Based on these relative value units (RVUs) and the current (2017) conversion factor, the Medicare allowance for code 99495 performed in a non-facility setting (e.g., a physician’s office) would be approximately $165.45. In a facility setting, the corresponding allowance is approximately $112.
What is the payment for CPT 99495 and 99596?
For CPT 99495, payment is increasing from $166.50 to $175.76. For CPT 99596, it will increase from $234.97 to $237.11. (Please note we use the non-facility national payment rate calculated with the 2020 conversion factor of $36.09 throughout this article, unless noted otherwise.)
How many units of CPT 99458 can be billed per calendar month?
(Unlike non-complex CCM, CMS did not explicitly state only two units of CPT 99458 can be billed each calendar month. This limitation, however, is implicit in CMS’ discussion regarding the RPM codes.)
Can I use code 99496 for a non-facility setting?
For code 99496 performed in a non-facility setting, the Medicare ... You can bill it as an office visit if documentation requirements for history, exam, and medical decision making are met should the
What is the difference between CPT 99490 and CPT g2058?
Effective January 1, 2020, a practitioner can bill CPT 99490 for the first 20 minutes of clinical staff time spent performing CCM activities in a given calendar month and can bill G2058 for the second and third 20-minute increments. Payment for CPT 99490 is $42.23, while each add-on code (up to two) pays $37.89.
What is the reimbursement rate for 99495?
$175.76/patient/monthCPT code 99495 – moderate medical complexity requiring a face-to-face visit within 14 days of discharge. Reimbursement rate – $175.76/patient/month.
Does Medicare pay for 99495?
You may provide CPT codes 99495 and 99496 via telehealth. Medicare pays for a limited number of Part B services you provide an eligible patient via a telecommunications system. Using eligible telehealth services substitutes for an in-person encounter.
How often can CPT 99495 be billed?
The codes can be billed only once per patient within 30 days after the original discharge for which a TCM code has been billed. Can more than one physician bill the TCM codes if they are caring for the same patient? No, these services may be billed by only one individual during the 30 day period after discharge.
What is procedure code 99495?
Code 99495 has the following requirements: Communication (direct contact, telephone, or electronic) with the patient or caregiver within two business days of discharge, Medical decision making of at least moderate complexity during the service period, A face-to-face visit within 14 days of discharge.
Can 99495 be billed as telehealth?
TCM is on Medicare's list of covered telehealth services. Per Current Procedural Terminology (CPT), CPT codes 99495 and 99496 include one face-to-face (but not necessarily in-person) visit that is not separately reportable.
Does CPT code 99495 need a modifier?
Per CCI the 99495 or 99496 cannot have a modifier 25 appended, which may be a hint that it is intended to be billed alone. But a 99396 for example can take a modifier 25. So the combination 99396-25 and 99495 may well be acceptable.
What is the difference between 99495 and 99496?
There are two codes used to reimburse for Transitional Care Management, CPT 99495 for moderate complexity patients and CPT 99596 for high complexity patients. A key difference between these codes is days after discharge in which a face-to-face visit is required, 14 days for CPT 99495 and 7 days for CPT 99496.
How do you bill transitional care management?
The two CPT codes used to report TCM services are:CPT code 99495 – moderate medical complexity requiring a face-to-face visit within 14 days of discharge.CPT code 99496 – high medical complexity requiring a face-to-face visit within seven days of discharge.
Do commercial payers pay for TCM?
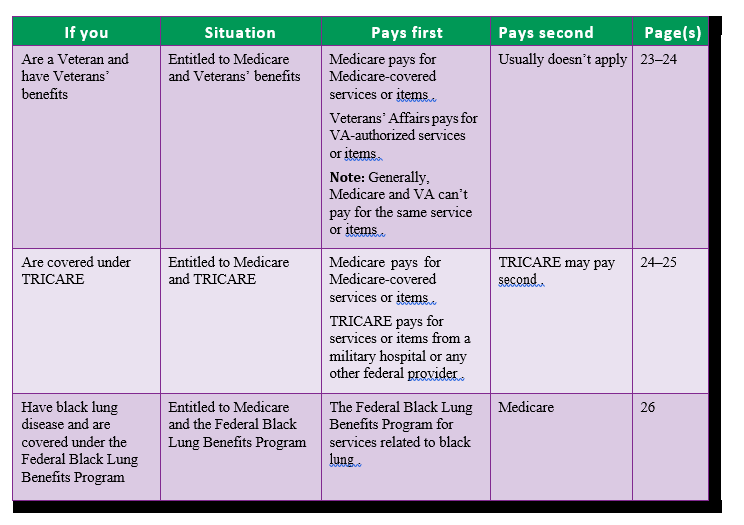
Other commercial payers and Medicare Advantage plans may pay for TCM. Commercial payers may have different payment rates for each code. TCM services rendered by a FQHC for a Medicare beneficiary are subject to co-insurance. 99495 Moderate complexity medical decision making during the service period.
Can transitional care management be billed after ER visit?
No. Emergency department visits are excluded. Patients are eligible for TCM services to help with the transition following discharge from inpatient or observation status, a nursing facility, or partial hospitalization.
Can you bill an office visit with a TCM?
You can bill it as an office visit if documentation requirements for history, exam, and medical decision making are met should the patient die or be re-admitted.
How often can you bill transitional care management?
The TCM service may be reported once during the entire 30-day period. If a surgeon is caring for the patient in the hospital after surgery, TCM cannot be billed for upon discharge as those services are part of the global period of the surgical procedure.
Who Is Eligible For Ccm?
For patients with multiple chronic conditions (two or more), who were expected to survive for more than 12 months, including time to die, and pose a significant threat to acute exacerbation, depression, or functional decline, CCM service is available.
Are Tcm Visits Only For Medicare?
Both Medicare and CPT do not exclude specific specialties in using the TCM codes. In addition, NPPs of an acceptable quality will be able to bill these services.
How Does Chronic Care Management Work?
A CCM doctor or non-physician provider conducts the care of the patient in this way, implementing a care team-based delivery system. Taking charge of care coordination and working directly with a patient are the tasks the clinical staff performs.
What Is Care Management Program Medicare?
You may be eligible for Medicare payment for the services of a health care provider if you have either one or more chronic conditions that are expected to last beyond one year and have chronic health issues. Furthermore, chronic health conditions such as arthritis and diabetes are managed by chronic care management.
What Is A Ccm Care Plan?
CCM, which offers care plans, describes what it covers s the CCM care plan include? Medical documentation is needed in order to help a healthcare provider keep track of a patient’s health at the CCM level. medical history, treatment lists, drug allergies, and medical records are part of the list.
Can Nurses Bill For Chronic Care Management?
Registered nurses can administer CCM under the care plan but patients must be supervised by physician, nurse practitioner or physician assistant professionals.
What Are The Requirements To Bill For Chronic Care Management?
The requirement is (1) two or more chronic conditions that will last at least one year (or until the patient dies). This plan should also have a written commitment (verbal or signed), and a copy provided to the patient as part of the process.
What is provider based outpatient?
provider-based outpatient department of a hospital is part of the hospital and therefore may bill for CCM services furnished to eligible patients, provided that it meets all applicable requirements. A hospital-owned practice that is not provider-based to a hospital is not part of the hospital and, therefore, not eligible to bill for services under the OPPS; but the physician (or other qualifying practitioner) practicing in the hospital-owned practice may bill under the PFS for CCM services furnished to eligible patients, provided all PFS billing requirements are met.
How long does a CPT 99490 bill take?
The service period for CPT 99490 is one calendar month, and CMS expects the billing practitioner to continue furnishing services during a given month as applicable after the 20 minute time threshold to bill the service is met (see #3 above). However practitioners may bill the PFS at the conclusion of the service period or after completion of at least 20 minutes of qualifying services for the service period. When the 20 minute threshold to bill is met, the practitioner may choose that date as the date of service, and need not hold the claim until the end of the month.
What is CPT 99490?
CPT 99490 describes activities that are not typically or ordinarily furnished face-to-face, such as telephone communication, review of medical records and test results, and consultation and exchange of health information with other providers. If these activities are occasionally provided by clinical staff face-to-face with the patient but would ordinarily be furnished non-face-to-face, the time may be counted towards the 20 minute minimum to bill CPT 99490. However, see #12 below regarding care coordination services furnished on the same day as an E/M visit.
What is Medicare outpatient?
Per section 20.2 of publication 100-04 of the Medicare Claims Processing Manual, a hospital outpatient is a person who has not been admitted by the hospital as an inpatient but is registered on the hospital records as an outpatient and receives services (rather than supplies alone) from the hospital. Since CPT code 99490 will ordinarily be performed non face-to-face (see # 11 above), the patient will typically not be a registered outpatient when receiving the service. In order to bill for the service, the hospital’s clinical staff must provide at least 20 minutes of CCM services under the direction of the billing physician or practitioner. Because the beneficiary has a direct relationship with the billing physician or practitioner directing the CCM service, we would expect a beneficiary to be informed that the hospital would be performing care management services under their physician or other practitioner’s direction.
How many times can you bill Medicare for E/M?
Under longstanding Medicare guidance, only one E/M service can be billed per day unless the conditions are met for use of modifier -25. Time cannot be counted twice, whether it is face-to-face or non-face-to-face time, and Medicare and CPT specify certain codes that cannot be billed for the same service period as CPT 99490 (see #13, 14 below). Face-to-face time that would otherwise be considered part of the E/M service that was furnished cannot be counted towards CPT 99490. Time spent by clinical staff providing non-face-to-face services within the scope of the CCM service can be counted towards CPT 99490. If both an E/M and the CCM code are billed on the same day, modifier -25 must be reported on the CCM claim.
What is CCM certified technology?
Hospital furnished the CCM services using a version of certified EHR that is acceptable under the EHR Incentive Programs as of December 31st of the calendar year preceding each Medicare PFS payment year (referred to as “CCM certified technology”). The hospital must also meet the requirements to use electronic technology in providing CCM services that are required for payment under the Physician Fee Schedule, such as 24/7 access to the care plan, and electronic sharing of the care plan and clinical summaries other than by fax.
When is CPT 99490 billed?
CPT 99490 can be billed if the beneficiary dies during the service period, as long as at least 20 minutes of qualifying services were furnished during that calendar month and all other billing requirements are met.
What is an FQHC visit?
FQHC visit that includes an Initial Preventive Physical Exam (IPPE) or Annual Wellness Visit (AWV) and includes the typical bundle of services that would be furnished per diem to a Medicare beneficiary receiving an IPPE or AWV , including all services that would otherwise be billed as a FQHC visit under G0466 or G0467.
What is an established patient?
An established patient is one who has received any professional medical or mental health services from any practitioner within the FQHC organization or from any sites within the FQHC organization within three years prior to the date of service.
What is a face to face encounter with a FQHC?
medically-necessary, face-to-face (one-on-one) encounter between a new patient and a qualified FQHC practitioner during which time one or more FQHC services are rendered and includes a typical bundle of services that would be furnished per diem to a Medicare beneficiary receiving medical services. A new patient is one who has not received any professional medical or mental health services from any practitioner within the FQHC organization or from any sites within the FQHC organization within the past three years prior to the date of service.
