How much does Medicare pay for inpatient rehab?
You must pay the inpatient hospital deductible for each benefit period. There's no limit to the number of benefit periods. Days 1-60: $1,556 deductible.*. Days 61-90: $389 coinsurance each day. Days 91 and beyond: $778 coinsurance per each “lifetime reserve day” after day 90 for each benefit period (up to a maximum of 60 reserve days over ...
What does Medicare Part a pay for hospital costs?
Dec 01, 2021 · The Inpatient Utilization and Payment Public Use File (Inpatient PUF) provides information on inpatient discharges for Medicare fee-for-service beneficiaries. To navigate directly to the Inpatient PUF, please use the links below. Inquiries regarding this data can be sent to [email protected].
What does Medicare Part a cover for inpatient care?
Apr 12, 2022 · The costs for rehab in an inpatient rehabilitation facility are as follows: You usually pay nothing for days 1–60 in one benefit period, after the Part A deductible is met. You pay a per-day charge set by Medicare for days 61–90 in a benefit period. You may use up to 60 lifetime reserve days at a per-day charge set by Medicare for days 91 ...
How much is the copay for Medicare Part D in 2019?
May 06, 2021 · You’ll usually need to pay a deductible ($1,484 per benefit period* in 2021). You pay coinsurance or copayment amounts in some cases, especially if you’re an inpatient for more than 60 days in one benefit period. Your copayment …

Is CPT 51798 covered by Medicare?
Your biller is correct at this time. When billing Medicare, you do not need a –25 modifier attached to the E/M when billing with 51798 (Measurement of post-voiding residual urine and/or bladder capacity by ultrasound, non-imaging).Dec 4, 2018
What does CPT code 51798 mean?
CPT code 51798 (Measurement of post-voiding residual urine and/or bladder capacity by ultrasound, non-imaging) should not be performed more than once per day.
How Much Does Medicare pay for 99072?
CPT code 99072 is defined as “additional supplies, materials, and clinical staff time over and above those usually included in an office visit or other non-facility service(s), when performed during a Public Health Emergency as defined by law, due to respiratory-transmitted infectious disease.” The AMA asked CMS to ...Dec 21, 2020
Is 51798 a surgical procedure?
The Current Procedural Terminology (CPT) code range for Surgical Procedures on the Bladder 51725-51798 is a medical code set maintained by the American Medical Association.
What is cpt76705?
CPT® 76705, Under Diagnostic Ultrasound Procedures of the Abdomen and Retroperitoneum. The Current Procedural Terminology (CPT®) code 76705 as maintained by American Medical Association, is a medical procedural code under the range - Diagnostic Ultrasound Procedures of the Abdomen and Retroperitoneum.
How are ultrasounds billed?
Ultrasounds can be classified as complete or limited as indicated in the CPT® code descriptor. To bill for a complete examination, all items and organs listed must be imaged and described, or reason an organ is not imaged or described (ie, organ surgically absent) documented.
Is CPT 99072 covered by Medicare?
During its quarterly update to the Medicare Physician Fee Schedule, CMS announced that it does not currently plan to pay for 99072. So, at the very least, CMS won't pay for this code through the end of 2020.Dec 1, 2020
How often can you bill 99072?
Code 99072 is to be reported only once per in-person patient encounter per provider identification number (PIN), regardless of the number of services rendered at that encounter.Sep 8, 2020
Does BCBS cover 99072?
For Blue Cross NC commercial members (fully insured, State Health Plan, Inter-Plan Program Host members), providers can include code 99072 on the claim; however, payment will be considered “incident to” the course of diagnosis or treatment of a condition (i.e. furnished as an integral, although incidental, part of the ...Sep 29, 2020
What is procedure code 52000?
The Current Procedural Terminology (CPT®) code 52000 as maintained by American Medical Association, is a medical procedural code under the range - Endoscopy-Cystoscopy, Urethroscopy, Cystourethroscopy Procedures on the Bladder.
Does 76000 need a modifier?
A. Yes, fluoroscopy has been bundled into ESWL. This means for Medicare claims, modifier -59 Distinct procedural service must be appended to code 76000 to receive reimbursement.
How do you bill a urinalysis?
CPT Code For Urinalysis Complete CPT Code 81003 is to bill for complete urine analysis. It would be done to detect a wide range of abnormalities like UTI, Kidney diseases, or other disorders of the urinary bladder.
What is the benefit period for Medicare?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
How long does it take to get into an inpatient rehab facility?
You’re admitted to an inpatient rehabilitation facility within 60 days of being discharged from a hospital.
What is part A in rehabilitation?
Inpatient rehabilitation care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What is Medicare Part A?
Published by: Medicare Made Clear. Medicare Part A covers medically necessary inpatient rehab (rehabilitation) care , which can help when you’re recovering from serious injuries, surgery or an illness. Inpatient rehab care may be provided in of the following facilities: A skilled nursing facility.
How much does Medicare pay for day 150?
You pay 100 percent of the cost for day 150 and beyond in a benefit period. Your inpatient rehab coverage and costs may be different with a Medicare Advantage plan, and some costs may be covered if you have a Medicare supplement plan. Check with your plan provider for details.
How long does Medicare cover inpatient rehab?
Medicare covers inpatient rehab in a skilled nursing facility – also known as an SNF – for up to 100 days. Rehab in an SNF may be needed after an injury or procedure, like a hip or knee replacement.
How long does it take to get Medicare to cover rehab?
The 3-day rule for Medicare requires that you are admitted to the hospital as an inpatient for at least 3 days for rehab in a skilled nursing facility to be covered. You must be officially admitted to the hospital by a doctor’s order to even be considered an inpatient, so watch out for this rule. In cases where the 3-day rule is not met, Medicare ...
What is an inpatient rehab facility?
An inpatient rehabilitation facility (inpatient “rehab” facility or IRF) Acute care rehabilitation center. Rehabilitation hospital. For inpatient rehab care to be covered, your doctor needs to affirm the following are true for your medical condition: 1. It requires intensive rehab.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is the medical condition that requires rehab?
To qualify for care in an inpatient rehabilitation facility, your doctor must state that your medical condition requires the following: Intensive rehabilitation. Continued medical supervision.
How much does Medicare Supplement pay for hospital visits?
(Under Medicare Supplement Plan N, you might have to pay a copayment up to $20 for some office visits, and up to $50 for emergency room visits if they don’t result in hospital admission.)
What does Medicare cover?
Medicare coverage: what costs does Original Medicare cover? Here’s a look at the health-care costs that Original Medicare (Part A and Part B) may cover. If you’re an inpatient in the hospital: Part A (hospital insurance) typically covers health-care costs such as your care and medical services. You’ll usually need to pay a deductible ($1,484 per ...
What type of insurance is used for Medicare Part A and B?
This type of insurance works alongside your Original Medicare coverage. Medicare Supplement insurance plans typically help pay for your Medicare Part A and Part B out-of-pocket costs, such as deductibles, coinsurance, and copayments.
How much is a deductible for 2021?
You’ll usually need to pay a deductible ($1,484 per benefit period* in 2021). You pay coinsurance or copayment amounts in some cases, especially if you’re an inpatient for more than 60 days in one benefit period. Your copayment for days 61-90 is $371 for each benefit period in 2021.
How much is coinsurance for 61-90?
Your copayment for days 61-90 is $371 for each benefit period in 2021. After you’ve spent more than 90 days in the hospital during a single benefit period, you’ll generally have to pay a coinsurance amount of $742 per day in 2021.
What does Part B cover?
Part B typically covers certain disease and cancer screenings for diseases. Part B may also help pay for certain medical equipment and supplies.
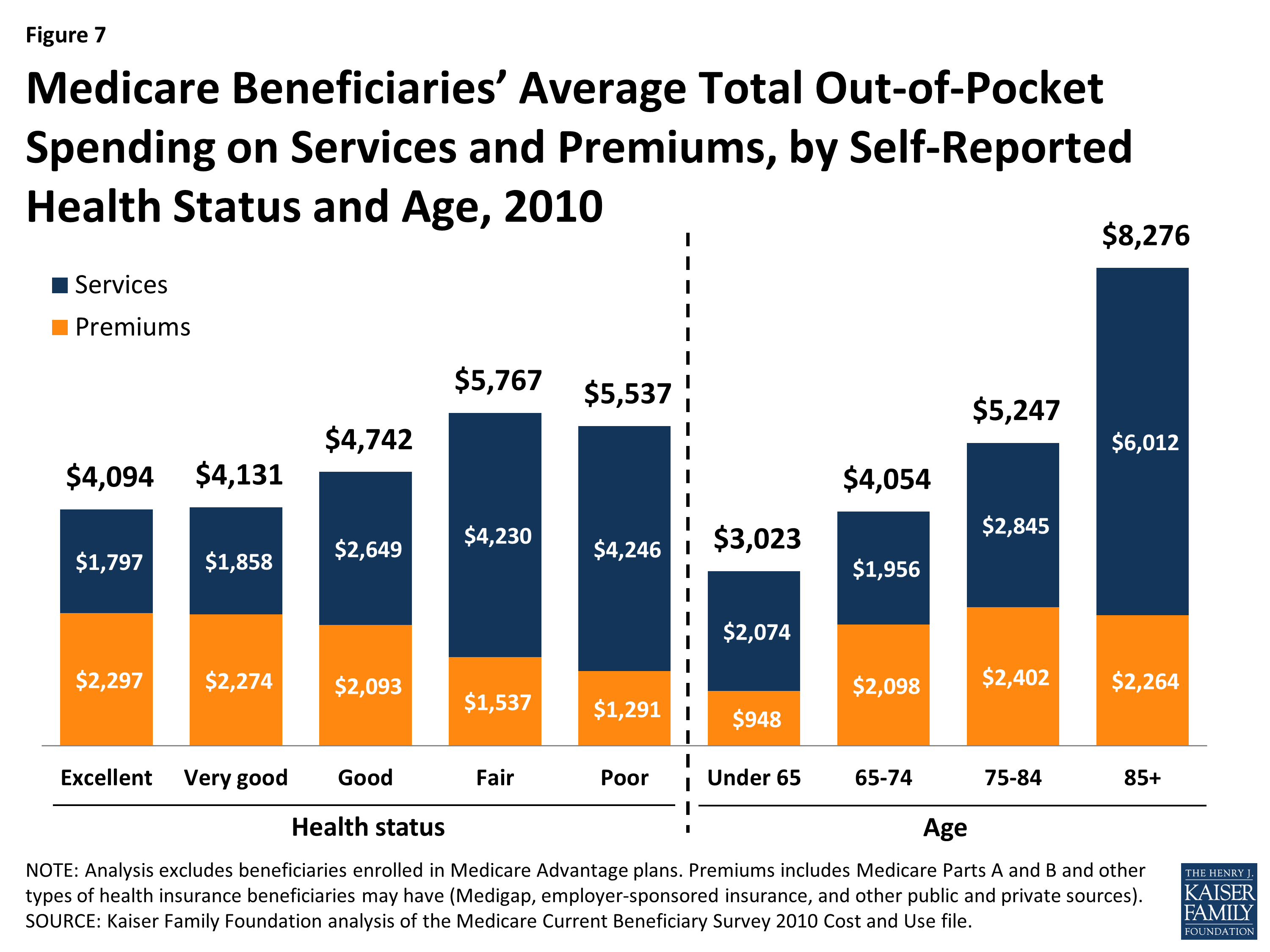
Does Medicare have a maximum spending limit?
Be aware that Original Medicare has no annual out-of-pocket maximum spending limit. If you meet your Medicare Part A and/or Part B deductibles, you still generally pay a coinsurance or copayment amount – and there’s no limit to what you might pay in a year.
What is Medicare Part A?
Medicare Part A, the first part of original Medicare, is hospital insurance. It typically covers inpatient surgeries, bloodwork and diagnostics, and hospital stays. If admitted into a hospital, Medicare Part A will help pay for:
How much does Medicare Part A cost in 2020?
In 2020, the Medicare Part A deductible is $1,408 per benefit period.
How long does Medicare Part A deductible last?
Unlike some deductibles, the Medicare Part A deductible applies to each benefit period. This means it applies to the length of time you’ve been admitted into the hospital through 60 consecutive days after you’ve been out of the hospital.
How many days can you use Medicare in one hospital visit?
Medicare provides an additional 60 days of coverage beyond the 90 days of covered inpatient care within a benefit period. These 60 days are known as lifetime reserve days. Lifetime reserve days can be used only once, but they don’t have to be used all in one hospital visit.
What is the Medicare deductible for 2020?
Even with insurance, you’ll still have to pay a portion of the hospital bill, along with premiums, deductibles, and other costs that are adjusted every year. In 2020, the Medicare Part A deductible is $1,408 per benefit period.
How much is coinsurance for 2020?
As of 2020, the daily coinsurance costs are $352. After 90 days, you’ve exhausted the Medicare benefits within the current benefit period. At that point, it’s up to you to pay for any other costs, unless you elect to use your lifetime reserve days. A more comprehensive breakdown of costs can be found below.
How long do you have to work to qualify for Medicare Part A?
To be eligible, you’ll need to have worked for 40 quarters, or 10 years, and paid Medicare taxes during that time.
Most Common Psychiatry CPT Codes
While there are many obscure and obtuse CPT Codes for Psychiatr y, it’s most efficient to learn the most commonly billed psychiatry CPT codes and their corresponding time allotments.
Medicare Reimbursement Rates for Psychiatrists
Medicare pays psychiatrists surprisingly well. Unfortunately, they now require electronic billing, which involves complex online enrollments for completion.
Medicaid Reimbursement Rates for Psychiatrists
Medicaid rates vary by state plan, carrier, and plan, so these rates below are a rough guide to compare against Medicare rates.
Commercial Insurance Reimbursement Rates for Psychiatrists
Commercial insurance rates vary dramatically across companies. Some rates are actually lower by 5% than Medicaid rates.
Maximize Your Reimbursement
While it’s useful to know about the reimbursement rates for psych services, what is more important is knowing how to successfully bill these various CPT codes to the appropriate payer, knowing your claims will be paid.