Medicare Part D In 2018
| If you earned (single tax filing): | If you earned (joint tax return): | You’ll pay: |
| Up to $85,000 | Up to $170,000 | The plan premium |
| Over $85,000 to $107,000 | Over $170,000 to $214,000 | $13.30 + plan premium |
| Over $107,000 to $160,000 | Over $214,000 to $320,000 | $34.20 + plan premium |
| Over $160,000 to $214,000 | Over $320,000 to $428,000 | $55.20 + plan premium |
Full Answer
What is the monthly premium in Medicare Part D?
4 rows · Part D plans can't charge a deductible that's more than $405 in 2018, but you can find many ...
What is the average cost of Medicare Part D?
6 rows · Part D coverage varies by plan, but as mentioned above, there are caps in place that all plans ...
How to reduce Medicare Part D cost?
Feb 16, 2018 · Here’s what you need to know about Medicare Part D and the costs for 2018. Premiums. Unlike Medicare Part A and Part B, Part D does not have premiums set by the government, so costs can vary based on the plan you choose and where you live. This is partially due to the fact that private insurance companies provide Part D benefits and can set their own …
How to compare Medicare Part D drug plan costs?
Part D plans can't charge a deductible that's more than $405 in 2018, but you can find many ...
What were Medicare Part D premiums in 2018?
The average monthly premium for Medicare Advantage plans in 2018 was $12 and in 2019, the amount was $8. Prescription drug plan premiums also decreased slightly, from $26 in 2018 to $25 in Medicare costs 2019.Dec 30, 2021
What were Medicare Part D premiums in 2019?
2019 Medicare Part D premiums The average Part D plan premium in 2019 is around $41.21 per month, which is a 2 percent increase from the 2018 average premium. Part D plan premiums can also be subject to a Medicare IRMAA for higher income earners.
What is the cost of Part D for 2022?
Part D. The average monthly premium for Part coverage in 2022 will be $33, up from $31.47 this year. As with Part B premiums, higher earners pay extra (see chart below). While not everyone pays a deductible for Part D coverage — some plans don't have one — the maximum it can be is $480 in 2022 up from $445.Dec 31, 2021
What is the annual cost of Medicare Part D?
Want to make changes to your Part D coverage? Discuss your options with a licensed Medicare advisor at 1-844-309-3504. The maximum annual deductible in 2021 for Medicare Part D plans is $445, up from $435 in 2020.
What is the most popular Medicare Part D plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
Why is Medicare charging me for Part D?
If you have a higher income, you might pay more for your Medicare drug coverage. If your income is above a certain limit ($87,000 if you file individually or $174,000 if you're married and file jointly), you'll pay an extra amount in addition to your plan premium (sometimes called “Part D-IRMAA”).
Who has the cheapest Part D drug plan?
SilverScript Medicare Prescription Drug Plans Although costs vary by zip code, the average nationwide monthly premium cost of the SmartRX plan is only $7.08, making it the most affordable Medicare Part D plan on the market.
What is the max out of pocket for Medicare Part D?
3, out-of-pocket drug spending under Part D would be capped at $2,000, while under H.R. 19 and the Senate Finance bill, the cap would be set at $3,100 (both amounts exclude the value of the manufacturer price discount).Jul 23, 2021
Is Medicare Part D automatically deducted from Social Security?
If you receive Social Security retirement or disability benefits, your Medicare premiums can be automatically deducted. The premium amount will be taken out of your check before it's either sent to you or deposited.Dec 1, 2021
Do I need Medicare Part D if I don't take any drugs?
Even if you don't take drugs now, you should consider joining a Medicare drug plan or a Medicare Advantage Plan with drug coverage to avoid a penalty. You may be able to find a plan that meets your needs with little to no monthly premiums. 2. Enroll in Medicare drug coverage if you lose other creditable coverage.
Does Medicare Part D have copays?
No type of Medicare drug coverage may have a deductible more than $445 in 2021. Some plans don't charge a deductible. You pay copayments or coinsurance for your prescription drugs after you pay the deductible. You pay your share, and your plan pays its share for covered drugs.
How are Medicare Part D premiums calculated?
The income that counts is the adjusted gross income you reported plus other forms of tax-exempt income. Your additional premium is a percentage of the national base beneficiary premium $33.37 in 2022. If you are expected to pay IRMAA, SSA will notify you that you have a higher Part D premium.
How much is the penalty for Medicare Part B?
For Part B, the penalty is 10 percent of your premium (charged on top of the premium rate) for each 12-month period that you didn’t have Part B coverage when you could have. The penalty lasts for as long as you have Part B. Medicare Part B has other costs as well.
What is Medicare Part A?
Medicare Part A is the hospital portion, covering services related to hospital stays, skilled nursing facilities, nursing home care, hospice and home healthcare. Under the Affordable Care Act, Part A alone counts as minimum essential coverage, so if this is all you sign up for, you’ll meet the law’s requirements. Most people don’t pay a premium for Part A because it’s paid for via work-based taxes. If, over the course of your working life, you’ve accumulated 40 quarter credits, then you won’t pay a premium for Part A. This applies to nearly all enrollees, but some do pay a premium as follows:
How much is Medicare premium in 2017?
The standard premium in 2017 is $134 a month for new enrollees, but this number actually only applies to about 30 percent of Part B beneficiaries. The remaining majority pay about $109 a month – but this will change in 2018. The standard premium applies to:
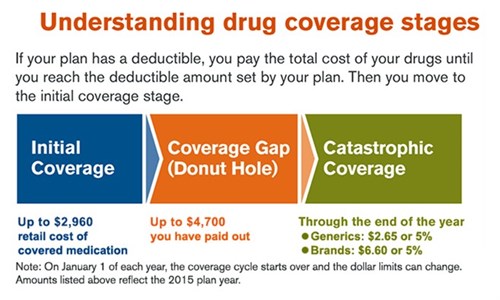
What is the donut hole in Medicare?
If you have Medicare Part D, then you may face a situation known as the donut hole (or coverage gap). This happens when you hit your plan’s initial coverage limit ($3,750 in 2018) but still need to buy prescriptions. Until you hit the catastrophic coverage limit – i.e., the other side of the “donut” – you’ll be responsible for the full cost of your medications.
Does Medicare Advantage cover Part B?
If you have Medicare Advantage, then you will pay the Part B premium as well as any premiums that your plan charges. Medicare Advantage must cover Part B services. Income thresholds will change in 2018.
What is the discount for generic drugs?
If you fall into the donut hole, you’ll get a discount on the cost of your prescriptions. In 2018, the discount is: 56 percent for generic medications (you pay 44 percent) 65 percent for brand name drugs (you pay 35 percent)
What is catastrophic limit?
This will effectively close the coverage gap. As it stands, the catastrophic limit prevents you from paying higher prescription drug costs forever. Once you hit the catastrophic limit ($5,000 in 2018), you’ll only be responsible for about 5 percent of the cost of your medications for the rest of your plan year.
What is Medicare Part D?
Prescription drug coverage, or Medicare Part D, is a relatively new feature of Medicare, but millions of seniors take advantage of the program to help lower their prescription drug costs. Here’s what you need to know about Medicare Part D and the costs for 2018.
How long do you have to enroll in Part D?
If you want to enroll in Part D coverage, make sure you do it at the right time: the seven-month period around your 65 th birthday month, including the three months leading up to it. If not, you could be penalized for signing up 63 days or more after your Initial Enrollment Period is over. If you don’t sign up during your Initial Enrollment Period, you will have to wait for the Fall Open Enrollment Period, which is October 15 – December 7, and you could be penalized.
What is the coverage gap for prescription drugs?
Once your out-of-pocket drug costs have reached $3,750, you fall into the coverage gap, also known as the donut hole. This means your plan stops paying for your prescription drugs until you reach catastrophic coverage. For 2018, catastrophic coverage begins once your out-of-pocket expenses have reached $5,000. Until you reach that, there are coverage gap discounts available to you: in 2018, name brand drugs will be discounted 65% and generic drugs will be discounted 56%. All payments (including discounts) will count toward your out-of-pocket costs and help you reach catastrophic coverage.
Do Part D plans require copays?
Copays and coinsurance are also typical under Part D plans. Some plans require you to pay a certain percentage of prescription drug costs (coinsurance), while others charge a fixed dollar amount (copayment). Prescription drug costs also depend on whether the drug is name brand or generic.
Summary
This analysis presents findings on Medicare Part D enrollment, premiums, and cost sharing in 2018 and key trends over time, based on data from the Centers for Medicare & Medicaid Services (CMS).
Findings
More than 43 million Medicare beneficiaries, or 72 percent of all Medicare beneficiaries nationwide, are enrolled in Part D plans.
Methodology
This analysis focuses on the Medicare Part D marketplace in 2018 and trends over time. Data on Part D plan availability, enrollment, and premiums were collected primarily from a set of data files released by the CMS on a regular basis:
How much is Medicare Part D deductible?
Medicare Part D offers a standard prescription drug benefit with a 2017 deductible of $400 and an average estimated monthly premium of $35.
How much is Medicare Part C?
Part C ($203.0 billion gross spending in 2018) Medicare Part C, the Medicare Advantage Program, pays plans a capitated monthly payment to provide all Part A and B services, and Part D services if offered by the plan.
What is Medicare Part A?
Medicare Part A pays for inpatient hospital, skilled nursing facility, home health related to a hospital stay, and hospice care. Part A financing comes primarily from a 2.9 percent payroll tax paid by both employees and employers.
What is the FY 2018 budget?
The FY 2018 Budget reflects the President’s commitment to preserve Medicare and does not include direct Medicare cuts. The Budget repeals the Independent Payment Advisory Board, commits to improving the Medicare appeals process, and supports efforts to limit defensive medicine as a part of a larger medical liability reform effort.
What is the repeal of the Independent Payment Advisory Board?
Repeal the Independent Payment Advisory Board: The Budget proposes to repeal the Independent Payment Advisory Board, created by Section 3403 of the Affordable Care Act, and all amendments thereto. All remaining unobligated administrative funds would be rescinded.
7.6 billion in costs over 10 years]
What is medical liability reform?
Medical Liability Reform: The Budget includes a set of proposals for medical liability reform. This initiative will reduce Federal spending on healthcare, including by curbing the provision of unnecessary services in Medicare.
How many people are on Medicare Advantage in 2018?
In 2018, Medicare Advantage enrollment will total approximately 20.8 million, or approximately 38 percent of all Medicare beneficiaries. Centers for Medicare and Medicaid Services (CMS) data confirm that 99 percent of Medicare beneficiaries will have access to at least one Medicare Advantage plan in 2018.
How much is Medicare Part A deductible?
The Medicare Part A annual inpatient hospital deductible that beneficiaries pay when admitted to the hospital will be $1,340 per benefit period in 2018, an increase of $24 from $1,316 in 2017. The Part A deductible covers beneficiaries’ share of costs for the first 60 days of Medicare-covered inpatient hospital care in a benefit period.
What is the deductible for Medicare Part B?
The annual deductible for all Medicare Part B beneficiaries will be $183 in 2018, the same annual deductible in 2017. Premiums and deductibles for Medicare Advantage and Medicare Prescription Drug plans are already finalized and are unaffected by this announcement. Since 2007, beneficiaries with higher incomes have paid higher Medicare Part B ...
What is the Medicare Part B premium?
Medicare Part B Premiums/Deductibles. Medicare Part B covers physician services, outpatient hospital services, certain home health services, durable medical equipment, and other items. The standard monthly premium for Medicare Part B enrollees will be $134 for 2018, the same amount as in 2017.
What is Medicare Part A?
Medicare Part A Premiums/Deductibles. Medicare Part A covers inpatient hospital, skilled nursing facility, and some home health care services. About 99 percent of Medicare beneficiaries do not have a Part A premium since they have at least 40 quarters of Medicare-covered employment. The Medicare Part A annual inpatient hospital deductible ...
How much will Social Security increase in 2018?
After several years of no or very small increases, Social Security benefits will increase by 2.0 percent in 2018 due to the Cost of Living adjustment.
How much is Medicare Part D 2021?
How much does Medicare Part D cost? As mentioned above, the average premium for Medicare Part D plans in 2021 is $41.64 per month. The table below shows the average premiums and deductibles for Medicare Part D plans in 2021 for each state. Learn more about Medicare Part D plans in your state.
What is Part D premium?
Your Part D deductible is the amount that you must spend out of your own pocket for covered drugs in a calendar year before the plan kicks in and begins providing coverage.
What is the difference between generic and brand name drugs?
Generic drugs are typically on lower tiers and cost less, while brand name drugs and specialty drugs are typically on higher tiers and cost more. Medicare Part D plans are sold by private insurance companies. These insurance companies are generally free to set their own premiums for the plans they sell.
Does Medicare Part D have coinsurance?
Medicare Part D plan costs in any particular area may depend partly on the cost of other plans being sold in the same area by competing carriers. Cost-sharing. Some Medicare Part D plans have deductibles and copayments or coinsurance. The cost of your Part D premium may depend on the amounts of coinsurance or copayments you pay with your plan, ...
What is the Medicare donut hole?
After 2020, Medicare Part D plans have a shrunken coverage gap, or “donut hole,” which represents a temporary limit on what the plan will cover for prescription drugs. You enter the Part D donut hole once you and your plan have spent a combined $4,130 on covered drugs in 2021.
Does Medicare Advantage cover Part A?
Medicare Advantage plans (also called Medicare Part C) provide all of the same coverage as Medicare Part A and Part B, and many plans include some additional benefits that Original Medicare doesn’t cover. Read additional medicare costs guides to learn more about Medicare costs and how they will affect you.
What is coinsurance and copayment?
Copayments and coinsurance are the amounts that you must pay once your plan’s coverage does begin. A copayment is usually a fixed dollar amount (such as $5) while coinsurance is most often a percentage of the cost (such as 20 percent). Plans might have different copayment or coinsurance amounts for each tier of drugs.
