Medicare has profoundly affected private insurance market oportunites, the technology and infrastructure used by private insurance, the culture and expectations of providers with whom private insurers must deal, and the culture and expectations of the employers and individuals who purchase private insurance.
Full Answer
What happens when you have Medicare and private insurance?
This can happen if you’re covered under private insurance through your or your spouse’s employer. When you have private insurance and Medicare, one of the two providers will pay for healthcare services first. The second provider may then potentially cover the remaining costs.
What would be the negative impact of Medicare for all?
However, a negative impact of Medicare for All would be that a single-payer system would almost certainly decrease profit margins of hospitals across the country.
How will Medicare-for-all affect the private insurance workforce?
Recognizing the likely impact on the private insurance workforce, both Medicare-for-all bills would set aside 1% of all national health expenditures per year for the first five years to offset anticipated economic dislocation of private health insurance and billing industry employees.
Do private insurers pay more for physician services than Medicare?
Across all studies, payments from private insurers are much higher than Medicare payments for both hospital and physician services, although the magnitude of the difference varies ( ES Figure 1 ).
Does Medicare pay private insurance companies?
Private insurance and original Medicare plans provide varying benefits and coverage. Most of both types of plans cover hospital care and outpatient medical services, including doctor's visits, physical therapy, and diagnostic tests. However, Medicare may have gaps in coverage that private insurers cover.
Can someone have Medicare and private insurance at the same time?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
How are insurance companies paid by Medicare?
The plans receive some funding through monthly plan premiums, but most of the money comes from Medicare. The private insurance companies that offer the plans receive a payment each month from Medicare. This covers the costs of Medicare parts A and B for each beneficiary.
How does Medicare influence reimbursement?
A: Medicare reimbursement refers to the payments that hospitals and physicians receive in return for services rendered to Medicare beneficiaries. The reimbursement rates for these services are set by Medicare, and are typically less than the amount billed or the amount that a private insurance company would pay.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Will Medicare pay my primary insurance deductible?
“Medicare pays secondary to other insurance (including paying in the deductible) in situations where the other insurance is primary to Medicare.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
What are the advantages and disadvantages of Medicare Advantage plans?
Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
How is Medicare financed?
Funding for Medicare comes primarily from general revenues, payroll tax revenues, and premiums paid by beneficiaries (Figure 1). Other sources include taxes on Social Security benefits, payments from states, and interest.
How do providers get reimbursed by Medicare?
Traditional Medicare reimbursements When an individual has traditional Medicare, they will generally never see a bill from a healthcare provider. Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider.
Do doctors lose money on Medicare patients?
Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
How does Medicare affect healthcare costs?
Overview of Medicare Spending Medicare plays a major role in the health care system, accounting for 20 percent of total national health spending in 2017, 30 percent of spending on retail sales of prescription drugs, 25 percent of spending on hospital care, and 23 percent of spending on physician services.
What percentage of Americans have private health insurance?
Others include Medicaid and Veteran’s Affairs benefits. According to a 2020 report from the U.S. Census Bureau, 68 percent of Americans have some form of private health insurance. Only 34.1 percent have public health insurance, including 18.1 percent who are enrolled in Medicare. In certain cases, you can use private health insurance ...
How does Medicare work with a group plan?
How Medicare works with your group plan’s coverage depends on your particular situation, such as: If you’re age 65 or older. In companies with 20 or more employees, your group health plan pays first. In companies with fewer than 20 employees, Medicare pays first. If you have a disability or ALS.
How to contact the SSA about Medicare?
Contacting the SSA at 800-772-1213 can help you get more information on Medicare eligibility and enrollment. State Health Insurance Assistance Program (SHIP). Each state has its own SHIP that can aid you with any specific questions you may have about Medicare. United States Department of Labor.
What is the process called when you have both insurance and a primary?
When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer. Once the payment order is determined, coverage works like this: The primary payer pays for any covered services until the coverage limit has been reached.
What is health insurance?
Health insurance covers much of the cost of the various medical expenses you’ll have during your life. Generally speaking, there are two basic types of health insurance: Private. These health insurance plans are offered by private companies.
What age do you have to be to be enrolled in Medicare?
are age 65 or over and enrolled in Medicare Part B. have a disability, end stage renal disease (ESRD), or amyotrophic lateral sclerosis (ALS) and are enrolled in both Medicare Part A and Part B. have Medicare and are a dependent of an active duty service member with TRICARE.
Does Medicare pay first or second for ESRD?
You have ESRD. COBRA pays first. Medicare may pay second, depending whether there’s overlap between your COBRA coverage and your first 30 months of Medicare eligibility based on having ESRD.
What is the paradigm shift in Medicare?
The paradigm shift is from the use ofintermediaries to handle administrative services to the bearing of this burden by p/ans that are under at--risk contracts. Past Medicare legislation called for the use of private insurers to handle the administrative processing for the program. The use of intermediaries, as they are called under Part A, and carriers, as they are called under Part B, allowed the program to be set up rapidly, using private processing capabilities already in place. It also allowed private insurers, particularly Blue Cross and Blue Shield plans, to profit greatly from the enactment of the program. Medicare's vast processing load required-and Medicare financed-upgrades of private insurers'
Is Medicare a 700 pound gorilla?
should do the same. But, insurers argue, Medicare is a 700-pound gorilla. When it rolls over, providers who share the bed have no choice but to go along. Aud insurers simply don't carry the same weight. But even this paradigm is shifting. Because of the oversupply of physician and
How much more do private insurers pay than Medicare?
Private insurers pay around 100-200 percent more than Medicare pays for the same services and treatments, so eliminating this sector of the American healthcare industry would greatly affect hospital profits. This is a problem because hospitals often use excess funds to invest in healthcare innovations.
How does Medicare for All affect hospitals?
One positive impact of Medicare for All would be that hospitals are guaranteed payment under a single-payer system. This would be especially beneficial to hospitals in rural communities that often serve larger ...
What would happen if Medicare for All became the new American healthcare system?
If Medicare for All becomes the new American healthcare system, many healthcare industry professionals could face major changes.
What percentage of Americans are covered by private insurance?
Many of the proposed Medicare for All bills advocate for a complete elimination of private insurers. According to data from the Kaiser Family Foundation, 56 percent of Americans are covered by private insurance, 36 percent are covered by government-funded insurance, and about 9 percent of Americans are currently uninsured.
Why is it bad for doctors to have less money?
However, if physician salaries are affected at all by a shift to a single-payer system, it would be the result of shrinking long-term pay raises rather than direct salary reductions.
Can insurance companies budge on Canadian doctors?
If a doctor pushes hard enough for their patient, the insurance company may budge, but that kind of ruthless advocacy can take a mental toll and isn’t sustainable when doctors have hundreds of patients. Canadian doctors are less than one-third as likely to dispute with insurance companies compared to American doctors.
Is Medicare for All a single payer system?
There are currently dozens of proposed bills floating around Congress which would attempt to move the United States closer (if not fully) to a single-payer healthcare system. Most bills fall under the umbrella of Medicare for All and share the commonality of providing healthcare coverage for every single American.
How many parts does Medicare have?
Before diving into how Medicare works with your existing health coverage, it’s helpful to understand how it works on its own. Medicare has four main parts: A, B, C, and D. You can also purchase Medicare supplement insurance, known as Medigap.
What happens if you miss your Medicare enrollment deadline?
If you miss your enrollment deadline, you may face penalties for signing up late— especially if you don’t have employer-provided coverage or drug coverage that Medicare considers comparable to its own.
How long do you have to enroll in Medicare Advantage?
3 You have eight months from the time your employment ends or your coverage ends (whichever comes first) to enroll in Part B. 10 You have two months after the month your coverage ends to join Part D or a Medicare Advantage plan.
What is a Medigap plan?
Medigap Plans: These plans are supplemental insurance sold by private insurance companies that can help fill gaps in Medicare coverage like copays, coinsurance (the amount you may have to pay toward a claim), and any deductibles. You must have Parts A and B to buy a Medigap plan. 6
How long do you have to sign up for Medicare?
In the year that you turn 65, you have seven months to sign up for Medicare Part A (if you have to pay for it) and Part B. You also have seven months to sign up for Part D unless you have other prescription drug coverage considered acceptable by Medicare (“creditable” prescription drug coverage). The initial enrollment period begins three months before you turn 65 and ends three months after, including the month of your birthday.
What happens if you go without prescription coverage?
If you go without creditable prescription drug coverage for 63 consecutive days, you may owe a late enrollment penalty. The penalty is permanently added to your Part D premium. 12
What happens if you don't sign up for Part A?
If like most people, you qualify for premium-free Part A, there’s no late enrollment penalty should you not sign up during your initial enrollment period. If you don’t qualify, your monthly premium may increase up to 10%, to be paid for twice the number of years you didn’t sign up. 8 If you don’t sign up for Part B and you don’t have employer-provided health insurance, you could face an even stiffer penalty: a premium increase up to 10% for as long as you have Part B. 9
What would happen if provider payment rates were lower under the public plan than under private insurance?
All other things equal, if provider payment rates were lower under the public plan than under private insurance, then the public plan would be expected to have lower premiums – assuming similar benefits and no selection effects.
What is the role of private health insurance?
population have some form of coverage delivered by a private health insurer. This includes: non-elderly people with employer-sponsored coverage or individually purchased health insurance plans; low-income Medicaid enrollees covered by managed care organizations;
How many people are in Medicare Advantage plans?
Among the more than 60 million people now covered by Medicare, about one-third ( 22 million in 2019) are in a Medicare Advantage plan. Medicare Advantage plans are required to provide all Medicare-covered services, and are subject to federal standards with respect to benefits and cost-sharing requirements, and network adequacy. Many also provide additional benefits, such as dental, vision and gym memberships. Medicare Advantage plans receive capitated, risk adjusted payments from the federal government to provide Medicare-covered services, exceeding $250 billion in 2019, sometimes supplemented by beneficiary premiums. The Congressional Budget Office (CBO) projects nearly half of all Medicare beneficiaries (47 percent) will be in a Medicare Advantage plan by 2029.
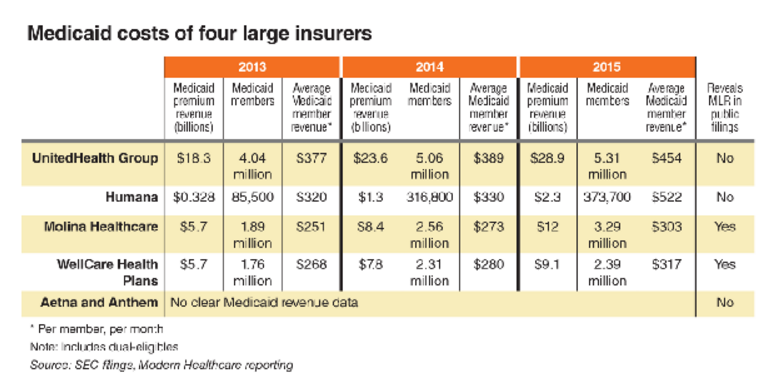
How much did Medicaid MCOs pay in 2017?
Payments to Medicaid MCOs totaled nearly $264 billion in FY 2017, accounting for about 46% of total Medicaid spending. While states contract with private plans, not all enrollment and spending is for private managed care plans. For example, California has a number of public county-operated health plans.
What is Medicare for All?
Under Medicare-for-all approaches proposed by Senator Bernie Sanders (S.1129) and Representative Pramila Jayapal (H.R.1384), all U.S. residents would be covered under a public program that provides comprehensive benefits, with no premiums or cost-sharing requirements. Both Medicare-for-all bills would prohibit employers and private health insurers from offering coverage that duplicates Medicare-for-all covered benefits. The bills would permit supplemental insurance. However, because Medicare-for-all covered benefits would be comprehensive, the market for insurance to cover supplemental benefits likely would largely be limited to nursing home care, and only under the Senate bill, since the House bill covers institutional long-term care.
What is the Sanders bill?
The Sanders Medicare-for-all bill would permit private contracting between health care providers who do not participate in the universal Medicare program and patients, and allow private insurance to cover these costs – a practice that is generally prohibited under the House bill. As a result, under the Sanders bill, ...
What is non group insurance?
Non-group, individually purchased coverage is another source of private health insurance. An estimated 14 million people had private insurance coverage in the non-group market (also known as the individual market) in the first quarter of 2018. Of this total, roughly three-quarters purchased coverage through the ACA Marketplaces, where subsidies are available to eligible individuals with incomes between 100% and 400% of the federal poverty level (FPL). Most non-group plans are ACA compliant, meaning they must cover essential health benefits and cannot discriminate based on a person’s pre-existing condition; however, recent regulatory changes have made health plans that do not comply with the ACA consumer protections increasingly available in the individual market outside the Marketplaces.
What is the difference between Medicare and private insurance?
The difference between private and Medicare rates was greater for outpatient than inpatient hospital services, which averaged 264% and 189% of Medicare rates overall, respectively. For physician services, private insurance paid 143% of Medicare rates, on average, ranging from 118% to 179% of Medicare rates across studies.
What percentage of healthcare expenditures are private insurance?
Private insurers currently play a dominant role in the U.S. In 2018, private insurance accounted for more than 40% of expenditures on both hospital care and physician services.
What is private insurance claims data?
As noted earlier, researchers are typically at a disadvantage without access to comprehensive private insurance payments from all insurers, or a sample that is representative of all private insurance claims to compare with publicly reported Medicare data. Studies that use data from larger insurers that have exceptionally strong market power relative to physicians in many markets, such as the Ginsburg 2010 study, may observe relatively low private payments. 68 A similar effect may be seen in the annual analyses conducted by MedPAC, which are based on claims data from only one large commercial PPO that operates nationwide. 69 In contrast, Song’s analysis makes use of data from the Truven MarketScan commercial claims database (now known as IBM MarketScan), which reflects over 300 private payers. 70 Compared to studies that use data only from a few large insurers, this dataset contains claims paid by several smaller insurers that do not have nationwide market penetration.
How many studies have addressed payment rates for hospitals?
Of these 19 studies, 14 addressed payments to hospitals, eight of which addressed payments for inpatient hospital services, five addressed payments for outpatient services, and seven reported relative payment rates for both types of hospital services combined, with some overlap across studies. Eight studies addressed payment rates for physician services. The full search methodology is described in the Methods section.
What is the literature review of Medicare?
This literature review summarizes findings from 19 studies that compare payment rates paid by private insurers and Medicare for hospital care and physician services, using data pertaining to the period from 2010 to the present. Studies that only addressed other types of providers such as home health services and long-term care facilities were excluded. The studies reviewed in this brief are limited to those that compare private insurance rates with rates under traditional fee-for-service Medicare; studies that addressed only payments by Medicare Advantage plans were excluded.
How much is healthcare spending?
Health care spending in the United States is high and growing faster than the economy. In 2018, health expenditures accounted for 17.7% of the national gross domestic product (GDP), and are projected to grow to a fifth of the national GDP by 2027. 1 Several recent health reform proposals aim to reduce future spending on health care while also expanding coverage to the nearly 28 million Americans who remain uninsured, and providing a more affordable source of coverage for people who struggle to pay their premiums. 2 Some have argued that these goals can be achieved by aligning provider payments more closely with Medicare rates, whether in a public program, like Medicare-for-All, a national or state-based public option, or through state rate-setting initiatives. 3,4,5,6,7,8 9,10,11
How are private insurance rates determined?
By contrast, private insurers’ payment rates are typically determined through negotiations with providers, and so vary depending on market conditions, such as the bargaining power of individual providers relative to insurers in a community.
