Full Answer
Does Medicare Part a cover blood?
Medicare Part A (Hospital Insurance) covers blood you get as a hospital inpatient. Medicare Part B (Medical Insurance) covers blood you get as a hospital outpatient.
How often does Medicare cover blood tests?
Here are some of the conditions that are commonly screened through blood tests and how often you can have them done with Medicare coverage: Diabetes: once a year, or up to twice per year if you are higher risk (the A1C test will need to be repeated after 3 months) Heart disease: cholesterol, lipids, and triglycerides screening once every 5 years
How much does a blood test cost for Medicare Part B?
The cost of the blood test will be applied to your annual Part B deductible, which is $203 in 2021. If the laboratory is not Medicare-approved, there may also be a coinsurance payment required by the beneficiary.
How much does Medicare pay for blood transfusions?
After you have met your Part B deductible (and paid for the first three pints of blood if charged), Medicare Part B will pay 80% of the Medicare approved amount for blood transfusion and blood processing services for the rest of the calendar year.

How many units of blood does Medicare cover?
3 unitsPay the hospital costs for the first 3 units of blood you get in a calendar year. Donate the blood (or have someone else donate it for you)
How many pints of blood does Medicare pay for?
three pintsAs a Medicare beneficiary, though, there's a medical charge that might surprise you: the Medicare blood deductible. Under Medicare, you actually have to pay for (or donate) the first three pints of blood you use each calendar year.
Does Medicare cover pints of blood?
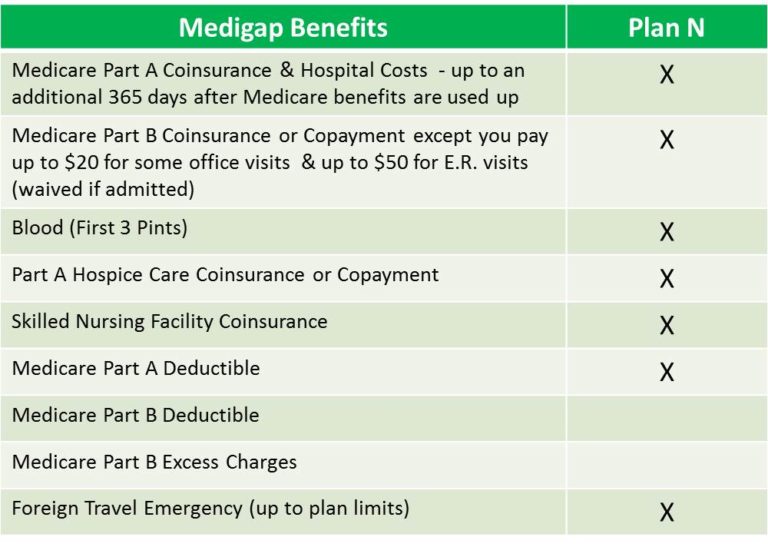
Medigap policies, also referred to as Medicare Supplement insurance, work with Original Medicare to help cover your out-of-pocket costs. All Medigap plans cover your costs for the first three pints of blood each year. Medigap also covers all or part of your copayments and coinsurance, depending on which plan you have.
Does Medicare cover complete blood count?
Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines. Examples would be screening blood tests to diagnose or manage a condition. Medicare Advantage, or Part C, plans also cover blood tests.
How much is in a unit of blood?
One unit of whole blood is roughly the equivalent of one pint. Blood makes up about seven percent of your body's weight. A newborn baby has about one cup of blood in his body. Giving blood will not decrease your strength.
What is the average cost of a blood transfusion?
Blood transfusions can cost a lot. A unit of blood usually costs about $200 to $300. There are added costs for storage and processing, as well as hospital and equipment fees. Costs can be much higher if the transfusion causes an infection or serious problem.
What is the blood deductible?
The amount of money for which the intermediary determined the beneficiary is liable for the blood deductible. A blood deductible amount applies to the first 3 pints of blood (or equivalent units; applies only to whole blood or packed red cells - not platelets, fibrinogen, plasma, etc. which are considered biologicals).
Why do blood transfusions cost so much?
As far as the cost to a patient for a transfusion, that has a price tag, too. Our expert Dr. Ge Bai explained hospitals have expenses for transfusions. It has to cover the cost of the blood, the pay for staff to administer it, and a host of other costs associated with getting blood into your veins.
How long does it take for 1 unit of blood transfusion?
A transfusion of one unit of red blood cells usually takes 2 to 4 hours. A transfusion of one unit of platelets takes about 30 to 60 minutes. Your nurse will monitor you carefully during your entire transfusion.
Does Medicare cover vitamin D blood test?
Under changes to the Medicare benefits schedule, only high-risk patients will get a rebate when they get vitamin D levels screened. Eligible patients include those with deeply pigmented skin, osteoporosis or those with chronic lack of sun exposure.
What lab can I use with Medicare?
Medicare will pay for clinical diagnostic lab tests that your doctor orders if they are medically necessary. Typically, you will not have to pay anything for the tests. Lab tests could include urinalysis, blood tests, tests on tissue specimens and screening tests.
What blood tests are covered under preventive care?
Preventive plans include various tests such as a blood test for sugar and cholesterol, pressure monitoring, cancer screening, Pap smear, HIV and genetic testing.
What part of Medicare covers blood tests?
If the blood test is ordered while receiving inpatient care at a hospital or skilled nursing facility, it will be covered under Medicare Part A (ho...
How much does a blood test cost?
If conducted in an inpatient care setting, the cost of the testing is subject to the Medicare Part A deductible, which is $1,364 per benefit period...
What blood tests are covered under Medicare?
Some of the more common types of blood tests that are covered by Original Medicare include Diabetes, Prostate cancer, Cardiovascular disease, Hepat...
What does Medicare pay for blood transfusions?
Medicare’s coverage of blood transfusions may depend partly upon where you receive the blood transfusion and where the health-care provider gets the blood.
Who orders blood transfusions?
That is, a licensed doctor or other authorized health-care provider orders the transfusion, and Medicare agrees the care is necessary and proper. The blood transfusion and/or blood-related services are delivered by a health-care provider who accepts Medicare assignment.
Does Medicare Advantage cover hospice?
(The exception is that Part A, not your Medicare Advantage plan covers hospice benefits.)
Do you have to pay for blood in a hospital?
Sometimes the hospital or skilled nursing facility gets blood from a blood bank at no charge. In this case, you won’t have to pay for the blood or replace it. If the hospital or skilled nursing facility has to buy blood for you, you must either pay the hospital costs for the first three units of blood you receive during the calendar year or have the blood donated.
Do you have to pay for the first three pints of blood?
If you receive blood from a donor or from a blood bank that does not charge for the blood, you will not have to pay for the first three pints of blood. You may be responsible for a copayment of the blood processing services. After you have met your Part B deductible (and paid for the first three pints of blood if charged), ...
How much does a blood test cost?
The costs are based on the particular test, your location, and the lab used. Tests can run from a few dollars to thousands of dollars. That’s why it’s important to check that your test is covered before you have it done.
How often does Medicare cover mammograms?
once a year if you meet criteria. *Medicare covers diagnostic mammograms more often if your doctor orders them. You are responsible for the 20 percent coinsurance cost. Other nonlaboratory diagnostic screenings Medicare covers include X-rays, PET scans, MRI, EKG, and CT scans.
What is the purpose of blood test?
Blood tests are an important diagnostic tool doctors use to screen for risk factors and monitor health conditions. A blood test is generally a simple procedure to measure how your body is functioning and find any early warning signs. Medicare covers many types of blood tests. Trusted Source.
What is Medicare Part A?
Medicare Part A offers coverage for medically necessary blood tests. Tests can be ordered by a physician for inpatient hospital, skilled nursing, hospice, home health, and other related covered services. Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines.
How much is Medicare Part B 2021?
You have to meet your annual deductible for this coverage as well. In 2021, the deductible is $203 for most people. Remember, you also have to pay your monthly Part B premium, which is $148.50 in 2021 for most beneficiaries.
Does Medigap cover out of pocket costs?
Medigap (Medicare supplemental insurance) plans can help pay for some out-of-pocket costs like coinsurance, deductibles, or copayments of covered screenings and other diagnostic tests.
Does Medicare cover 20 percent coinsurance?
You have to pay your 20 percent coinsurance as well as your deductible and any copays. Remember to go to providers that accept assignment to avoid charges Medicare won’t cover. Helpful links and tools. Medicare offers a tool you can use to check which tests are covered.
What is a copayment in Medicare?
copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage.
How to find out how much a test is?
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like: 1 Other insurance you may have 2 How much your doctor charges 3 Whether your doctor accepts assignment 4 The type of facility 5 Where you get your test, item, or service
How many blood tests are required for diabetes?
Diabetes – Two screenings per year with a referral or by meeting qualifying risk factors (blood sugar test strips for people with diabetes are also covered by Part B)
What happens if a lab is not Medicare approved?
If the laboratory is not Medicare-approved, there may also be a coinsurance payment required by the beneficiary.
How much is Medicare Part A deductible for 2021?
If conducted in an inpatient care setting, the cost of the testing is subject to the Medicare Part A deductible, which is $1,484 per benefit period in 2021.
Is a blood test covered by Medicare?
If the blood test is ordered while receiving inpatient care at a hospital or skilled nursing facility, it will be covered under Medicare Part A (hospital insurance).
Does Medicare Part C cover everything?
Medicare Advantage plans (Medicare Part C) are required to cover everything that is covered by Original Medicare, so the same coverage rules detailed above will apply.
Does Medicare Cover Blood Tests?
Medicare may cover blood tests in certain situations. Learn about how the different parts of Medicare cover blood tests and find a plan with the coverage you need.
Why is blood testing important?
Blood tests play a crucial role in the diagnosis, monitoring and treatment of a large number of diseases. Many patients and doctors rely on blood test results to create a holistic treatment plan geared toward overall wellness, but blood tests can also be vital when determining whether a current treatment is effective or not.
Is blood testing painless?
Blood testing is typically a quick and virtually painless procedure , and in just one visit, a relatively small amount of blood can provide a wealth of knowledge to healthcare providers.
Does Medicare cover blood work?
Aside from simple and routine blood testing, Medicare benefits also offer coverage for a range of associated diagnostic tests, including urinalysis, tissue testing and screenings for certain diseases when a medical order has been provided.
Is blood testing covered by Medicare?
In the vast majority of cases, blood testing is covered by Medicare Part B. Part B (Medical Insurance) provides benefits for medically necessary care administered in a physician’s office or in an outpatient clinical setting.
Can Medicare provide blood tests?
It’s worth noting that some blood tests can provide improper readings due to medications, so always clarify with your physician what medications to take and which to avoid prior to having your blood drawn. Medicare Provides For More Than Just Blood Testing.
Does Medicare cover lab testing?
It’s important to make this distinction because Medicare benefits often aren’t available for lab testing that a patient has sought out on his or her own. Medicare Part A (Hospital Insurance) may also provide coverage for blood testing when such tests are administered in a hospital or skilled nursing facility setting.
Can you get diagnostic tests with Medicare?
This essentially means that Medicare recipients are able to receive diagnostic services for almost any illness with a doctor ’s orders as long as the testing is medically necessary and carried out at a Medicare-ap proved facility.
How Much Do Blood Tests Cost With Medicare?
Beneficiaries typically do not pay anything for these blood tests as long as they are performed by a Medicare-approved health care provider.
How often does Medicare cover diabetes?
Diabetes – Medicare covers a blood test for diabetes once per year, or up to twice per year for high-risk individuals who have risk factors such as a history of high blood pressure or hypertension, a history of abnormal cholesterol or triglyceride levels, a history of high blood sugar or obesity.
What is Medicare Part B?
Medicare Part B covers clinical diagnostic lab tests such as blood tests, tissue specimen tests, screening tests and urinalysis when your doctor says they’re medically necessary to diagnose or treat a health condition.
Do you have to pay 20% coinsurance for blood work?
However, if more frequent blood tests are needed due to your risk factors or health condition, you may be required to pay a 20% coinsurance cost of the Medicare-approved amount after you meet your annual Part B deductible.
Does Medicare cover alcohol screening?
Medicare also covers screenings for alcohol and substance abuse and obesity.
Does Medicare cover blood tests?
Medicare covers blood tests for diabetes, heart disease, hepatitis, various types of cancer and more. Learn what blood tests Medicare pays for, and find out how much you can expect to pay.
How often does Medicare cover fecal occult blood test?
Fecal occult blood test. Medicare covers a fecal occult blood test once every 12 months for people aged 50 years or above. The test checks for blood in the stool that a person cannot see with the naked eye. If the result is positive, it may indicate that some part of the digestive tract is bleeding.
How often does Medicare cover lipoprotein?
Medicare covers a lipoprotein panel every 5 years. This test helps show whether or not a person is at risk of heart disease.
What is Medicare Advantage?
Medicare Advantage, or Medicare Part C, offers an alternative to Medicare parts A, B, and D. Medicare Advantage consists of Medicare-approved, private insurance companies that must follow the guidelines and rules of Medicare. Like parts A and B, Medicare Advantage plans cover the costs of blood work and other tests.
What is a coinsurance for Medicare?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
How much is a diagnostic test deductible?
For a diagnostic test, such as an X-ray, an individual will still pay 20% of the cost. The Part B annual deductible of $203 also applies.
Does Medicare cover blood work?
In some cases, Medicare Part A will cover the costs of blood work. Typically, a hospital or care facility will bill Part A when the person is staying within the facility. Medicare consists of three main parts: Part A: This is hospitalization insurance, which covers blood tests and other diagnostic laboratory tests that a doctor orders ...
Does Medicare Advantage cover copayments?
A person with Medicare Advantage may be responsible for copayments and coinsurance. These costs vary among plans. Someone with a Medicare Advantage plan may also need to go to an in-network laboratory to get lower costs.
How Often Does Medicare Pay for Blood Work?
Medicare pays for medically necessary blood work a doctor orders, as well as screening laboratory testing. Medicare may limit how often you can have these tests and the amount they pay. Examples include:
Does Medicare Part B Cover Lab Tests?
Medicare Part B will cover medically necessary laboratory tests, provided your doctor orders the test, and a Medicare-approved lab runs the test. Part B is the Medicare portion that covers medical services, including doctor’s visits.
Does Medicare Cover LabCorp or Quest?
Medicare covers medically necessary lab tests from LabCorp and Quest. These are two large laboratories that provide outpatient laboratory testing.
