Is counseling covered by Medicaid?
Clinical psychologists diagnose and treat mental, emotional, and behavioral disorders – and are one of the health care providers covered by Medicare Part B. Coverage: Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs.
Is EMDR covered by Medicare?
Medicare reimbursement rates for psychologists have been falling steadily for years. In 2001, Medicare paid $102 for a 45-minute psychotherapy session (the most common mental health service). Today, the program pays just $84.74 for the same service, a more than 30 percent decline, adjusted for inflation.
Does Medicare cover psychotherapy?
Jul 22, 2019 · Texas – TX. $90-$110. Again, these are estimated rates for a typical 60 minute session for an entry-level mental health license. The city you practice in will have a larger impact on your insurance reimbursement rates for psychotherapy than the state you pick.
Does Medicaid cover therapy sessions?
You pay nothing for your yearly depression screening if your doctor or health care provider accepts assignment. After you meet the Part B deductible, you pay 20% of the Medicare-Approved Amount for visits to your doctor or other health care provider to diagnose or treat your condition. If you get your services in a hospital outpatient clinic or hospital outpatient department, you …

What percentage of Medicare beneficiaries have mental health issues?
Each year, about 26 percent of all Medicare beneficiaries experience some mental disorder, including cognitive disorders like Alzheimer's disease. Studies show that roughly 70 percent of older adults who meet diagnostic criteria for major depressive disorder or for anxiety disorder do not receive mental health treatment.
What is the primary provider of behavioral health services to Medicare beneficiaries?
Psychologists are the predominant provider of behavioral health services to Medicare beneficiaries, providing nearly half of outpatient psychotherapy services and 70 percent of inpatient psychotherapy services. Psychologists provide almost all mental health diagnostic, testing, and assessment services under Medicare.
Do psychologists bill Medicare?
Psychologists are the predominant provider of the few procedures for which they bill Medicare. Under Medicare's payment formula, a lower-paid specialty can have its payment rates lifted when higher practice expenses incurred by other specialties providing the same service are factored in.
Does Medicare cover psychologists?
The "rising tide" effect that occurs with practice expenses under Medicare's formula works for some specialties, but not psychologists. Psychologists bill only a small number of different services; the average psychologist bills only two Current Procedural Terminology (CPT) codes.
Do depressed primary care patients prefer psychotherapy to medication?
Despite this trend, depressed primary care patients seeking treatment prefer psychotherapy to medication by a two-to-one margin. The Practice Organization has been discussing psychologists' problems with the Medicare provider payment formula with the Centers for Medicare and Medicaid Services (CMS). Most recently, in October of 2014 the Practice ...
What factors affect insurance reimbursement rate for psychotherapy?
Factors that effect your insurance reimbursement rate for psychotherapy: Location, paying more for under-served locales and less for over-served locations. License, education, and specialization. Specialization. Consumer demand at the time of signing your contract.
Does insurance pay for mental health therapists?
In summary, some private insurance companies reimburse mental health therapists for far more than others. A great way to quickly learn which companies pay the most is to simply ask your colleagues about their experiences with different reimbursement rates for private insurance companies.
Does Medicare cover mental health?
Medicare doesn’t cover all licenses and is far more selective than Medicaid about which providers they will allow into their network. As a result, mental health reimbursement rates for Medicare are higher than Medicaid rates by a substantial margin.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. applies. If you get your services in a hospital outpatient clinic or hospital outpatient department, you may have to pay an additional. copayment.
What is a health care provider?
health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. to diagnose or treat your condition.
Do you pay for depression screening?
You pay nothing for your yearly depression screening if your doctor or health care provider accepts assignment. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
Most common benefits
The average salary for a psychologist is $95,294 per year in the United States. 2.8k salaries reported, updated at February 23, 2022.
Best-paid skills and qualifications for Psychologists
The jobs requiring this certification have increase by 21.23% since 2018. Psychologists with this certification earn +18.95% more than the average base salary, which is $95,294 per year.
How much should you be earning?
Get an estimated calculation of how much you should be earning and insight into your career options. See more details
Common questions about salaries for a Psychologist
If you’re unsure about what salary is appropriate for a psychologist position, visit Indeed's Salary Calculator to get a free, personalized pay range based on your location, industry and experience.
When is the 2019 Medicare Physician Fee Schedule released?
These provisions are part of the final rule on the 2019 Medicare Physician Fee Schedule and Quality Payment Program, released by CMS in early November. Highlights of the Final Rule include.
Does Medicare update fee schedules?
Back to Medicare. Medicare maintains and updates fee schedules for all health care related costs including physicians, ambulance services, clinical labs, and durable medical equipment. The Medicare Physician Fee Schedule is updated on an annual basis through the rule-making process.
How many different Medicaid programs are there?
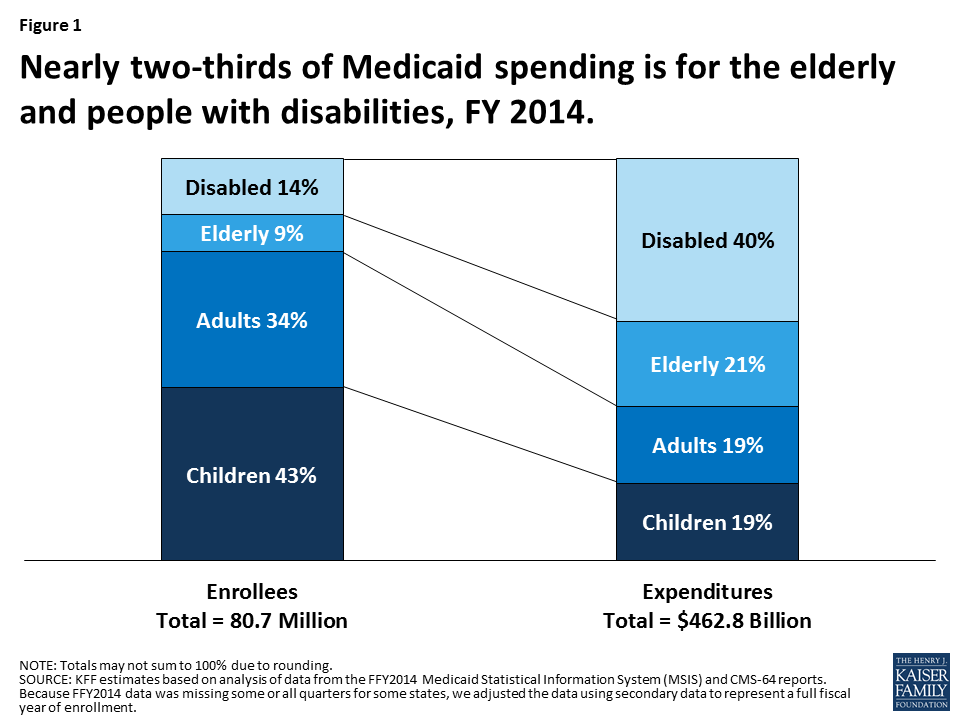
That means there are 56 different Medicaid programs.
What is Medicaid for low income?
Medicaid currently provides health care for certain low-income individuals. These include pregnant women, parents and children, people with severe disabilities and what's known as “dual eligibles,” low-income seniors and younger persons with disabilities who are enrolled in both Medicare and Medicaid. To determine eligibility for Medicaid, ...
What is CMS in healthcare?
State Medicaid agencies administer their own plans, but must meet federal guidelines set by the Centers for Medicare and Medicaid Services (CMS). CMS is an agency within the U.S. Department of Health and Human Services.
Does Medicaid cover psychological services?
No. States that offer psychological services in their Medicaid programs vary widely in what —and how much—they cover. While some states cover psychological treatment, for example, others cover only psychological evaluations.
Does Medicaid pay for psychologists?
Medicaid doesn’t give beneficiaries the money to pay for the care they receive. Instead, the program pays participating psychologists, physicians, pharmacists, hospitals, and other providers for the care beneficiaries receive.
Do you have to include psychological services in Medicaid?
While some benefits are mandatory under the federal guidelines, states are not required to include optional benefits, including psychological services, in their Medicaid plans. There is one exception, however. Some states contract with private companies to run their Medicaid programs.
Does Medicaid have to be managed by private companies?
Some states contract with private companies to run their Medicaid programs. These so-called Medicaid managed care programs are subject to a federal law that gives enrollees equal access to both mental health and substance use services and medical and surgical services.