The federal government also funds an average of 57 percent of the operating costs for each state’s Medicaid program based on the state’s Medicaid expenditures. Meanwhile, the Medicare program is primarily funded through payroll taxes and Social Security income deductions.
Full Answer
What percentage of Medicaid spending goes to managed care?
Mar 11, 2022 · If we look at each program individually, Medicare spending grew 3.5% to $829.5 billion in 2020, which is 20% of total NHE, while Medicaid spending grew 9.2% to $671.2 billion in 2020, which is 16%...
How are Medicare and Medicaid payment rates set?
Jul 21, 2016 · The Affordable Care Act (ACA) envisions that Medicare will continue to lead the way in efforts to slow health care costs. It authorizes the Center for Medicare & Medicaid Innovation to test new models to reduce program spending while preserving or enhancing the quality of care. And the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 …
How much does the US spend on Medicare and Medicaid each year?
May 19, 2021 · It provides a shared focus on evidence-based interventions and preventive services that can improve health and control costs. 1. Medicaid is a publicly financed program that provides health insurance for millions of low-income Americans, including low-income adults, children, pregnant women, older adults and people with disabilities. 2 With Medicaid …
How is Medicare and Medicaid funded?
Jan 07, 2020 · In the aggregate, both Medicare and Medicaid payments fell below costs in 2020: § Combined underpayments were $100.4 billion in 2020, up from $75.8 billion in 2019. The 2020 underpayment includes a shortfall of $75.6 billion for Medicare and $24.8 billion for Medicaid.
How does the government control health care costs?
Costs are controlled principally through single-payer purchasing, and increases in real spending mainly reflect government investment decisions or budgetary overruns. Cost-control measures include: Mandatory global budgets for hospitals and regional health authorities. Negotiated fee schedules for providers.Jun 5, 2020
What is the best way to control the costs of the attributed Medicaid patients?
Strategies to Reduce Medicaid Acute Care SpendingPremiums, Cost Sharing, and Enrollee Wellness Incentives.Complex Care Management.Patient-Centered Medical Homes.Alternative Payment Models.Tightening Financial Eligibility Rules for Long-Term Care Services.Private Long-Term Care Insurance.More items...•Jun 21, 2017
What are three ways to reduce health care costs?
Three Ways to Lower Health Care CostsEqualizing Medicare Payments Regardless of Site-of-Care. ... Reducing Medicare Advantage Overpayments. ... Capping Hospital Prices.Feb 23, 2021
How does Medicare and Medicaid affect the economy?
Medicaid spending generates economic activity, including jobs, income and state tax revenues, at the state level. Medicaid is the second largest line item in state budgets. Money injected into a state from outside the state is critical to generating economic activity.
How can nurses reduce healthcare costs?
Another way nurses can help influence organization costs is by advocating against unnecessary treatments or medications. For example, nurses can be diligent at documenting and reporting symptoms and patient progress which would help clinical decision-making by physicians.
Why should we lower healthcare costs?
Workplace health programs will not impact many of the drivers of healthcare costs, but they can impact unhealthy behaviors and this is why reducing health care costs is one of the main benefits of wellness. By helping employees adopt and maintain healthy behaviors, they improve their health and avoid chronic diseases.Feb 22, 2022
How can medical costs be reduced?
Here are some tips on how to choose a provider and a price before getting socked with unexpected or larger-than-expected bills.Use In-Network Care Providers.Research Service Costs Online.Ask for the Cost.Ask About Options.Ask for a Discount.Seek Out a Local Advocate.Pay in Cash.Use Generic Prescriptions.More items...
How can technology reduce healthcare costs?
– Automating insurance claims processing. – Using targeted digital marketing to reduce customer acquisition costs. – Efficiently allocating human resources using staffing applications. – Automating administrative tasks, freeing physicians to spend more time with patients.
How can hospitals reduce costs?
4 Hospital Cost Reduction Ideas & StrategiesExamine appropriate labor use in different scenarios. ... Re-evaluate supply costs for hidden savings. ... Assess procedures performed for possible cost reductions. ... Track quality measures and take steps to improve deficiencies.
What is the impact of Medicaid on economic growth?
If the 14 states expand Medicaid, from 2022 to 2025 state output will rise by more than $600 billion, state gross products will increase by $350 billion, and personal incomes will grow by $218 billion in these states. Additional improvements will accrue to the rest of the nation, too.May 20, 2021
How did Medicaid affect society?
In short, Medicaid adds billions of dollars in economic activity. The federal government boosts this activity by matching state Medicaid spending at least dollar for dollar, bringing new money into states.
What are the disadvantages of Medicaid?
Disadvantages of MedicaidLower reimbursements and reduced revenue. Every medical practice needs to make a profit to stay in business, but medical practices that have a large Medicaid patient base tend to be less profitable. ... Administrative overhead. ... Extensive patient base. ... Medicaid can help get new practices established.
What is ASPs in healthcare?
A growing body of evidence demonstrates that hospital-based programs dedicated to improving antibiotic use, commonly referred to as “Antibiotic Stewardship Programs ” (ASPs), can optimize the treatment of infections and reduce adverse events associated with antibiotic use. 20.
How to manage asthma?
One way to manage asthma is using the National Asthma Education and Prevention Program (NAEPP Guidelines). 26 The goals of the NAEPP are to raise public awareness regarding the seriousness of asthma, teach people to identify its signs and symptoms, and enhance the quality of life of people with asthma.
How many people have high blood pressure?
Nearly 1 in 2 adults—108 million— have high blood pressure. 13 Most adults are aware of and treat their high blood pressure, but only about half have their blood pressure under control. 14
What is the 6|18 initiative?
New York focused on unintended pregnancies in its effort with the 6|18 Initiative. The New York State Department of Health’s Office of Health Insurance Programs (Medicaid agency) and the Division of Family Health (public health agency) worked to reduce the state’s unintended pregnancy rate by increasing access to and use of effective contraception , particularly LA RC.
How many people have asthma?
More than 24 million Americans have asthma, affecting over 7% of both adults and children. 24 People with low incomes are disproportionately affected by asthma and most low-income children with asthma are enrolled in Medicaid or the Children’s Health Insurance Program. 25
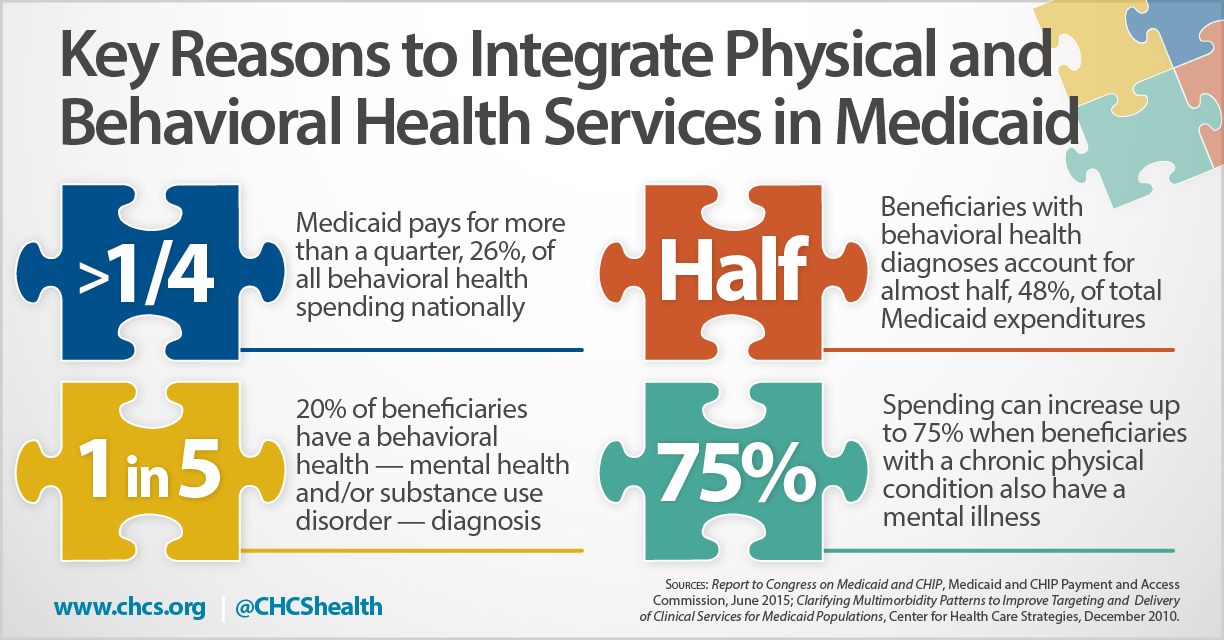
Is Medicaid a public or private program?
Medicaid is a publicly financed program that provides health insurance for millions of low-income Americans, including low-income adults, children, pregnant women, older adults and people with disabilities. 2 With Medicaid accounting for nearly 30% of total state spending, 3 state policymakers continually look for ways to reduce its costs.
How much of all births are unintended?
On average, Medicaid pays for about 46% of births in the U.S. 32 Approximately 50% of all pregnancies are unintended and these pregnancies increase the risk for poor maternal and infant outcomes. 33
How are Medicare and Medicaid payments reported?
Gross charges for these services are then translated into costs. This is done by multiplying each hospital’s gross charges by each hospital’s overall cost-to-charge ratio, which is the ratio of a hospital’s costs (total expenses exclusive of bad debt) to its charges (gross patient and other operating revenue).
How much is the Medicare shortfall?
This includes a shortfall of $56.8 billion for Medicare and $19.0 billion for Medicaid. For Medicare, hospitals received payment of only 87 cents for every dollar spent by hospitals caring for Medicare patients in 2019. For Medicaid, hospitals received payment of only 90 cents for every dollar spent by hospitals caring for Medicaid patients in 2019.
How much is Medicare underpayment?
In the aggregate, both Medicare and Medicaid payments fell below costs in 2019: 1 Combined underpayments were $75.8 billion in 2019. This includes a shortfall of $56.8 billion for Medicare and $19.0 billion for Medicaid. 2 For Medicare, hospitals received payment of only 87 cents for every dollar spent by hospitals caring for Medicare patients in 2019. 3 For Medicaid, hospitals received payment of only 90 cents for every dollar spent by hospitals caring for Medicaid patients in 2019. 4 In 2019, 63 percent of hospitals received Medicare payments less than cost, while 58 percent of hospitals received Medicaid payments less than cost.
What is underpayment in healthcare?
Underpayment occurs when the payment received is less than the costs of providing care, i.e., the amount paid by hospitals for the personnel, technology and other goods and services required to provide hospital care is more than the amount paid to them by Medicare or Medicaid for providing that care.
Is Medicare voluntary for hospitals?
Hospital participation in Medicare and Medicaid is voluntary. However, as a condition for receiving federal tax exemption for providing health care to the community, not-for-profit hospitals are required to care for Medicare and Medicaid beneficiaries. Also, Medicare and Medicaid account for more than 60 percent of all care provided by hospitals.
What is Medicare ACO model?
The Medicare-Medicaid ACO Model is open to all states and the District of Columbia that have a sufficient number of Medicare-Medicaid enrollees in fee-for-service Medicare and Medicaid. CMS will enter into Participation Agreements with up to six states, with preference given to states with low Medicare ACO saturation. Additional eligibility requirements and details about the application process are provided in the Request for Letters of Intent found at the Medicare-Medicaid ACO Model web page. States must follow all rules, including those related to Medicaid coverage, payment and fiscal administration that apply under the approach they are approved to offer. CMS will work with states to determine the appropriate Medicaid authority needed for their desired approach. State participation in the Model is contingent upon obtaining any necessary approvals and/or waivers from CMS.
What is CMS innovation center?
The CMS Innovation Center was created by the Affordable Care Act to test innovative payment and service delivery models to reduce program expenditures while preserving or enhancing the quality of care for Medicare and Medicaid beneficiaries.
What is an ACO?
On December 15, 2016, the Department of Health and Human Services (HHS) announced a new model focused on improving care and reducing costs for beneficiaries who are dually eligible for Medicare and Medicaid (“Medicare-Medicaid enrollees”). Through the Medicare-Medicaid Accountable Care Organization (ACO) Model, the Centers for Medicare & Medicaid Services (CMS) intends to partner with interested states to offer ACOs in those states the opportunity to take on accountability for both Medicare and Medicaid costs and quality for their beneficiaries. This is in accordance with the Department of Health and Human Services’ “Better, Smarter, Healthier” approach to improving our nation’s health care and the Administration setting clear, measurable goals and a timeline to move the Medicare program -- and the health care system at large -- toward paying providers based on the quality rather than the quantity of care they provide to patients. CMS is adding the Medicare-Medicaid ACO Model to its existing portfolio of ACO initiatives, which include: 1 Medicare Shared Savings Program (Shared Savings Program) 2 Pioneer ACO Model 3 Next Generation ACO Model 4 ACO Investment Model (AIM) 5 Comprehensive ESRD Care (CEC) Model
What is a letter of intent for ACO?
The Request for Letters of Intent includes some ACO eligibility criteria, but states and CMS may agree to additional criteria during the state-specific development process. A state-specific Request for Applications will be released to ACOs at a later date. In addition to applying to participate in the Medicare-Medicaid ACO Model, ACOs will be required to apply to participate in (or apply to renew their Participation Agreement for) the Shared Savings Program and ultimately sign a Participation Agreement to participate in the Shared Savings Program in order to participate in the Medicare-Medicaid ACO Model. Providers, whether currently participating in an ACO or potentially interested in joining or forming an ACO, are encouraged to participate in the state-specific development process and to submit letters of interest with their state’s Letter of Intent.
How much did Medicaid spend in 2019?
Medicaid spending grew 2.9% to $613.5 billion in 2019, or 16 percent of total NHE. Private health insurance spending grew 3.7% to $1,195.1 billion in 2019, or 31 percent of total NHE. Out of pocket spending grew 4.6% to $406.5 billion in 2019, or 11 percent of total NHE.
How much did the NHE increase in 2019?
NHE grew 4.6% to $3.8 trillion in 2019, or $11,582 per person, and accounted for 17.7% of Gross Domestic Product (GDP). Medicare spending grew 6.7% to $799.4 billion in 2019, or 21 percent of total NHE. Medicaid spending grew 2.9% to $613.5 billion in 2019, or 16 percent of total NHE.
How much of Medicaid is managed care?
Nationally, over two-thirds of Medicaid beneficiaries received most or all covered benefits through managed care in 2017. About 45 percent of Medicaid spending goes to managed care plans.
How much does the federal government contribute to Medicaid?
The federal government contributes at least $1 in matching funds for every $1 a state spends on Medicaid. The fixed percentage the federal government pays a state, known as the federal medical assistance percentage (FMAP), depends on state income levels and ranges from 50 percent to 78 percent.
What is MLR in health insurance?
One way states can do this is to require managed care plans to repay the state if they don’t meet a “medical loss ratio” (MLR) — a certain percentage of premium revenue that insurers must spend on health care services rather than administrative costs and profits.
What is a capitation payment?
Nearly all states contract with managed care plans to provide some or all covered benefits to some or all enrollees, with the state paying the plan a set monthly amount per enrollee (called a capitation payment) to cover the cost of those benefits plus the plan’s administrative costs .