Every month without coverage, a penalty of 1% of the national base beneficiary premium is assessed, which will be about $33 in 2021. 1 The dollar amount of the penalty will change each year when the base premium changes.
How do you calculate Medicare penalty?
Your Initial Enrollment Period ended December 2016. You waited to sign up for Part B until March 2019 during the General Enrollment Period. Your coverage starts July 1, 2019. Your Part B premium penalty is 20% of the standard premium, and you’ll have to pay this penalty for as long as you have Part B.
Why is there a late enrollment penalty for Medicare?
Dec 21, 2021 · Every month without coverage, a penalty of 1% of the national base beneficiary premium is assessed, which will be about $33 in 2021. 1 The dollar amount of the penalty will change each year when ...
How do you calculate Medicare late enrollment penalty?
The late-enrollment penalty for Part B also is a 10% hike on premiums. But you get hit with another 10% extra for each 12-month period that passes after you're eligible to …
What is the penalty for not taking part B Medicare?
Part A late enrollment penalty. Some people have to buy Part A because they don't qualify for premium-free Part A. If you have to buy Part A, and you don't buy it when you're first eligible for Medicare, your monthly premium may go up 10%. You'll have to pay the higher premium for twice the number of years you didn't sign up.

How do I avoid Medicare Part B penalty?
How is the Medicare Part B penalty calculated?
Is there a limit on the Medicare Part B penalty?
Can Medicare penalties be waived?
Do I have to pay for Medicare Part B?
You pay a premium each month for Part B. Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these: Social Security. Railroad Retirement Board.
Can you drop Medicare Part B anytime?
How is Medicare late enrollment penalty calculated?
What is late enrollment penalty?
How do I fight Medicare penalty?
What will Irmaa be in 2021?
What happens if you don't get Part B?
If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B.
Do you pay late enrollment penalty for Part B?
And, the penalty increases the longer you go without Part B coverage. Usually, you don't pay a late enrollment penalty if you meet certain conditions that allow you to sign up for Part B during a Special Enrollment Period.
When does Part B start?
You waited to sign up for Part B until March 2019 during the General Enrollment Period. Your coverage starts July 1, 2019. Your Part B premium penalty is 20% of the standard premium, and you’ll have to pay this penalty for as long as you have Part B.
How much is the penalty for Part D in 2021?
Your penalty for 2021 would be 33 cents x 12 (for the 12 months of 2020 you weren’t covered), or $3.96.
Who is Amy Fontinelle?
Amy Fontinelle has more than 15 years of experience covering personal finance—insurance, home ownership, retirement planning, financial aid, budgeting, and credit cards—as well corporate finance and accounting, economics, and investing. In addition to Investopedia, she has written for Forbes Advisor, The Motley Fool, Credible, ...
Does Medicare have penalties for not following the rules?
The Bottom Line. Medicare imposes premium penalties on people who don’t follow the program’s health insurance coverage rules. You can avoid Part D penalties by signing up when you first become eligible. But not everyone needs Medicare at age 65.
Can you get Medicare at 65?
You can avoid Part D penalties by signing up when you first become eligible. But not everyone needs Medicare at age 65.
How long can you go without Medicare?
If you’re not ready to get Medicare yet, make sure you never go more than 63 days without Part D or creditable prescription drug coverage after your initial enrollment period is up.
When does Medicare Part D end?
Your initial enrollment period for Medicare starts three months before you turn 65 and ends three months after you turn 65.
How long does Medicare enrollment last?
Your initial enrollment period for Medicare starts three months before you turn 65 and ends three months after you turn 65. That means you have seven months, including your birthday month, to enroll penalty free. 1 If your birthday is in April, for example, your initial enrollment period runs from January 1 through July 31.
What happens if you don't buy Medicare?
If you have to buy Part A, and you don't buy it when you're first eligible for Medicare, your monthly premium may go up 10%. You'll have to pay the higher premium for twice the number of years you didn't sign up.
How long do you have to pay for Part A?
If you were eligible for Part A for 2 years but didn't sign up, you'll have to pay the higher premium for 4 years. Usually, you don't have to pay a penalty if you meet certain conditions that allow you to sign up for Part A during a special enrollment period.
Do you have to pay a penalty for a special enrollment?
Usually , you don't have to pay a penalty if you meet certain conditions that allow you to sign up for Part A during a special enrollment period. If you have limited income and resources, your state may help you pay for Part A, and/or Part B.
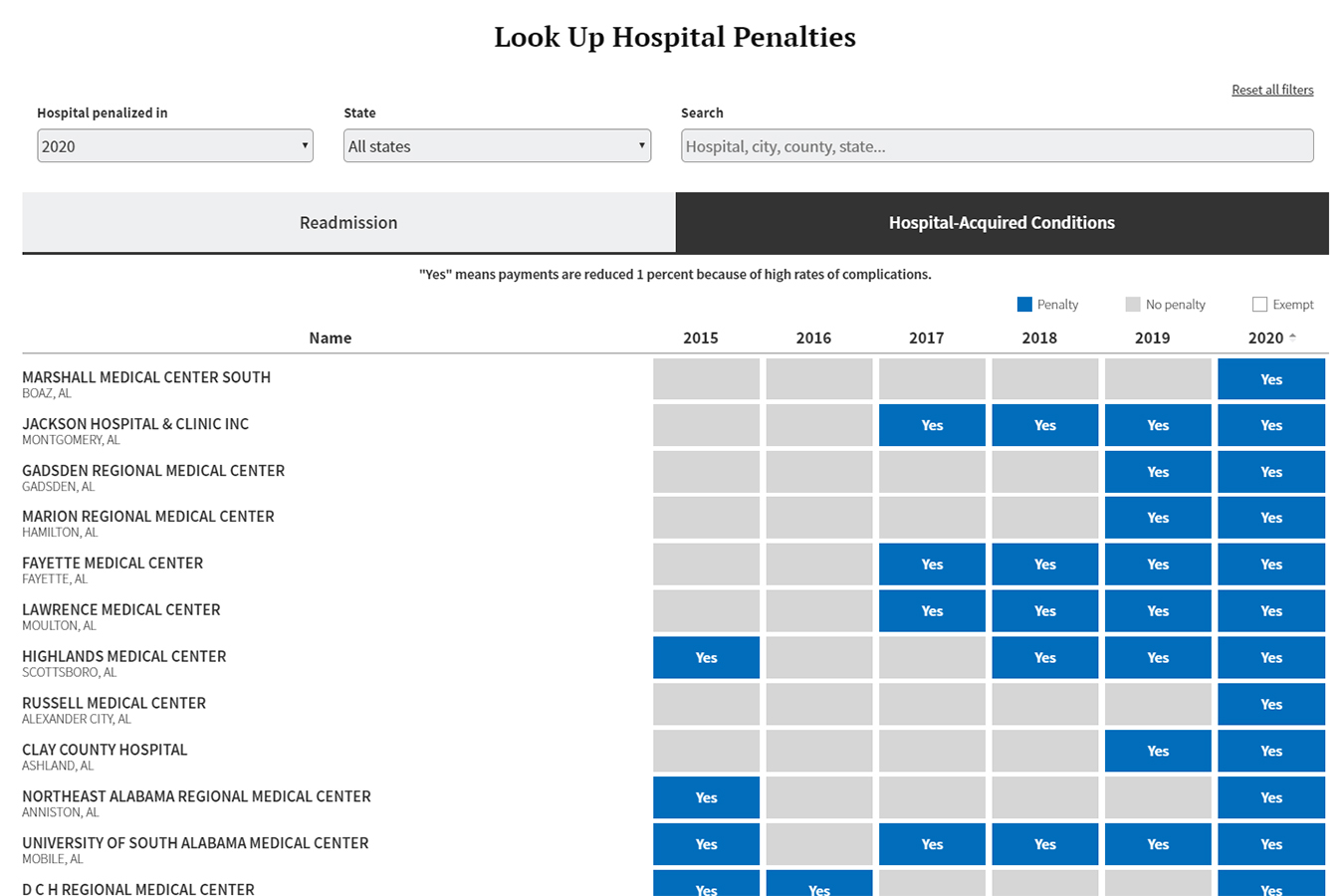
How much does Medicare cut for readmissions?
For the readmission penalties, Medicare cuts as much as 3 percent for each patient, although the average is generally much lower.
Why are Maryland hospitals exempt from Medicare penalties?
Maryland hospitals are exempted from penalties because that state has a separate payment arrangement with Medicare.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
Do you have to pay late enrollment penalty for Medicare?
In general, you'll have to pay this penalty for as long as you have a Medicare drug plan. The cost of the late enrollment penalty depends on how long you went without Part D or creditable prescription drug coverage. Learn more about the Part D late enrollment penalty.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
How much is the Part B premium for 91?
Part B premium. The standard Part B premium amount is $148.50 (or higher depending on your income). Part B deductible and coinsurance.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
What is the Medicare tax rate for 2021?
Together, these two income taxes are known as the Federal Insurance Contributions Act (FICA) tax. The 2021 Medicare tax rate is 2.9%. Typically, you’re responsible for paying half of this total Medicare tax amount (1.45%) and your employer is responsible for the other 1.45%.
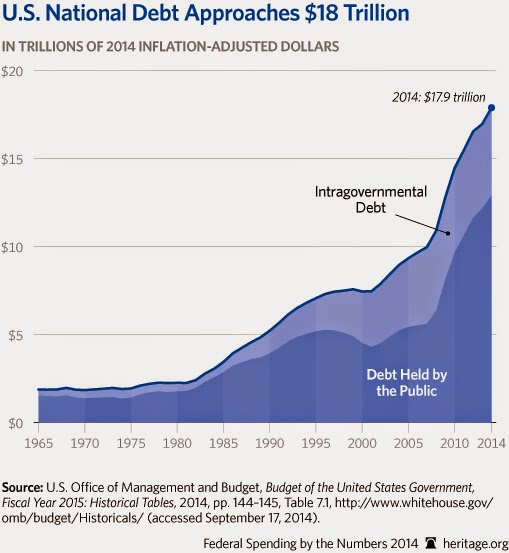
How is Medicare financed?
1-800-557-6059 | TTY 711, 24/7. Medicare is financed through two trust fund accounts held by the United States Treasury: Hospital Insurance Trust Fund. Supplementary Insurance Trust Fund. The funds in these trusts can only be used for Medicare.
What is Medicare Part A?
Medicare Part A premiums from people who are not eligible for premium-free Part A. The Hospital Insurance Trust Fund pays for Medicare Part A benefits and Medicare Program administration costs. It also pays for Medicare administration costs and fighting Medicare fraud and abuse.
How much Medicare tax do self employed pay?
Medicare taxes for the self-employed. Even if you are self-employed, the 2.9% Medicare tax applies. Typically, people who are self-employed pay a self-employment tax of 15.3% total – which includes the 2.9% Medicare tax – on the first $142,800 of net income in 2021. 2. The self-employed tax consists of two parts:
How is the Hospital Insurance Trust funded?
The Hospital Insurance Trust is largely funded by Medicare taxes paid by employees and employers , but is also funded by: The Hospital Insurance Trust Fund pays for Medicare Part A benefits and Medicare Program administration costs. It also pays for Medicare administration costs and fighting Medicare fraud and abuse.
When was the Affordable Care Act passed?
The Affordable Care Act (ACA) was passed in 2010 to help make health insurance available to more Americans. To aid in this effort, the ACA added an additional Medicare tax for high income earners.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
Does Medicare Part B and D have to be higher?
Learn more about what you may pay for Medicare, depending on your income. Medicare Part B and Part D require higher income earners to pay higher premiums for their plan.
Does Medicare require income to pay higher premiums?
Medicare Part B and Part D require higher income earners to pay higher premiums for their plan. If you have Part B and/or Part D benefits (which are optional), your premiums will be based in part on your reported income level from two years prior.
When will Medicare Part B and Part D be based on income?
If you have Part B and/or Part D benefits (which are optional), your premiums will be based in part on your reported income level from two years prior. This means that your Medicare Part B and Part D premiums in 2021 may be based on your reported income in 2019.
What is Medicare Part B based on?
Medicare Part B (medical insurance) premiums are based on your reported income from two years prior. The higher premiums based on income level are known as the Medicare Income-Related Monthly Adjustment Amount (IRMAA).
How much is the 2021 Medicare Part B deductible?
The 2021 Part B deductible is $203 per year. After you meet your deductible, you typically pay 20 percent of the Medicare-approved amount for qualified Medicare Part B services and devices. Medicare typically pays the other 80 percent of the cost, no matter what your income level may be.
What percentage of Medicare Part B is paid?
After you meet your deductible, you typically pay 20 percent of the Medicare-approved amount for qualified Medicare Part B services and devices. Medicare typically pays the other 80 percent of the cost, no matter what your income level may be.
Does Medicare Part D cover copayments?
There are some assistance programs that can help qualified lower-income beneficiaries afford their Medicare Part D prescription drug coverage. Part D plans are sold by private insurance companies, so additional costs such as copayment amounts and deductibles can vary from plan to plan.