Are sleep studies covered by Medicare?
Sleep studies Medicare Part B (Medical Insurance) covers Type I, II, III, and IV sleep tests and devices if you have clinical signs and symptoms of sleep apnea. Your costs in Original Medicare You pay 20% of the Medicare-approved amount after you’ve met your Part B deductible . note:
Does Medicaid cover sleep studies?
Nov 27, 2018 · How much will Medicare pay for a sleep study? Medicare will pay 80% of the Medicare-approved amount for an in-home (HST) or in-center sleep study after you’ve met your Part B deductible (learn about this and other insurance terms here). If you have a secondary insurance, they may pick up the remaining 20% (read our post about how much sleep studies …
How to get paid to do a sleep study?
Jan 19, 2022 · Even if your sleep study is covered by Medicare, Medicare requires that you pay 20 percent of the Medicare-approved costs of the study. Additionally, you’ll have to pay any part of your Part B deductible that you haven’t yet met. In 2022, the Part B deductible is $233 per year. A Medicare Supplement Insurance (Medigap) plan can help pay for your sleep study Medicare …
Will Medicare cover sleep study?
Apr 02, 2019 · If you have Original Medicare, you will likely pay 20% of the Medicare-approved amount for your sleep study, and the Part B deductible will apply. If you are enrolled in a Medicare Advantage (MA) plan, you will have at least the same coverage as Original Medicare Part A and Part B, but many MA plans offer additional coverage.
How many sleep studies will Medicare pay for in a year?
All four levels of sleep studies (Type I, Type II, Type III and Type IV) are covered by Medicare. But a Type I study, which requires you to sleep overnight in a sleep lab facility under the supervision of a sleep specialist, must be specifically ordered by a doctor before Medicare will cover it.Jan 20, 2022
What diagnosis will cover sleep study?
Medicare covers sleep studies when the test is ordered by your doctor to diagnose certain conditions, including sleep apnea, narcolepsy and parasomnia. Sleep studies can take place at a sleep clinic or in your home. Medicare Part B covers 80 percent of the cost for sleep studies.
What is the cost of a sleep apnea study?
“Generally speaking, for self-pay rates, home sleep apnea tests will vary between $200 and $450,” Khan says. While both types of sleep apnea tests can provide valuable data, your candidacy for each type of test will depend on either your physician or the home sleep test provider you choose.
How often does Medicare require a sleep study for CPAP?
There is a three-month trial period for CPAP therapy. Medicare continues covering your CPAP machine after the first three months if your doctor confirms that CPAP therapy is helping.Sep 30, 2021
Are sleep studies worth it?
Sleep studies are a vital diagnostic tool for many sleep disorders, but they aren't necessary in all cases. A doctor can prescribe a sleep study depending on a person's symptoms and overall health.Mar 25, 2022
What is the average cost for a CPAP machine?
A CPAP machine's cost can range anywhere from $250 to $1,000 or more, with prices generally rising for the best cpap machines with more advanced features....How Much Does a CPAP Machine Cost?Machine TypeCost RangeAuto CPAP or APAP (Automatic Positive Airway Pressure)$450 to $1,8002 more rows•Mar 11, 2022
Is a sleep study covered by Medicare Australia?
The fee for a Home Sleep Study is $400. This is partially covered by Medicare (rebate of $293.90). In order to receive a rebate you must have a valid Medicare card and a current GP or specialist referral. Up to one (1) Home Based Sleep Study may be covered by Medicare per year, per person.
Does insurance cover sleep studies?
Yes, sleep studies are usually covered by health insurance. Most sleep disorder centers are just like a regular doctor's office and accept multiple insurance plans.Aug 4, 2017
How much is a CPAP without insurance?
There are many kinds of CPAP machines from different brands and manufacturers, so the prices range anywhere from $500 to $4000, with the average being around $850 without insurance.Jan 29, 2022
How much does a CPAP machine cost with Medicare?
Cost of a CPAP Machine with MedicareAverage cost of a CPAP machineMedicare coverageTotal cost to you$85080%$373Sep 15, 2021
How often can I get a new CPAP machine on Medicare?
every five yearsMedicare will usually cover the cost of a new CPAP machine every five years. If you had a machine before enrolling in Medicare, Medicare may cover some of the costs for a replacement CPAP machine rental and accessories if you meet certain requirements.
Are sleep apnea machines covered by Medicare Australia?
New South Wales In practice, only patients on a pension or health care card with severe OSA can access an ENABLE machine, and there is a wait of at least 4 months to access supply of a machine.
Does Medicare Cover In-Home Sleep Apnea Testing?
Yes.In 2008, the Centers for Medicare and Medicaid Services (CMS) updated the National Coverage Determination for CPAP to include home sleep apnea...
What Type of Home Sleep Apnea Test Does Medicare Cover?
Medicare will cover two types of home sleep testing devices: 1. Type III home sleep test. This is a four-channel device which measures (1) airflow,...
What Are The Criteria For Medicare to Cover An In-Home Or In-Center Sleep Study?
1. Patient must be referred by their attending physician (not a dentist). 2. Sleep must be recorded and staged. 3. Sleep study may be ordered to di...
Is Snoring Alone Sufficient For Ordering A Sleep Study For A Medicare Patient?
From a DME (CPAP) and Part B perspective for ultimate coverage of the PAP device for treatment of sleep apnea, Medicare must see elaboration and ex...
Does Medicare Cover Pap naps?
Currently, there is no coverage for PAP nap (afternoon nap or short daytime titration studies) sleep studies, regardless of billing codes or modifi...
How Often Will Medicare Cover A Sleep Study?
It depends on the circumstances requiring the new study. There is no lifetime limit for sleep studies. Generally, an initial diagnostic PSG and a f...
Who Can Interpret A Sleep Study For A Medicare Patient?
Once the sleep study is completed and the data is scored, the report is sent to a sleep specialist for review and interpretation. Only a sleep boar...
What Type of Certification Must The Sleep Technician Have to Perform Studies For Medicare Patients
The technician must be credentialed OR certified with one or more of the following: 1. American Academy of Sleep Medicine (AASM) 2. American Board...
How Much Will Medicare Pay For A Sleep Study?
Medicare will pay 80% of the Medicare-approved amount for an in-home (HST) or in-center sleep study after you’ve met your Part B deductible (learn...
What Codes Are Used to Bill Medicare For A Sleep Study?
For home sleep apnea testing, Medicare uses code G0399 (for a type III device) or G0398 (for a type II device). Medicare uses code 95810 for in-cen...
How Much Do Sleep Studies Cost With Medicare?
If you show symptoms of sleep apnea and your doctor orders testing, Medicare will help pay for Type I, II, III and IV sleep studies.
Does Medicare Cover Sleep Apnea?
Sleep apnea can be a serious health problem. It occurs when your normal breathing is interrupted during sleep. Medicare does help cover some sleep apnea tests and treatment.
Find Medicare Supplement Plans That Help Cover Your Sleep Study
If you undergo a sleep study that is covered by Medicare, a Medicare Supplement Insurance (Medigap) plan can help cover some of your associated Medicare costs.
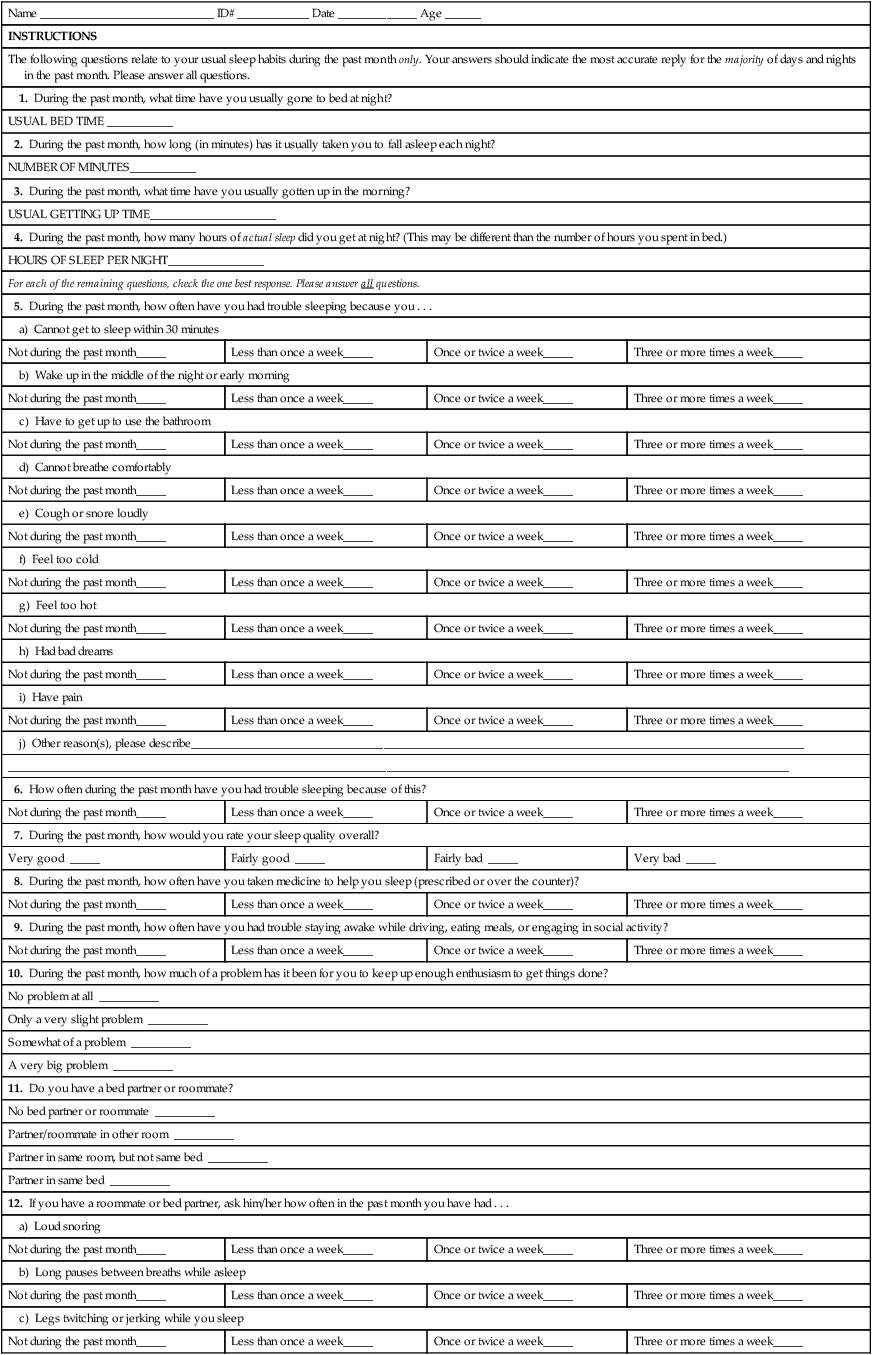
What is sleep study?
Sleep studies involve measuring and recording certain readings over the course of a night to evaluate sleep quality and quantity, and any other clinical signs that could lead to the diagnosis of a sleeping disorder. There are four main types of sleep studies available, and they are numbered one through four.
How many types of sleep studies are there?
There are four main types of sleep studies available, and they are numbered one through four. All of these tests have the potential to be covered by Medicare. Type I: Type I sleep tests are performed at a sleep lab facility and must be taken overnight. Type II: Type II tests utilize seven different channels to regulate body and brain function, ...
What is Medicare Part B?
Medicare Part B offers coverage for all four types of studies and the necessary treatments afterwards given a diagnosis. Medicare Part B is responsible for covering healthcare costs for medically necessary procedures, services, and supplies that are administered at a doctor’s office or in an outpatient setting.
Does Medicare pay for sleep study?
If you have Original Medicare, you will likely pay 20% of the Medicare-approved amount for your sleep study, and the Part B deductible will apply. If you are enrolled in a Medicare Advantage (MA) plan, you will have at least the same coverage as Original Medicare Part A and Part B, but many MA plans offer additional coverage.
Why is it important to sleep every night?
Getting enough sleep on a nightly basis is important for your body and brain to continue functioning correctly. The amount of sleep you need each night varies based on age and depends on individual needs, but the effects of lack of sleep are well documented.
Is sleep apnea a medical condition?
For instance, treating obstructive sleep apnea is considered medically necessary care. Sleep apnea is described as a condition that results in difficulty breathing while you sleep. It can result in snoring and gasping for air during the night.
Does Medicare cover CPAP?
If you are diagnosed with sleep apnea, treatment using a CPAP machine is also covered by Medicare insurance plans. CPAP stands for Continuous Positive Airway Pressure, and these devices work to maintain the pressure in your throat to prevent it from collapsing when you breathe in.
How long does a sleep test last?
The test may last several days depending on what sleep condition your doctor suspects.
What is the maintenance of wakefulness test?
Maintenance of wakefulness test (MWT). Also often performed the day after a PSG, this test helps doctors see if you have trouble staying awake during the day and if your sleepiness is a potential safety concern. Home sleep test (HST). This is typically a simple test you do at home yourself.
Does Medicare cover PSG?
Medicare covers the PSG test (Type I) test only if it is performed in a certified sleep lab facility. It may also cover certain types of home sleep study monitors (Type II, Type III, and Type IV) if you have clinical signs and symptoms of obstructive sleep apnea.
What is HST test?
Home sleep test (HST). This is typically a simple test you do at home yourself. During the test, you are connected to a portable monitor while you sleep in your bed at night. The monitor measures many of the same things as the PSG (such as heart rate or blood oxygen level) and is only appropriate in certain situations.
Does Medicare cover sleep studies?
Medicare coverage of sleep studies. Medicare Part B covers certain medically necessary sleep study tests if your doctor believes you have obstructive sleep apnea and you have clinical signs and symptoms for this condition; you pay 20% of Medicare-approved charges plus any applicable Part B deductible. Medicare covers the PSG test (Type I) ...
When Does Medicare Pay for a Sleep Study?
Sleep studies are covered by Medicare Part B health care coverage. And because Medicare Advantage insurance plans (Medicare Part C) are required by law to provide all of the same coverage as Part A and Part B, sleep studies are covered by these private Medicare plans as well.
How Much Does It Cost to Have a Sleep Apnea Test?
When your sleep test is covered by Medicare Part B, you will typically be responsible for a 20% coinsurance payment of the Medicare-approved amount after you meet your annual Part B deductible ($203 per year in 2021).
What Types of Sleep Studies Does Medicare Cover?
Type I sleep studies take place exclusively in a dedicated sleep lab facility and are observed in real-time by a Registered Polysomnographic Technologist (sleep specialist).
Is Sleep Apnea Covered by Medicare?
If you’ve been diagnosed with sleep apnea, Medicare Part B may provide coverage for a three-month trial of Continuous Positive Airway Pressure (CPAP) therapy. Coverage may be extended longer if your doctor determines the therapy is helping.
What is sleep study?
Basically, what a sleep study involves is having a doctor monitor you over the course of the night.
Why are sleep studies important?
Tests are needed to find out the source of a problem – this is why sleep studies are so important for those who find it very hard to get some rest during their sleep. If you have Medicare Part B, some costs may be covered, whereas a Medicare Supplement Insurance plan may also get you rid of the 20% coinsurance.
Does Medicare cover CPAP?
What’s even better is the fact that Medicare may cover a trial of three months for CPAP therapy , which aims to find out how you are responding to this type of treatment. However, even if certain sleep studies are covered, you may still have to pay some additional costs.
How does an EEG work?
It works by having an EEG analyze of your sleeping cycle. If there are any disruptions in your REM and nonREM cycles, the EEG will notice it and help set the diagnosis.
Does Medicare cover sleep study?
Medicare can indeed cover the costs of a sleep study, but it has specific requirements that you need to take into consideration. This is why talking to a healthcare provider is essential before you sign up for it. Basically, you need to find out if Medicare is accepted by your sleep study lab.
How long does Medicare pay for a CPAP machine?
Medicare pays the supplier to rent the CPAP machine for up to 13 months, and after that, the CPAP machine is considered yours.
How long is a CPAP trial?
If you have Medicare and you’re diagnosed with obstructive sleep apnea, you may be eligible to receive Continuous Positive Airway Pressure (CPAP) therapy for a three-month trial period. With Medicare Part B, you’ll pay 20% of the Medicare-approved amount for the CPAP machine rental and supplies, after reaching ...
What is the Medicare Part B deductible?
As mentioned, with Medicare Part B, you will be responsible for paying 20% of the Medicare-approved amount to rent a CPAP device and necessary parts or accessories, and the Part B deductible applies.
Does Medicare cover CPAP?
You must get the CPAP equipment from a Medicare-assigned supplier for Medicare to cover it. If your health-care provider decides that the sleep apnea therapy is helping, you may continue to be covered under Medicare for a longer period.
Can you stop breathing while sleeping?
Sleep apnea might be your diagnosis if you momentarily stop breathing while you sleep — sometimes many times per night, according to the U.S. Food and Drug Administration. Find affordable Medicare plans in your area. Find Plans. Find Medicare plans in your area. Find Plans.