiaries. As long as your doctor takes Medicare, you should have coverage.
Personal Stories About Having A Prostate
These stories are based on information gathered from health professionals and consumers. They may be helpful as you make important health decisions.
What Do The Experts Recommend
Experts have set up guidelines to advise men about prostate cancer screening.
What Is The Cost Of A 4kscore Test And Will Insurance Cover It
We often hear from patients and physicians interested in learning more about the cost associated with the 4Kscore test, and whether the test is covered under Medicare, Medicaid or other health insurance plans. This is a confusing area and the answers always vary because of different insurance carriers and plans.
Medical Insurance Coverage For Prostate Cancer
Understanding the benefits provided by your medical insurance is critical as you explore the possible tests and treatments for prostate The prostate is a walnut-sized gland located between the bla… Full Definition cancer Cancer is a group of diseases where cells grow abnormally an… Full Definition.
How Is A Digital Rectal Exam Different From A Prostate
A digital rectal exam is when a doctor inserts his finger into your rectum to feel your prostate for signs of enlargement. A prostate-specific antigen test is a blood test that measures how much PSA is present in your blood. Often, doctors use both digital rectal exams and PSA testing to screen for prostate cancer.
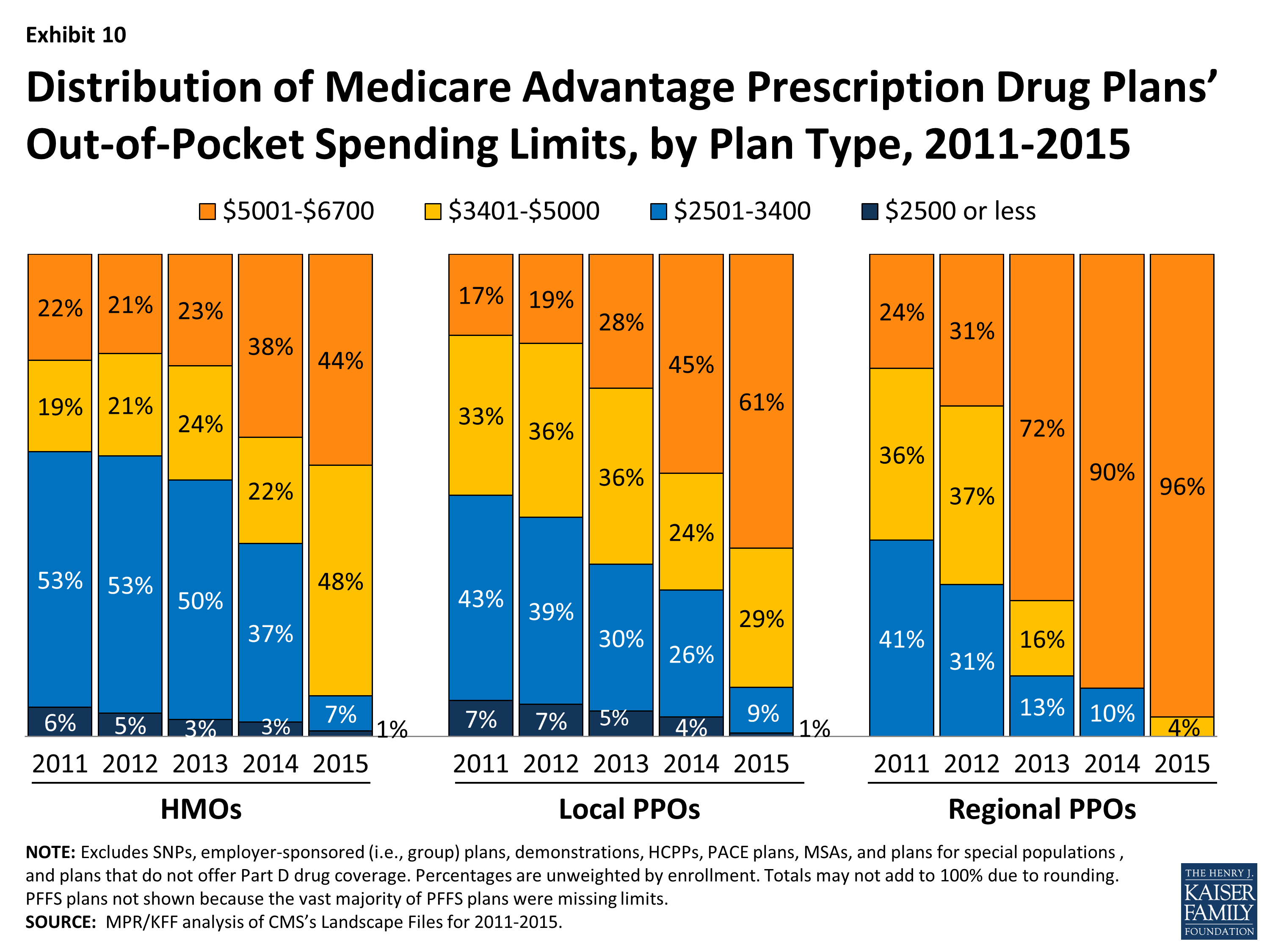
Medicare Advantage And Cancer
If you have Medicare Advantage , this means that youve purchased your Medicare plan from a private insurance company as opposed to getting it directly from the federal government. These types of plans are required to give you the same basic coverages as Original Medicare, but the CMS warns that they can have different rules and costs.
How much does a PSA blood test cost?
The cost of a PSA blood test varies based on where you live, but the American Board of Internal Medicine Foundation reports that the average cost of the test is $40. Your doctor may charge an additional fee or copayment for the office visit. If your PSA levels are elevated, you are likely to have additional costs for further testing. The average prices for common tests are:
What is a PSA test?
On a Medicare statement, a PSA Medicare screen is routine PSA testing performed annually to check for signs of prostate cancer. Most often, PSA tests fall under this category. A PSA Medicare diagnostic test is ordered by a doctor due to a suspicion that a person may have prostate cancer. For example, if you made an appointment to discuss difficulty urinating and your doctor ordered a PSA test to check your prostate, the blood work would likely be classified as diagnostic.
What is the primary screening test for prostate cancer?
The PSA test is the primary screening test for prostate cancer. To perform the test, a medical professional collects a blood sample and sends it to a lab for analysis. The test measures how much of a substance called prostate-specific antigen is present in the blood.
Does Medicare pay for prostate cancer screening?
For most men, Medicare begins paying for PSA testing at age 50. If your doctor believes that the test is medically necessary due to symptoms you are experiencing or a family history of prostate cancer, Medicare may cover the cost of a PSA test before you turn 50.
Does Medicare cover PSA blood test?
Medicare Part B usually covers 100% of the cost of annual PSA blood testing for men aged 50 and over. If your doctor assesses additional fees, Medicare Part B typically covers 80% of the costs, leaving you responsible for the remaining 20%. You may also be responsible for a copay.
Does Medicare cover PSA?
In addition to paying for the PSA test, Medicare Part B will cover 80% of the cost of annual digital rectal examinations and additional fees assessed by your doctor. You are also likely to be assessed a copay.
Does Medicare pay for PSA test?
Medicare Advantage plans must cover at least as much as what Medicare does. If your doctor assesses fees for diagnostic testing based on the results of your PSA test results, Medicare Advantage will usually pay for those additional expenses while Medicare Part B pays for the initial PSA test.
What tests are done to detect prostate cancer?
The initial tests doctors usually perform to detect prostate cancer are the digital rectal exam and prostate specific antigen (PSA) blood test.
Does Medicare Advantage have the same coverage as Medicare Part A?
If you are enrolled in a Medicare Advantage plan, you will have at least the same benefits as Original Medicare Part A and Part B, but many MA plans will offer additional coverage. Check with your plan directly for specific information.
How is the coverage of a PSA test determined?
The coverage, and subsequent payment, for a PSA test is determined by the contractual agreement with the patient's insurance company. Some insurance companies pay and others do not for procedures and other services with different diagnoses.
Does Medicare pay for PSA test?
If the PSA test is ordered with one of the diagnoses, such as cancer of the prostate, elevated PSA level, etc., Medicare will pay for it any number of times that the test is considered to be medically necessary during the year, but they will not pay for a PSA test for any other diagnoses, other than a "screening" test, as discussed below.
Does Medicare require a 25 modifier?
The simple answer is yes, it is true. For Medicare, you no longer need to use a –25 modifier on an E&M code when billed in conjunction with uroflow (51741–complex uroflowmetry or 51736–simple uroflowmetry). The reason is very simple: Medicare changed the rules.
How often is a PSA test covered by Medicare?
Screening PSA tests are covered at a frequency of once every 12 months for men who have attained age 50 (i.e., starting at least one day after they have attained age 50), if at least 11 months have passed following the month in which the last Medicare-covered screening prostate specific antigen test was performed.
What is a PSA test?
Diagnostic PSA tests are defined as those performed when the patient has signs or symptoms. If a patient has no signs or symptoms of prostate cancer, submit the appropriate code for a screening PSA. If a patient does have signs or symptoms of prostate cancer, submit the appropriate code for a diagnostic PSA.
What is the PSA code for prostate cancer?
PSA when used in conjunction with other prostate cancer tests, such as digital rectal examination, may assist in the decision-making process for diagnosing prostate cancer. PSA also, serves as a marker in following the progress of most prostate tumors once a diagnosis has been established. This test is also an aid in the management of prostate cancer patients and in detecting metastatic or persistent disease in patients following treatment. UnitedHealthcare Community Plan reimburses for Prostate Specific Antigen (PSA) (CPT code 84153), when the claim indicates a code found on the list of approved diagnosis codes for this test. UnitedHealthcare Community Plan will not reimburse when the treatment rendered is without inclusion of one of the ICD-9-CM and ICD-10-CM diagnostic codes being included on the claim accurately reflecting the member’s condition.
What is the code for prostate cancer screening?
Screening PSAs. Submit HCPCS code G0103 for screening PSA tests. Medicare coverage for screening PSAs is limited to once every 12 months.
What is prostate specific antigen?
Prostate Specific Antigen (PSA), a tumor marker for adenocarcinoma of the prostate, can predict residual tumor in the post-operative phase of prostate cancer. Three to 6 months after radical prostatectomy, PSA is reported to provide a sensitive indicator of persistent disease.
How often is a digital rectal exam covered by Medicare?
1. Screening digital rectal examinations are covered at a frequency of once every 12 months for men who have attained age 50 (i.e., starting at least one day after they have attained age 50), if at least 11 months have passed following the month in which the last Medicare-covered screening digital rectal examination was performed. Screening digital rectal examination means a clinical examination of an individual’s prostate for nodules or other abnormalities of the prostate.
Who performs the osteopathy screening?
This screening must be performed by a doctor of medicine or osteopathy (as defined in §186l (r) (1) of the Act), or by a physician assistant, nurse practitioner, clinical nurse specialist, or by a certified nurse mid-wife (as defined in §1861 (aa) and §1861 (gg) of the Act), who is authorized under State law to perform the examination, fully knowledgeable about the beneficiary, and would be responsible for explaining the results of the examination to the beneficiary.
How much does a blood test cost?
The costs are based on the particular test, your location, and the lab used. Tests can run from a few dollars to thousands of dollars. That’s why it’s important to check that your test is covered before you have it done.
How often does Medicare cover mammograms?
once a year if you meet criteria. *Medicare covers diagnostic mammograms more often if your doctor orders them. You are responsible for the 20 percent coinsurance cost. Other nonlaboratory diagnostic screenings Medicare covers include X-rays, PET scans, MRI, EKG, and CT scans.
What is Medicare Part A?
Medicare Part A offers coverage for medically necessary blood tests. Tests can be ordered by a physician for inpatient hospital, skilled nursing, hospice, home health, and other related covered services. Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines.
How much is Medicare Part B 2021?
You have to meet your annual deductible for this coverage as well. In 2021, the deductible is $203 for most people. Remember, you also have to pay your monthly Part B premium, which is $148.50 in 2021 for most beneficiaries.
Does Medigap cover out of pocket costs?
Medigap (Medicare supplemental insurance) plans can help pay for some out-of-pocket costs like coinsurance, deductibles, or copayments of covered screenings and other diagnostic tests.
Does Medicare cover 20 percent coinsurance?
You have to pay your 20 percent coinsurance as well as your deductible and any copays. Remember to go to providers that accept assignment to avoid charges Medicare won’t cover. Helpful links and tools. Medicare offers a tool you can use to check which tests are covered.
Does Medicare Advantage cover blood work?
Medicare Advantage, or Part C, plans also cover blood tests. These plans may also cover additional tests not covered by original Medicare (parts A and B). Each Medicare Advantage plan offers different benefits, so check with your plan about specific blood tests. Also consider going to in-network doctors and labs to get the maximum benefits.
How often does Medicare cover PSA?
Medicare, for example, covers screening PSA tests once every 12 months for men age 50 years and older, as instructed in the Claims Processing Manual, Chapter 18, Section 50.
What is the code for prostate cancer screening?
Some payers, including Medicare, have different coding requirements for screening and diagnostic PSA tests. For a Medicare patient, report a screening PSA with G0103 Prostate cancer screening; prostate specific antigen test (PSA) and a diagnostic PSA with one of the following three codes (based on the type of test): ...
How to know if you should use G0103 or 8415X?
You can quickly identify whether to use G0103 or 8415X by reviewing the urologist’s notes. If you don’t see signs or symptoms in the notes that indicate the patient is having a urological/prostate problem — in other words, the patient is asymptomatic — use G0103. If, instead, the urologist orders the test and documents the patient as having, for example, a firm-feeling prostate gland on rectal examination, the PSA test is diagnostic, and you should use 84153.
What happens if you don't have a PSA?
Prostate specific antigen (PSA) screenings are commonplace in most urology practices, which means if you don’t have your procedure and diagnosis coding straight, you may face high denial rates and possibly significant revenue loss. Avoid those pitfalls with these three tips.
What is the diagnosis code for malignant neoplasm of prostate?
For a screening test for a patient with no signs or symptoms of disease, use diagnosis code Z12.5 Encounter for screening for malignant neoplasm of prostate. If you report another diagnosis code with G0103, Medicare will not pay for it. You must use a screening diagnosis with a screening CPT® code.
Do you have to pay for a PSA test before one year?
A patient may need or want a screening PSA before the one-year mark has passed, and you don’t have to lose the cost of that test. You should, however, know this before the test so you can have the patient sign an advance beneficiary notice (ABN), agreeing to pay for the test themselves if the payer denies the claim based on testing frequency.
Do you need modifier 25 for PSA?
You should not need modifier 25 Significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service on the E/M service, as a global period does not apply to the PSA laboratory test.