Does Medicare Part B cover Reclast?
Under Medicare Part B, benefit recipients may be able to have the cost of Reclast covered when certain criteria are met. If injections are deemed medically necessary and administered by a medical professional in an outpatient setting, your Part B coverage may help pay for Reclast.
Does insurance cover Reclast infusions?
As long as medically necessary, the infusion will be covered by insurance. Be sure to choose a doctor within the network and always confirm with your insurance company before proceeding. As for Medicare, it will cover the costs of Reclast under Medicare Part B.
What does Part B of the Medicare card cover?
Part B covers things like: Clinical research Ambulance services Durable medical equipment (DME) Mental health Inpatient Getting a second opinion before surgery Limited outpatient prescription drugs
Does Medicare cover Reclast for osteoporosis?
Additionally, osteoporosis is a concern for post-menopausal women, individuals who smoke, those who have a family history of osteoporosis and people who are deficient in calcium. While many treatment options exist to combat osteoporosis, many Medicare recipients find relief from symptoms through Reclast. What is Reclast?
Does Medicare Part B pay for Reclast infusions?
Under Medicare Part B, benefit recipients may be able to have the cost of Reclast covered when certain criteria are met. If injections are deemed medically necessary and administered by a medical professional in an outpatient setting, your Part B coverage may help pay for Reclast.
Is Reclast paid for by Medicare?
Do Medicare prescription drug plans cover Reclast? No. In general, Medicare prescription drug plans (Part D) do not cover this drug.
What is the average cost of Reclast infusion?
The cost for Reclast intravenous solution (5 mg/100 mL) is around $1,151 for a supply of 100 milliliters, depending on the pharmacy you visit. Prices are for cash paying customers only and are not valid with insurance plans. A generic version of Reclast is available, see zoledronic acid prices.
Are infusions covered under Part B Medicare?
Here are some examples of Part B-covered drugs: Drugs used with an item of durable medical equipment (DME): Medicare covers drugs infused through DME, like an infusion pump or a nebulizer, if the drug used with the pump is reasonable and necessary.
What osteoporosis drugs are covered by Medicare?
Original Medicare typically covers osteoporosis injectable drugs like Prolia and a home health nurse visit to inject the drug if you meet certain eligibility requirements:You must be a woman.You must be eligible for Medicare Part B and have paid your premium.More items...•
Is there a generic drug for Reclast?
Reclast (zoledronic acid) is an expensive drug used to treat Paget's disease and osteoporosis in women. It is less popular than comparable drugs. There are currently no generic alternatives to Reclast.
Is Reclast Better than Prolia?
In a small study with 107 participants, people who received Prolia and those who got Reclast saw similar improvements in their bone mineral density (BMD), a measure of bone health. A larger study compared the drugs to each other, focusing primarily on the risk of serious infections, heart disease, or bone fractures.
Which is better Fosamax or Reclast?
Fosamax (alendronate) is a first-choice treatment for osteoporosis, but taking it can be a hassle. Prevents bone loss. Reclast (zoledronate) is a good choice for osteoporosis if you aren't able to take bisphosphonates by mouth. It is available as a generic, but you have to see a doctor to get each dose.
How much does Reclast improve bone density?
Researchers compared the results of Reclast versus Actonel in 833 patients over a year's time. Patients taking Actonel showed a bone mineral density (BMD) increase of 2.7%, while those taking the Reclast showed increased BMD of over 4%.
What drugs does Medicare Part B pay for?
Drugs that are covered by Medicare Part B include the following.Certain Vaccines. ... Drugs That Are Used With Durable Medical Equipment. ... Certain Antigens. ... Injectable Osteoporosis Drugs. ... Erythropoiesis-Stimulating Agents. ... Oral Drugs for ESRD. ... Blood Clotting Factors. ... Immunosuppressive Drugs.More items...•
Does Medicare Part B cover IVIG infusions?
Medicare Part B is a medical benefit and allows coverage for intravenous immunoglobulin replacement therapy (IVIG) because it was typically administered in a hospital or facility setting.
Does Medicare pay for infusions?
Medicare also covers home infusion therapy services, like nursing visits, caregiver training, and patient monitoring. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
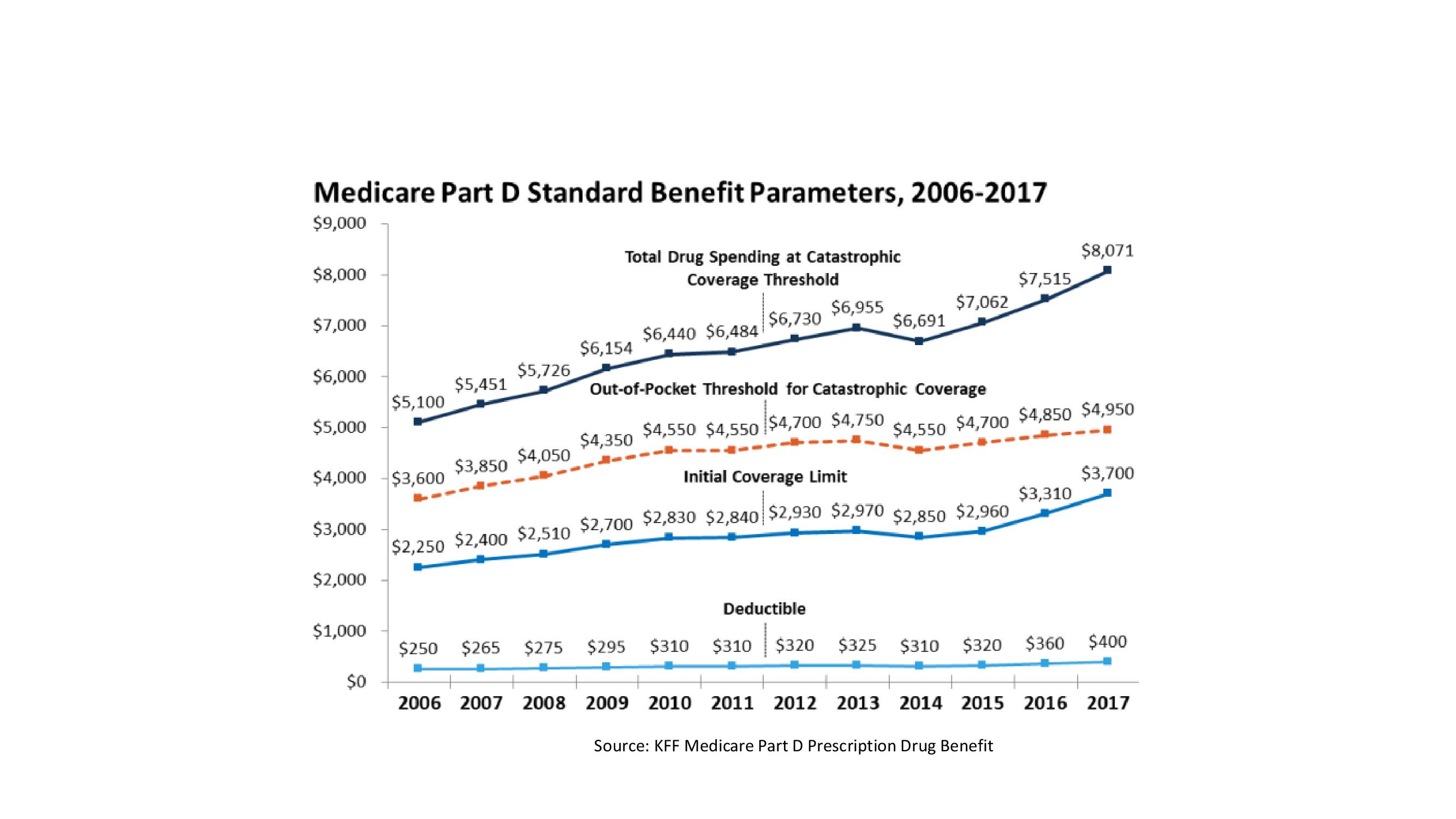
What is the post deductible stage?
After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug.
Does Medicare cover prescription drugs?
No. In general, Medicare prescription drug plans (Part D) do not cover this drug. Be sure to contact your specific plan to verify coverage information. A limited set of drugs administered in a doctor's office or hospital outpatient setting may be covered under Medical Insurance (Part B).
How often is reclast given?
Reclast is a prescription medication that contains the active ingredient Zoledronic Acid. It is given IV once every 1 to 2 years for the prevention and treatment of osteoporosis and Paget’s disease treatment. Reclast is a bisphosphonate medication that inhibits bone breakdown to reduce bone loss and risk of fracture.
What is a reclast?
Reclast ® is a prescription medication used to treat moderate to severe Ulcerative Colitis (UC) or Crohn’s Disease (CD) in adults.
How to compare Medicare Part D plans?
Compare Plans. Or call. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 24/7 to speak with a licensed insurance agent. You can also compare Part D prescription drug plans available where you live and enroll in a Medicare prescription drug plan online when you visit MyRxPlans.com.
What percentage of Medicare beneficiaries are MA-PDs?
Most Medicare Advantage beneficiaries ( 88 percent) are enrolled in MA-PDs. 2. Medicare prescription drugs plans each have their own formulary, or drug list, that details what prescription drugs are covered by the plan and how they are covered. Drug coverage may vary based on plan availability.
Can I take prescription medications with Medicare?
Speak to your doctor or healthcare provider about your specific healthcare needs, including your prescription medications. Only take medication as directed by your doctor. Coverage and costs of prescription medications will vary by Medicare plan. Not all plans are available in all areas.
Does Medicare cover reclast?
Because Medicare Advantage plans and Medicare Part D plans do not typically cover Reclast, you will likely be responsible for all costs for this drug if you have one of these types of Medicare coverage.
Can you get pregnant with reclast?
If you are able to get pregnant, a pregnancy test will be done prior to receiving Reclast to ensure you are not pregnant. Use birth control to prevent pregnancy during treatment with this drug and after your last dose.
How often should I give reclast?
Reclast infusion is an injection of zoledronic acid that is given over a short period of time, usually 15 to 30 minutes. It is sometimes used to treat osteoporosis and is usually administered once yearly. When used for treating Paget’s Disease, it may be administered more often, however. The medication helps strengthen and thicken bones and can also be used to treat patients with bone cancer or thinning bones due to cancer treatments. Both men and women can undergo Reclast infusion therapy. The dosage size will greatly depend on your medical condition.
What is reclast used for?
It’s commonly used to treat and prevent osteoporosis ...
How many fees are associated with an infusion?
There are often four to five different fees associated with each infusion session, so the estimates mentioned above will be much higher when the infusion is completed and billed. A patient should ask for a written breakdown of all possible charges associated with the infusion session so there will be no surprises.
Do you need follow up after reclast?
You will need follow-up appointments once the Reclast infusion therapy is completed. This will give the doctor a chance to see whether or not the treatment has worked. If you experience any negative side effects from Reclast infusion, you may need other medication or therapy to resolve these issues.
Does Medicare cover reclast?
Be sure to choose a doctor within the network and always confirm with your insurance company before proceeding. As for Medicare, it will cover the costs of Reclast under Medicare Part B.
What is Medicare Part B?
Medicare Part B pays for outpatient medical care, such as doctor visits, some home health services, some laboratory tests, some medications, and some medical equipment. (Hospital and skilled nursing facility stays are covered under Medicare Part A, as are some home health services.) If you qualify to get Medicare Part A, ...
How much is Medicare Part B 2021?
For Part B, you have to pay a monthly fee (called a premium ), which is usually taken out of your Social Security payment. For 2021, this fee is $148.50 per month. But if you have a higher than average personal income (over $85,000) or household income (over $176,000), you will have to pay a higher monthly premium for Medicare Part B.
How much does Medicare pay after paying $203?
After you pay $203 yourself, your benefits kick in. After that, Medicare will pay 80% of the cost of most Part B services, and you (or your Medigap policy) pay the other 20%. Finally, it’s important to know that there's a penalty for signing up late for Part B.
What is the Medicare approved amount?
Medicare decides what it will pay for any particular medical service. This is called the Medicare-approved amount. If your doctor is willing to accept what Medicare pays and won't charge you any more, they are said to "accept assignment.".
Why do people opt out of Medicare Part B?
Some people opt out of Medicare Part B because they still have coverage through union or employer health insurance. As long as your coverage is considered “creditable” you will not pay a penalty for signing up late.
What happens if you don't sign up for Medicare Part B?
If you don't sign up for Medicare Part B when you first become eligible (and you don’t have comparable coverage from an employer), your monthly fee may be higher than $148.50. You’ll pay a lifetime 10% penalty for every 12 months you delay your enrollment. Medical and other services.
Do you have to pay a co-payment for outpatient hospital services?
You must pay a co-payment for outpatient hospital services The exact amount varies depending on the service. Home health care. Medicare Part B pays for nurses and some therapists to provide occasional or part-time services in your home.
What is Part B?
Part B covers 2 types of services. Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.