96372 Therapeutic, prophylactic, or diagnostic injection (specify substance or drug); subcutaneous or intramuscular – Average fee amount $28 96374 – Therapeutic, prophylactic, or diagnostic injection (specify substance or drug); intravenous push, single or initial substance/drug – average fee amount – $50 – $60
Is 96372 covered by Medicaid?
NDCs will be the only ones Medicaid will cover for payment. A link to a list … the drug is possibly under a generic name. The claims …. Administration code ( 96372, 96373, 96374, 96375 and 96376) is provided at the same …
When to Bill 96372?
We always bill 96372 w/ office visit when injection was given with direct physician/other qualified health care professional; I work at urgent care facility. Hope this help. In Peds we always billed 96372 for rocephin no matter how many times the patient received it. The insurance always paid the claim. I work in a family physicians office.
When to use 96372?
The 96372 CPT code is to be billed for each injection performed on a patient. Modifier 59 should be used when the injection is a separate service from other treatments. Subsequent codes related to this code include: 96373 – therapeutic, prophylactic, and diagnostic substance by intra-arterial injections and infusions
How to Bill 96372 more than once?
- Initial injection med A (96374)
- Additional subsequent injection, meds B – Z (96375)
- Additional subsequent injections med A (96376), there must be a period of more than 30 minutes that has to pass between injections of same drug.

Is 96372 covered by Medicare?
A: Medicare requires the use of CPT code 96372 –Therapeutic, prophylactic, or diagnostic injection, specify substance or drug; subcutaneous or intramuscular for the administration of biologics.
What does CPT code 96372 pay?
CPT® code 96372: Injection of drug/substance under skin or into muscle | American Medical Association.
How Much Does Medicare pay for 90837?
$132.69What is the difference between the “facility rate” and “nonfacility rate” for telehealth services?CodeService2021 Facility Rate90832Psychotherapy 30-minutes$68.7490837Psychotherapy 60-minutes$132.6996132Neuropsych Test Eval$106.0896158Hlth Bhvr Intrv Indvl$58.971 more row•Dec 10, 2021
Is 96372 covered by Medicaid?
They advised that the injection code 96372 is a non payable and non allowable code.
How many times can you bill 96372?
The IM or SQ injection can be billed more than once or twice. If the drug is prepared and drawn up into two separate syringes and it is then administered in two individual injections in two distinct anatomic sites, you can bill two units of code 96372 (billing second unit with modifier 76).
Can you bill CPT 96372 with an office visit?
96372 CPT code reimbursement is allowed when the injection is performed alone or in conjunction with other procedures/services as allowed by NCCI.
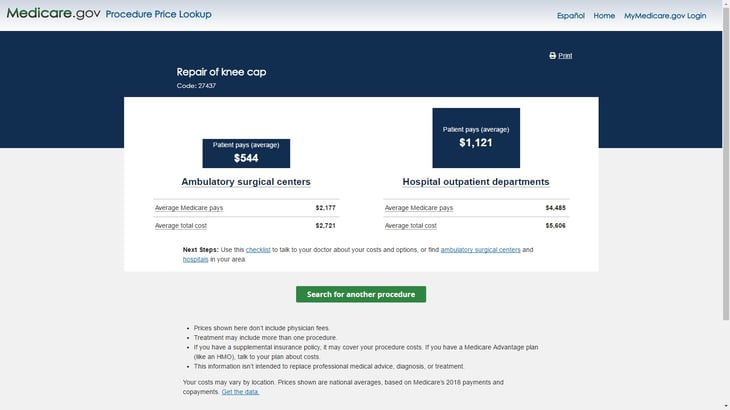
How do I calculate Medicare reimbursement for CPT codes?
You can search the MPFS on the federal Medicare website to find out the Medicare reimbursement rate for specific services, treatments or devices. Simply enter the HCPCS code and click “Search fees” to view Medicare's reimbursement rate for the given service or item.
What is the Medicare reimbursement rate?
roughly 80 percentAccording to the Centers for Medicare & Medicaid Services (CMS), Medicare's reimbursement rate on average is roughly 80 percent of the total bill. Not all types of health care providers are reimbursed at the same rate.
What is Medicare approved amount?
The approved amount, also known as the Medicare-approved amount, is the fee that Medicare sets as how much a provider or supplier should be paid for a particular service or item. Original Medicare also calls this assignment. See also: Take Assignment, Participating Provider, and Non-Participating Provider.
How do I bill for 2 injections?
If a provider wishes to report multiple injections (intramuscular or subcutaneous) of the same therapeutic medication, he or she may choose to report code 96372 (therapeutic, prophylactic, or diagnostic injection [specify substance or drug]). The number of administrations would be reported as the units of service.
Does Medicare pay for venipuncture?
If a venipuncture performed in the office setting requires the skill of a physician for diagnostic or therapeutic purposes, the performing physician can bill Medicare both for the collection – using CPT code 36410 – and for the lab work performed in-office.
How do you bill for injections?
The CPT code 96372 should be used–Therapeutic, prophylactic, or diagnostic injection.
Why is CPT 96372 not being paid?
Providers are not being paid for this injection administration code because it is being applied incorrectly, insurance companies say. Here’s why.
What is the purpose of 96372?
The primary intent of an injection as described by 96372 is generally to deliver a small volume of medication in a single shot. The substance is given directly by subcutaneous (sub-Q), intramuscular (IM), or intra-arterial (IA) routes, as opposed to an intravenous (IV) injection/push that requires a commitment of time.
What is the E/M code for immunotherapy?
Injections for allergen immunotherapy have their own administration codes, 95115-95117. Do not report 96365-96379 with any codes that describe a procedure of which IV push or infusion are a part. Hospitals may not report an E/M code in addition to 96372 or 96373 when the sole purpose of the visit is drug administration.
What is a procedure valued for reimbursement?
All procedures are valued for reimbursement to include an assessment of the patient at the encounter (vital signs, appearance of the patient, etc.). If a procedure is scheduled in advance of the encounter, the medical necessity for that procedure has already been determined and the treatment has already been decided.
Can you bill an E/M with an injection?
This is not possible with a scheduled injection performed by a nurse.
What is CPT 96372?
Across the country, in offices and facilities, coders are having trouble with CPT® 96372 Therapeutic, prophylactic, or diagnostic injection, specify substance, or drug; subcutaneous or intramuscular. As this code is applied incorrectly, providers are not being paid for this injection administration code.
What is the purpose of 96372?
The primary intent of an injection as described by 96372 is generally to deliver a small volume of medication in a single shot. The substance is given directly by subcutaneous (sub-Q), intramuscular (IM), or intra-arterial (IA) routes, as opposed to an intravenous (IV) injection/push that requires a commitment of time.
What is MBC billing?
Medical Billers and Coders (MBC) provides medical billing and coding services that ensure on-time and accurate billing. We understand the importance of entering the right information so there are no delays or denials on behalf of the insurance provider. To know more about our billing services, you can contact us at 888-357-3226 / [email protected]
What is the code for preventive medicine?
The Preventive Medicine codes (99381-99412, 99429) do not need Modifier 25 to indicate a significant, separately identifiable service when reported in addition to the diagnostic and therapeutic Injection service. The Preventive Medicine codes include routine services such as the ordering of immunizations or diagnostic procedures.
When an E/M service and an injection or infusion service are submitted for the same enrollee on the same?
When an E/M service and an Injection or Infusion service are submitted for the same enrollee on the same date of service , there is a presumption that the E/M service is part of the procedure unless the physician identifies the E/M service as a separately identifiable service.
Is E/M part of the procedure?
When an E/M service and a procedure are submitted for the same enrollee on the same date of service, there is a presumption that the E/M service is part of the procedure unless the physician identifies the E/M service as a separately identifiable service. Since the Injection procedure does not include the components of a Preventive Medicine E/M service, the Injection can be reported separately and the Preventive Medicine E/M code does not need a modifier to indicate it is distinct or separate from the Injection procedure.
Can 99211 be reimbursed?
E/M service code 99211 will not be reimbursed when submitted with a diagnostic or therapeutic Injection code, with or without Modifier 25. This very low service level code does not meet the requirement for ‘significant’ as defined by CPT, and therefore should not be submitted in addition to the procedure code for the Injection.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
How much will Medicare cost in 2021?
Most people don't pay a monthly premium for Part A (sometimes called " premium-free Part A "). If you buy Part A, you'll pay up to $471 each month in 2021. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $471. If you paid Medicare taxes for 30-39 quarters, the standard Part A premium is $259.
How long does a SNF benefit last?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. You must pay the inpatient hospital deductible for each benefit period. There's no limit to the number of benefit periods.
How much is the Part B premium for 91?
Part B premium. The standard Part B premium amount is $148.50 (or higher depending on your income). Part B deductible and coinsurance.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
What is periodic payment?
The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
When is Medicare paying for drugs?
Medicare has determined under Section 1861 (t) that these drugs may be paid when they are administered incident to a physician’s service and determined to be medically reasonable and necessary. Such determination of reasonable and necessary is currently left to the discretion of the Medicare Administrative Contractors (MACs). The documentation in the patient’s medical record must support the drugs as being medically reasonable and necessary.
What is the JB modifier for filgrastim?
J1442, Q5101 or Q5110: The subcutaneous or intravenous formulation of filgrastim needs to billed with the JA (intravenous) or JB (subcutaneous) modifier.
What is the HCPCS code for ustekinumab?
J3358: Effective September 23, 2016, IV ustekinumab (Stelara®) should be billed with HCPCS J3590 (OPPS: C9399 for dates of service (DOS) before 04/01/2017; C9487 for DOS from 04/01/2017 to 06/30/17, Q9989 for DOS from 07/01/2017-12/31/17 and J3358 for DOS 01/01/2018 and after) for the initial IV dose of Stelara® when used for Crohn’s disease and Ulcerative Colitis and each subsequent subcutaneous dose must be billed with J3357. This IV formulation is now FDA approved for Crohn’s disease and Ulcerative Colitis. On and after July 31, 2017, both the drug and administration should be billed on the same claim with no other drugs or administration to prevent inappropriate claim rejection.
What is the HCPCS code for octreotide acetate?
The subcutaneous or intravenous formulation of octreotide acetate is billed using HCPCS code J2354 with the JA (intravenous) or JB (subcutaneous) modifier.
What is the CPT code for chemotherapy?
The Current Procedural Terminology (CPT) codebook contains the following information and direction for the Chemotherapy and Other Highly Complex Drug or Highly Complex Biological Agent Administration CPT® codes: “Chemotherapy Administration codes 96401-96549 apply to parenteral administration of non-radionuclide anti-neoplastic drugs; and also to anti-neoplastic agents provided for treatment of non-cancer diagnoses (e.g. cyclophosphamide for auto-immune conditions) or to substances such as certain monoclonal antibody agents, and other biologic response modifiers. The highly complex infusion of chemotherapy or other drug or biologic agents requires physician or other qualified health care professional work and/or clinical staff monitoring well beyond that of therapeutic drug agents (96360-96379) because the incidence of severe adverse patient reactions are typically greater. These services can be provided by any physician or other qualified health care professional. Chemotherapy services are typically highly complex and require direct supervision for any or all purposes of patient assessment, provision of consent, safety oversight, and intraservice supervision of staff. Typically, such chemotherapy services require advanced practice training and competency for staff who provide these services; special considerations for preparation, dosage, or disposal; and commonly, these services entail significant patient risk and frequent monitoring. Examples are frequent changes in the infusion rate, prolonged presence of the nurse administering the solution for patient monitoring and infusion adjustments, and frequent conferring with the physician or other qualified health care professional about these issues. When performed to facilitate the infusion of injection, preparation of chemotherapy agent (s), highly complex agent (s), or other highly complex drugs is included and is not reported separately. To report infusions that do not require this level of complexity, see 96360-96379. Codes 96401-96402, 96409-96425, 96521-96523 are not intended to be reported by the individual physician or other qualified health care professional in the facility setting.”
When is the JW modifier not permitted?
A situation in which the JW modifier is not permitted is when the actual dose of the drug or biological administered is less than the billing unit. For example, one billing unit for a drug is equal to 10mg of the drug in a single use vial. A 7mg dose is administered to a patient while 3mg of the remaining drug is discarded. The 7mg dose is billed using one billing unit that represents 10mg on a single line item. The single line item of 1 unit would be processed for payment of the total 10mg of drug administered and discarded. Billing another unit on a separate line item with the JW modifier for the discarded 3mg of drug is not permitted because it would result in overpayment. Therefore, when the billing unit is equal to or greater than the total actual dose and the amount discarded , the use of the JW modifier is not permitted.
What is Section 1862 A?
Section 1862 (a) (1) (A) excludes expenses incurred for items or services which are not reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member