What is Medicare bad debt?
Medicare bad debt is defined as Medicare coinsurance and deductible amounts that are unpaid and uncollectable from the patient. The Centers for Medicare and Medicaid Services (CMS) pays hospitals 65% of their gross Medicare bad debt if ...
How much bad debt can be recovered from Medicare?
Hundreds of millions of dollars of unrealized Medicare bad debt revenue can be recovered at scale if reporting and analysis are performed efficiently with automation — whether via a fully outsourced consulting service or by using a SaaS solution. Recoveries can be close to a half a million dollars per provider (TransUnion Healthcare proprietary data).
How much of a hospital's annual revenue is patient financial responsibility?
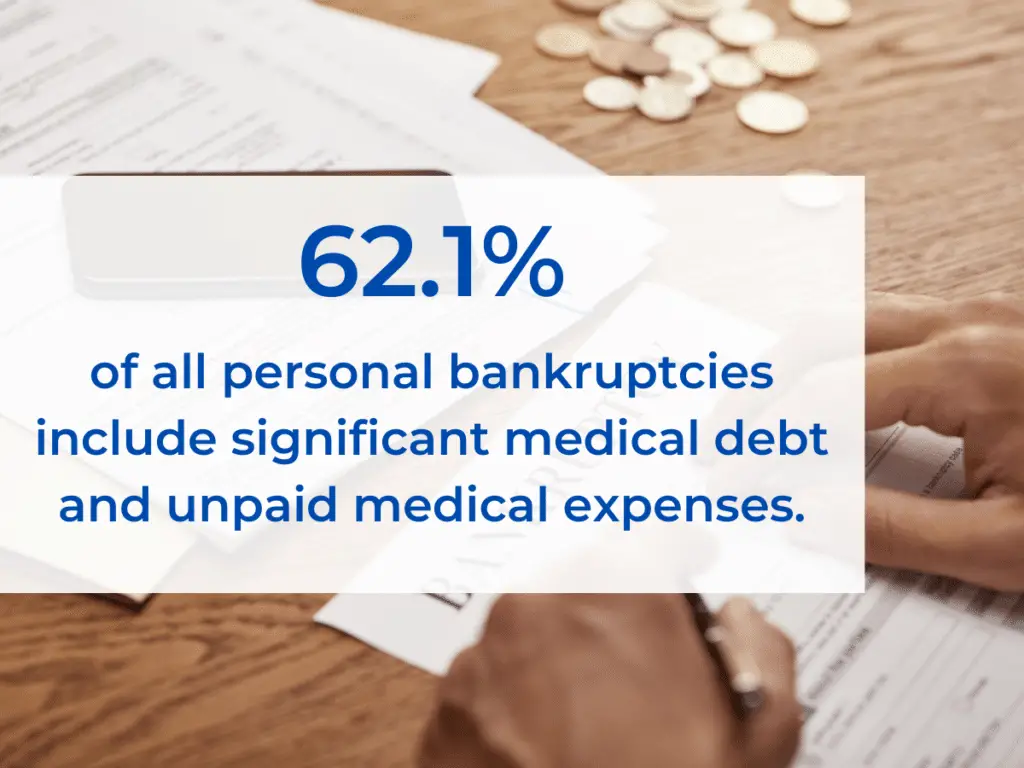
Patient financial responsibility represents more than 30% of a hospital’s annual revenues. When tackling uncompensated care, specifically as it relates to Medicare bad debt, it is important to address the problem holistically, to ensure all your earned revenue is realized. Healthcare is becoming increasingly unaffordable to many, ...
How to find bad debts?
Analyze the data. Examining accounting and transaction codes should provide an in-depth analysis to find bad debts that are payable but may have been missed. Consider having an outside partner analyze the data, which may uncover missed or previously unknown opportunities.
What does every dollar of payment mean for a hospital?
To a hospital, every dollar of payment means a better opportunity to deliver excellent patient care. By finding the right partner and tools, hospitals can accurately and efficiently recover Medicare-bad-debt revenue. The money is waiting — go get it.
Does Medicare give back money?
Secure defendable documentation. Medicare doesn’t like giving money back, so reports need to be defensible on audit. Ensure the process delivers results with the full documentation required for submission to Medicare.
Do people on Medicare have to pay for healthcare?
Although many people struggle to pay for healthcare, the issue is particularly prevalent among Medicare beneficiaries, who are often retired and on a fixed income.
What information does Medicare use for billing?
When billing for traditional Medicare (Parts A and B), billers will follow the same protocol as for private, third-party payers, and input patient information, NPI numbers, procedure codes, diagnosis codes, price, and Place of Service codes. We can get almost all of this information from the superbill, which comes from the medical coder.
What is a medical biller?
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
What is 3.06 Medicare?
3.06: Medicare, Medicaid and Billing. Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
What form do you need to bill Medicare?
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500. For the most part, however, billers will enter the proper information into a software program and then use ...
How long does it take for Medicare to process a claim?
The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days .
Is it harder to bill for medicaid or Medicare?
Billing for Medicaid. Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program ...
Can you bill Medicare for a patient with Part C?
Because Part C is actually a private insurance plan paid for, in part, by the federal government, billers are not allowed to bill Medicare for services delivered to a patient who has Part C coverage. Only those providers who are licensed to bill for Part D may bill Medicare for vaccines or prescription drugs provided under Part D.
Why is bad debt important for Medicare?
Medicare bad debts can be an important part of a hospital’s reimbursement strategy, providing a hospital with a significant cash flow for claims that otherwise wouldn’t be paid. The primary challenge when requesting reimbursement for Medicare bad debts is ensuring that documentation is kept and presented to the MAC in the required format so these claims don’t get denied.
What is Medicare bad debt reimbursement?
For hospital entities, the Medicare bad debt reimbursement is calculated as 65 percent of the uncollectible amount. This reimbursement varies by provider type.
What is the primary requirement for Medicare?
The primary requirement is the provider must put forth the same effort to collect from Medicare patients as non-Medicare patients.
What is the amount of charge eligible for bad debt reimbursement?
In general, the amount of charge eligible for bad debt reimbursement will be the coinsurance and deductible amount after the primary portion is paid by Medicare on a remittance advice.
How long does it take for a Medicare deductible to be billed?
To be considered for Medicare reimbursement, the deductible and coinsurance amounts must be billed to the patient within 90 days of the Medicare remittance advice and these dates must be presented on the bad debt listing.
What percentage of bad debt is reimbursed by Medicare?
For hospital entities, the Medicare bad debt reimbursement is calculated as 65 percent of the uncollectible amount. This reimbursement varies by provider type. This article focuses on the requirements for claiming Medicare reimbursement for bad debts, as well as some common pitfalls providers often face.
How long does it take for a provider to bill for coinsurance?
Timely billing – The provider must bill the deductible/coinsurance amount to the patient within 90 days of receiving the Medicare remittance advice. Collection agencies – If the provider uses collection agencies to attempt collection on any patient claim, the agencies must be used for Medicare claims as well.
What is Medicare Advantage?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
Why buy Medicare Supplement Insurance?
Buy a Medicare Supplement Insurance (Medigap) policy to help lower your share of costs for services you get.
Is Medicare a private insurance?
Medicare is different from private insurance — it doesn’t offer plans for couples or families. You don’t have to make the same choice as your spouse.
Do you have to have original Medicare if you have Medicare Advantage?
You’ll have Original Medicare unless you join a Medicare Advantage Plan.
Does Medicare cover urgent care?
Plans must cover all emergency and urgent care, and almost all medically necessary services Original Medicare covers. Some plans tailor their benefit packages to offer additional benefits to treat specific conditions.
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
What is included in a demand letter for Medicare?
The demand letter also includes information on administrative appeal rights. For demands issued directly to beneficiaries, Medicare will take the beneficiary’s reasonable procurement costs (e.g., attorney fees and expenses) into consideration when determining its demand amount.
How long does interest accrue?
Interest accrues from the date of the demand letter, but is only assessed if the debt is not repaid or otherwise resolved within the time period specified in the recovery demand letter. Interest is due and payable for each full 30-day period the debt remains unresolved; payments are applied to interest first and then to the principal. Interest is assessed on unpaid debts even if a debtor is pursuing an appeal or a beneficiary is requesting a waiver of recovery; the only way to avoid the interest assessment is to repay the demanded amount within the specified time frame. If the waiver of recovery or appeal is granted, the debtor will receive a refund.
How long does it take to appeal a debt?
The appeal must be filed no later than 120 days from the date the demand letter is received. To file an appeal, send a letter explaining why the amount or existence of the debt is incorrect with applicable supporting documentation.
What happens if you don't respond to a debt recovery?
Failure to respond within the specified time frame may result in the initiation of additional recovery procedures, including the referral of the debt to the Department of Justice for legal action and/or the Department of the Treasury for further collection actions.
What would happen if you paid back money?
Paying back the money would cause financial hardship or would be unfair for some other reason.
Can Medicare waive recovery of demand?
The beneficiary has the right to request that the Medicare program waive recovery of the demand amount owed in full or in part. The right to request a waiver of recovery is separate from the right to appeal the demand letter, and both a waiver of recovery and an appeal may be requested at the same time. The Medicare program may waive recovery of the amount owed if the following conditions are met:
How to contact CFPB about debt collection?
If you have a problem with a debt collector, you can submit a complaint online or call the CFPB at (855) 411-2372 . TTY/TDD users can call (855) 729-2372 . We'll forward your complaint to the debt collection company and work to get you a response from them.
What to do if your provider won't stop billing you?
If the medical provider won’t stop billing you, call Medicare at 1-800-MEDICARE (1-800-633-4227) . TTY users can call (877) 486-2048 . Medicare can confirm that you’re in the QMB Program. Medicare can also ask your provider to stop billing you, and refund any payments you’ve already made. 3.
Can you get a bill for QMB?
If you’re in the QMB Program and get a bill for charges Medicare covers: 1. Tell your provider or the debt collector that you're in the QMB Program and can’t be charged for Medicare deductibles, coinsurance, and copayments.
Is Medicare billed for QMB?
The Centers for Medicare & Medicaid Services (CMS) has heard from people with Medicare who report being billed for covered services, even though they’re in the QMB program.
How to determine primary payer for Medicare?
The CMS Questionnaire should be used to determine the primary payer of the beneficiary’s claims. This questionnaire consists of six parts and lists questions to ask Medicare beneficiaries. For institutional providers, ask these questions during each inpatient or outpatient admission, with the exception of policies regarding Hospital Reference Lab Services, Recurring Outpatient Services, and Medicare+Choice Organization members. (Further information regarding these policies can be found in Chapter 3 of the MSP Online Manual.) Use this questionnaire as a guide to help identify other payers that may be primary to Medicare. Beginning with Part 1, ask the patient each question in sequence. Comply with all instructions that follow an answer. If the instructions direct you to go to another part, have the patient answer, in sequence, each question under the new part. Note: There may be situations where more than one insurer is primary to Medicare (e.g., Black Lung Program and Group Health Plan). Be sure to identify all possible insurers.
When do hospitals report Medicare Part A retirement?
When a beneficiary cannot recall his/her retirement date, but knows it occurred prior to his/her Medicare entitlement dates, as shown on his/her Medicare card, hospitals report his/her Medicare Part A entitlement date as the date of retirement. If the beneficiary is a dependent under his/her spouse's group health insurance and the spouse retired prior to the beneficiary's Medicare Part A entitlement date, hospitals report the beneficiary's Medicare entitlement date as his/her retirement date. If the beneficiary worked beyond his/her Medicare Part A entitlement date, had coverage under a group health plan during that time, and cannot recall his/her precise date of retirement but the hospital determines it has been at least five years since the beneficiary retired, the hospital enters the retirement date as five years retrospective to the date of admission. (Example: Hospitals report the retirement date as January 4, 1998, if the date of admission is January 4, 2003)
What is secondary payer?
Medicare is the Secondary Payer when Beneficiaries are: 1 Treated for a work-related injury or illness. Medicare may pay conditionally for services received for a work-related illness or injury in cases where payment from the state workers’ compensation (WC) insurance is not expected within 120 days. This conditional payment is subject to recovery by Medicare after a WC settlement has been reached. If WC denies a claim or a portion of a claim, the claim can be filed with Medicare for consideration of payment. 2 Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer. 3 Covered under their own employer’s or a spouse’s employer’s group health plan (GHP). 4 Disabled with coverage under a large group health plan (LGHP). 5 Afflicted with permanent kidney failure (End-Stage Renal Disease) and are within the 30-month coordination period. See ESRD link in the Related Links section below for more information. Note: For more information on when Medicare is the Secondary Payer, click the Medicare Secondary Payer link in the Related Links section below.
Why did CMS develop an operational policy?
CMS developed an operational policy to help alleviate a major concern that hospitals have had regarding completion of the CMS Questionnaire.
Does Medicare pay for black lung?
Federal Black Lung Benefits - Medicare does not pay for services covered under the Federal Black Lung Program. However, if a Medicare-eligible patient has an illness or injury not related to black lung, the patient may submit a claim to Medicare. For further information, contact the Federal Black Lung Program at 1-800-638-7072.
Does Medicare pay for the same services as the VA?
Veteran’s Administration (VA) Benefits - Medicare does not pay for the same services covered by VA benefits.
Does no fault insurance cover medical expenses?
Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer.
What does a medical biller do?
The medical biller takes the superbill from the medical coder and puts it either into a paper claim form, or into the proper practice management or billing software. Biller’s will also include the cost of the procedures in the claim. They won’t send the full cost to the payer, but rather the amount they expect the payer to pay, as laid out in the payer’s contract with the patient and the provider.
Why do billers review a claim?
The biller reviews this report in order to make sure all procedures listed on the initial claim are accounted for in the report. They will also check to make sure the codes listed on the payer’s report match those of the initial claim. Finally, the biller will check to make sure the fees in the report are accurate with regard to the contract between the payer and the provider.
What does it mean when a patient is denied a claim?
A denied claim is one that the payer refuses to process payment for the medical services rendered. This may occur when a provider bills for a procedure that is not included in a patient’s insurance coverage. This might include a procedure for a pre-existing condition (if the insurance plan does not cover such a procedure).
What does "accepted" mean in medical billing?
Accepted does not necessarily mean that the payer will pay the entirety of the bill. Rather, they will process the claim within the rules of the arrangement they have with their subscriber (the patient). A rejected claim is one that the payer has found some error with.
What is the final phase of billing?
The final phase of the billing process is ensuring those bills get, well, paid. Billers are in charge of mailing out timely, accurate medical bills, and then following up with patients whose bills are delinquent. Once a bill is paid, that information is stored with the patient’s file.
What is the process of a medical claim being accepted?
Once a claim reaches a payer, it undergoes a process called adjudication. In adjudication, a payer evaluates a medical claim and decides whether the claim is valid/compliant and, if so, how much of the claim the payer will reimburse the provider for. It’s at this stage that a claim may be accepted, denied, or rejected.
Why is manual claim billing important?
Manual claims have a high rate of errors, low levels of efficiency, and take a long time to get from providers to payers. Billing electronically saves time, effort, and money, and significantly reduces human or administrative error in the billing process.
