Full Answer
What is the difference between CPT codes 95024 and 95004?
Code 95024 describe intracutaneous (intradermal) testing and include injection of small amounts of suspected allergens ?intradermally? (between the skin layers). This injection technique differs from scratch (on the skin) or percutaneous (just under the skin) techniques for delivering allergenic extracts, as described by code 95004.
How much does Medicare Part a cost?
Medicare costs at a glance. Most people don't pay a monthly premium for Part A (sometimes called " premium-free Part A "). If you buy Part A, you'll pay up to $437 each month. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $437. If you paid Medicare taxes for 30-39 quarters, the standard Part A premium is $240.
How do I Find my Medicare physician fee schedule?
If you requested these payments, learn how and when we’ll recoup them. To start your search, go to the Medicare Physician Fee Schedule Look-up Tool. To read more about the MPFS search tool, go to the MLN® booklet, How to Use The Searchable Medicare Physician Fee Schedule Booklet (PDF) .
How do I find Medicare reimbursement rates?
You can also find Medicare reimbursement rates if you know the CPT or HCPCS code for the service or item being billed and have access to the Medicare Physician Fee Schedule, which is essentially a master list of all reimbursement rates. The MPFS is updated on a quarterly basis to reflect the most recent changes to reimbursement rates.

Is allergy desensitization covered by Medicare?
Allergy shots may help improve symptoms of severe chronic allergies. Medicare Part B covers most of the cost of allergy shots if they're deemed medically necessary.
How do I bill a CPT 95004?
Interpretation of CPT codes: 95004 - 95078; use the code number which includes the number of tests which were performed and enter 1 unit for each test performed. For example, if 18 scratch tests are done, code 95004, 95017 or 95018 with 18 like services. If 36 are done, code 95004, 95017 or 95018 with 36 like services.
Does Medicare pay for allergy tests and shots?
Medicare Part B may cover allergy testing if you meet all the below criteria: Your physician must prescribe the allergy test. Your physician must be enrolled in Medicare and accept assignment. The test must be considered medically necessary, and your physician must provide documentation that says so.
What is the cost of allergen immunotherapy?
The Costs of Allergy Shots The allergy serum will typically cost around $100, and the preparation/administration costs can range from $20-100 per visit. Since these shots are dosed weekly, the annual cost can range from $1,000 to $4,000 per year.
Does 95004 need a modifier?
For scratch, puncture, and prick testing (code 95004) and a single intradermal test (code 95024), both types of testing may be reported when testing involves the same allergen and is performed on the same day. Hence, there is no need for modifier 59 if allregic testing through both the techniques are performed.
How do I bill for an allergy patch test?
95027 Intracutaneous (intradermal) tests, sequential and incremental, specify number of tests. Use this code when doing more than one ID test per antigen. (e.g. IDT) 95024 and 95027 may be billed at the same time.
What ICD 10 codes cover allergy testing?
ICD-10 Code for Encounter for allergy testing- Z01. 82- Codify by AAPC.
Is immunotherapy for allergies covered by insurance?
Allergy shots are typically covered by most health insurances, though this may vary depending on your specific plan. Even if your shots are covered by insurance, you still may have to pay a copay for each visit.
What is better allergy shots or drops?
Allergy drops can be very effective for treating allergic rhinitis due to ragweed, some grasses, and dust mites. They are as effective as allergy shots and are associated with fewer side effects. Currently there are only four types FDA-approved allergy drops, although other types are used as off-label drugs.
How much does oral immunotherapy cost?
The total OIT process with a new patient visit is typically $3,500 - $4,000.
How effective is allergy immunotherapy?
They usually improve during the first year of treatment, but the most noticeable improvement often happens during the second year. By the third year, most people are desensitized to the allergens contained in the shots — and no longer have significant allergic reactions to those substances.
How are allergy shots billed?
There are two types of charges billed for immunotherapy: a serum charge and an injection charge. Your serum is the first charge billed to your insurance. It is billed once a year. The amount made will provide you with enough serum for a years worth of immunotherapy.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
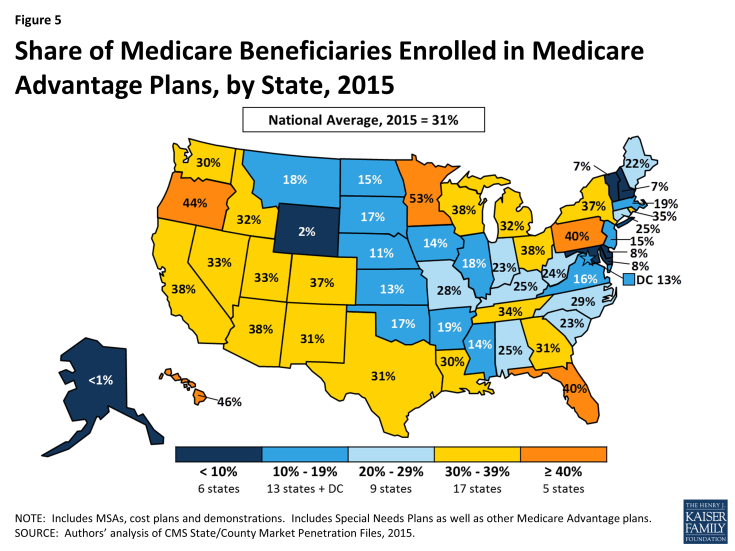
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.