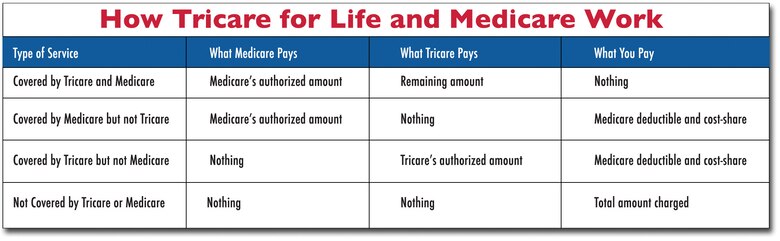
So how do the two work together to pay your health care costs? The provider will file the claim (s) with Medicare. Medicare will then pay the portion it’s responsible for and then send the claim to the TRICARE For Life claims processor. TRICARE For Life will pay its portion directly to the provider for the services TRICARE covers.
Full Answer
How does Tricare work with Medicare Advantage plans (Medicare Part C)?
How Does Medicare Work with TriCare for Life? • You are a member of the United States military. • You are a member of the National Guard or National Reserve of the U.S. • You are a military survivor. • Your former spouse was a member of the U.S. military. (This may not …
Do you have to have Medicare Part B for Tricare for life?
Apr 12, 2022 · Most people with TRICARE, who become Medicare eligible and get Medicare Part A, must also have Medicare Part B to be able to remain eligible. Part D is not required to maintain eligibility. You can remain eligible for TRICARE without enrolling in Medicare Part B only if you are: An active duty service member; An active duty family member
How do I get Tricare for my new spouse?
Dec 14, 2021 · The spouse who turns 65 first enrolls in Medicare/TFL, and the younger spouse stays in TRICARE Prime or Select until age 65. Change the younger spouse’s Prime or Select fees to the single rate rather than the family rate. Medicare/TFL in Retirement Once under the Medicare/TFL umbrella, it is easier to maintain coverage.
What is Tricare for life and how does it work?
members. Your spouse younger than age 65 would remain eligible for TRICARE Prime or TRICARE Select until they turn age 65 and become eligible for Medicare Part A and Part B. SIGNING UP FOR MEDICARE. Your birth date determines when you become entitled to Medicare and when you should sign . up for Medicare Part A and Part B. Your TFL . TRICARE ® AND …
Can Medicare and TRICARE be billed together?
Medicare is your primary payer. TRICARE pays second to Medicare or last if you have other health insurance. TRICARE supplements don't qualify as "other health insurance.". TRICARE benefits include covering Medicare's coinsurance and deductible for services covered by Medicare and TRICARE.Dec 19, 2017
Does my spouse keep TRICARE when I turn 65?
Nothing. The good news is your family's existing TRICARE coverage doesn't change. Your spouse can remain in his or her TRICARE plan. And if you have children, they remain in their current plan until they change plans or lose TRICARE eligibility.
Do you have to pay for Medicare if you have TRICARE?
When you use TRICARE For Life, you don't pay any enrollment fees, but you must have Medicare Part A and Medicare Part B. Medicare Part A is paid from payroll taxes while you are working.Jan 6, 2022
How does TRICARE for Life work with Medicare?
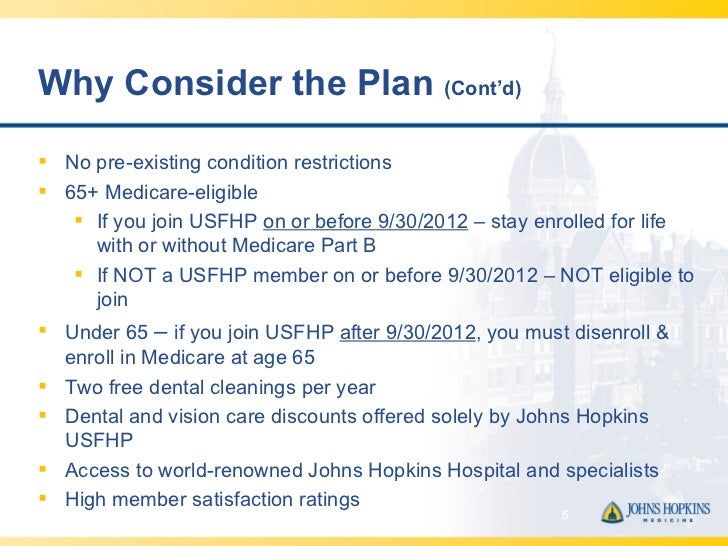
TRICARE For Life is Medicare wraparound coverage for TRICARE-eligible beneficiaries who have Medicare Parts A and B. Coverage is automatic if you have Parts A and B and pay your Part B premiums. There is no fee for enrolling in TRICARE For Life. TRICARE For Life is available worldwide and enrollment is not required.
Do widows get TRICARE for Life?
Surviving spouses remain eligible for TRICARE unless they remarry and children remain eligible until they age out or lose eligibility for TRICARE for other reasons.Nov 30, 2017
Is Medicare and TRICARE for life enough?
Is Medicare and TRICARE for Life enough? Together, the two programs provide comprehensive protection for health care needs. The cost of most treatments and services will be covered, usually without out-of-pocket charges, as long as you use a Medicare provider.
Is TRICARE free for spouses?
Spouses of service members are eligible for TRICARE coverage. Because getting married is a TRICARE Qualifying Life Event (QLE), you may change your health plan outside of the annual TRICARE Open Season. Your spouse and eligible children may also gain TRICARE coverage.Jul 16, 2020
Does TRICARE Prime end at 65?
For example, this means your new TFL coverage at age 65 doesn't extend to family members. Your spouse younger than age 65 would remain eligible for TRICARE Prime or TRICARE Select until they turn age 65 and become eligible for Medicare Part A and Part B.
What happens to my TRICARE when I turn 65?
Coverage under "regular" Tricare ends once the beneficiary becomes eligible for Medicare. For most people, that happens at age 65. In the three months before, during the month of or in the three months after you turn 65, you'll enroll in Medicare Parts A & B.Jan 24, 2022
What is the monthly cost for TRICARE for Life?
For an individual plan, you'll pay $12.50 per month or $150 annually. For a family plan, you'll pay $25.00 per month or $300 annually. The catastrophic cap will increase from $3,000 to $3,500. Your TRICARE Select enrollment fees will apply towards your catastrophic cap.Feb 15, 2022
Does TRICARE or Medicare pay first?
For active-duty military enrolled in Medicare, TRICARE pays first for Medicare- covered services or items, and Medicare pays second . For inactive-duty military enrolled in Medicare, Medicare pays first and TRICARE may pay second .
Does TRICARE for life cover what Medicare doesn t?
TRICARE will pay first for Medicare-covered services if you're on active duty. If TRICARE and Medicare cover the service, TRICARE will pay the Medicare deductible and coinsurance (if any). TRICARE will also pay for any services that it covers but Medicare does not.
How does tricare work?
How TRICARE works with other types of Medicare coverage 1 Medicare Advantage#N#TRICARE works with Medicare Advantage plans (Medicare Part C) in the same way that it works with Original Medicare (Medicare Part A and Part B) as described above.#N#Medicare Advantage plans offer the same benefits covered by Original Medicare, and some Medicare Advantage plans may also offer additional benefits such as dental, vision and hearing care, as well as prescription drug coverage. 2 Medicare Part D#N#TRICARE includes prescription drug coverage. In many cases, it isn’t necessary for TRICARE beneficiaries to enroll in a Medicare Part D prescription drug plan. 3 Medicare Supplement Insurance#N#TRICARE acts as supplemental coverage and picks up the cost of many of the same out-of-pocket Medicare costs as Medicare Supplement Insurance, such as Medicare coinsurance and deductibles. For this reason, it’s not typically necessary for TRICARE beneficiaries to enroll in a Medicare Supplement Insurance plan (also called Medigap).
Who is eligible for tricare?
Older members of the military, veterans and military retirees may be eligible for TRICARE, which is the health care program of the United States Department of Defense’s Military Health System. Americans who are over 65 years old or who have a qualifying disability are eligible for Medicare, the federal health insurance program.
What is tricare for life?
TRICARE For Life (TFL) is TRICARE’s optional health plan that is designed for military members and retirees who are also Medicare beneficiaries. In the U.S. and U.S. territories, Medicare serves as the primary coverage for people enrolled in both programs, and TRICARE offers secondary coverage.
How to contact Medicare Advantage?
For information about Medicare eligibility, benefits and the Medicare Advantage plan options available in your area, speak with a licensed insurance agent by calling. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 24 hours a day, 7 days a week.
What is accepting assignment?
A Medicare non-participating provider has not agreed to the Medicare-approved amount for their services, and they reserve the right to charge up to 15 percent more for covered services.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
Does Medicare Advantage cover prescriptions?
Medicare Advantage plans offer the same benefits covered by Original Medicare, and some Medicare Advantage plans may also offer additional benefits such as dental, vision and hearing care, as well as prescription drug coverage. Medicare Part D. TRICARE includes prescription drug coverage.
Your Benefits
TRICARE covers most inpatient and outpatient care that is medically necessaryTo be medically necessary means it is appropriate, reasonable, and adequate for your condition.. >>See what's covered
Out-of-Pocket Costs
Your health care costs are based on your sponsor's status (active duty or retired) and which health plan option you are using.
How old do you have to be to get tricare?
Age 65 or older. Under age 65 with certain disabilities. ( If you have Medicare due to a disability, you can continue your TRICARE Prime enrollment [if you qualify]. If you do, your Prime enrollment fees are waived. You can also get a refund for any Prime enrollment fees that you paid.
What is Medicare Advantage?
Medicare Advantage (Medicare Part C) When using Original Medicare you may get health care services from any Medicare participating or Medicare Non-participating provider, regardless of their specialty. Medicare Part A is hospital insurance Which is financed by payroll deductions when you are or were working.
Does tricare cover life?
TRICARE For Life. When you have Medicare Parts A and B, you automatically receive coverage from TRICARE For Life. There are no enrollment forms or enrollment fees for TRICARE For Life. Medicare is your primary payer.
Does Medicare Advantage cover pharmacy?
Medicare Advantage plans provide all of your Part A and Part B services and usually Part D pharmacy coverage. You may pay a plan premium each month in addition to your Medicare Part B premium. You must get all your health care services from the Medicare Advantage plan’s network of providers.
Does Medigap pay out of pocket?
You pay a premium each month. Medigap pays your out-of-pocket costs in Original Medicare. If you’re eligible for TRICARE and have Medicare Part A and Part B, TRICARE For Life provides wraparound coverage which pays your out-of-pocket costs in Original Medicare for TRICARE covered services.
When do you have to sign up for Medicare Part A and B?
You must sign up for Medicare Part A & B. Sign-up for Part B during your Medicare Initial Enrollment Period. To avoid a break in TRICARE coverage be sure to enroll no later than two months before you turn 65. If you enroll any later, your Part B effective date will be delayed and you will have a break in TRICARE coverage.
How old do you have to be to get Medicare?
You become eligible for Medicare Part A at age 65 if you or your spouse paid into Social Security for at least 40 quarters (at least ten years of work). You must have Medicare Part A and B in order to have TRICARE coverage when you are 65. Or you must have proof of your ineligibility for Medicare.
Do you have to have Medicare if you are 65?
Or you must have proof of your ineligibility for Medicare. If you’re 65, but have an active duty sponsor, you don’t have to have Medicare Part B until your sponsor is retired. Sign up before your sponsor retires to avoid a gap in TRICARE coverage.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What happens if a group health plan doesn't pay?
If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment. Medicare may pay based on what the group health plan paid, what the group health plan allowed, and what the doctor or health care provider charged on the claim.
What is a copayment?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. or a. deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.