How much does Medicare spend per capita by age?
Medicare per capita spending peaked at age 92 in 2000 ($9,557 in inflation-adjusted 2011 dollars), rising to age 96 by 2011 ($15,015 excluding Part D spending and $16,145 including Part D spending). Over time, the difference in Medicare per capita spending between beneficiaries ages 80 and older and younger beneficiaries has widened.
How much does Medicare spend on Medicare Advantage plans?
As a percent of total Medicare benefit spending, payments for Part A and Part B benefits covered by Medicare Advantage plans increased by nearly 50 percent between 2008 and 2018, from 21 percent ($99 billion) to 32 percent ($232 billion), as private plan enrollment grew steadily over these years (Figure 3).
How much does the elderly spend on health care?
In 2010, healthcare spending amounted to $18,424 per person for people aged 65 and older – about five times as much as per-person spending for children ($3,628) and triple what was spent on working-age individuals ($6,125). Much of the elderly’s medical costs are paid for by the government.
How much does Medicare supplement insurance cost for a 65-year-old?
A 65-year-old male will pay anywhere from $126 to $464 monthly for a Medigap policy, according to the American Association for Medicare Supplement Insurance. For 65-year-old women, the range is $118 to $464.
How much does Medicare cost for the average 65 year old?
At your current income level in 2021, you would pay around $4,342 in annual Medicare premiums ($3,564 for Part B and $778, on average, for Part D.) You would also likely buy a Medigap supplemental policy to help cover Medicare deductibles and limit annual cost sharing.
How much does Medicare cost per recipient?
In 2021, the average Medicare cost per beneficiary in the US was $15,671, an increase of 9% or $1,323 from 2020.
How much do most seniors pay for Medicare?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
How much do people pay out of pocket for Medicare?
In 2016, the average person with Medicare coverage spent $5,460 out of their own pocket for health care (Figure 1). This average includes spending by community residents and beneficiaries residing in long-term care facilities (5% of all beneficiaries in traditional Medicare).
How much does the government spend per person on Medicare?
Medicare spending per person has also grown, increasing from $5,800 to $15,300 between 2000 and 2021 – or 4.7% average annual growth over the 21-year period.
How much is the Medicare premium for 2021?
$148.50 forThe standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.
Does Medicare cost the same for everyone?
Everyone pays for Part B of Original Medicare. In 2020, the standard premium is $144.60/month for those making no more than $87,000 per year ($174,000 per year for married couples filing jointly). For 2020, the threshold for having to pay higher premiums based on income increased.
What is the average monthly cost for Medicare?
How much does Medicare cost?Medicare planTypical monthly costPart B (medical)$170.10Part C (bundle)$33Part D (prescriptions)$42Medicare Supplement$1631 more row•Mar 18, 2022
How much is taken out of your Social Security check for Medicare?
Medicare Part B (medical insurance) premiums are normally deducted from any Social Security or RRB benefits you receive. Your Part B premiums will be automatically deducted from your total benefit check in this case. You'll typically pay the standard Part B premium, which is $170.10 in 2022.
How much does the average American spend on healthcare out-of-pocket?
Overall, the average premium for a single American is about $7,188 for 2019, with employers carrying a significantly larger portion of the overall expense. Employer-based insurance for families costs about $20,576 this year, about a 5% increase from last year.
What are the negatives to a Medicare Advantage Plan?
The takeaway There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling. Whether you choose original Medicare or Medicare Advantage, it's important to review healthcare needs and Medicare options before choosing your coverage.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
The Medicare Cost
Medicare Part A is free if you have at least a 10-year work history. It covers hospital stays, skilled nursing, and some home healthcare services. It does, however, have a $1,364 deductible every benefit period, as well as some benefit restrictions.
Avoiding life-lasting penalties
Social Security benefits paid before age 65 will qualify you for Original Medicare (unless you live in Puerto Rico). You’ll be automatically registered about a month or two before you turn 65, and your card will arrive in the mail.
Medicare coverage gaps
Consider how you’ll pay for the things that Medicare doesn’t cover. It usually does not cover dental work or normal eye or hearing care, for example. Long-term care, cosmetic operations, and for the jet-setters, medical care abroad are all options.
Medicare Part A (Hospital Insurance)
Medicare Part A pays for inpatient clinic and hospital care as well as partial expert nursing and home-based healthcare services.
Medicare Part B (Medical Insurance)
Although Medicare Part A pays for inpatient services and some home-based healthcare services, you still need Part B coverage for protective care and medical appointments. Unfortunately, Medicare Part B doesn’t have a premium-free alternative like Part A.
Medicare Part D
Medicare Part D pays for treatment drugs, and its paid via premiums. Although Part D pays for your prescription drugs, you’re still liable for a portion of your medication expenses.
Medicare Part B
If you fail to register for Medicare Part B when you are eligible, you’ll have to pay a 10% fine for each year that you should have signed up.
Medicare Part D
Although signing up for Medicare Part D is optional, a penalty is charged for not signing up when you were supposed to.
Final Thought
To sum it all up, Medicare coverage is a bit complex, and there are many considerations unique to your condition.
Medicare Advantage Plan (Part C)
Monthly premiums vary based on which plan you join. The amount can change each year.
Medicare Supplement Insurance (Medigap)
Monthly premiums vary based on which policy you buy, where you live, and other factors. The amount can change each year.
How long does Medicare last?
Original, or basic, Medicare consists of Part A (hospital coverage) and Part B (outpatient and medicare equipment coverage). You get a seven-month window to sign up that starts three months before your 65th birthday month and ends three months after it.
How old do you have to be to sign up for Medicare?
While workers at businesses with fewer than 20 employees generally must sign up for Medicare at age 65 , people working for larger companies typically have a choice: They can stick with their group plan and delay signing up for Medicare without facing penalties down the road, or drop the company option and go with Medicare.
What to do if you are 65 and still working?
If you’ll hit age 65 soon and are still working, here’s what to do about Medicare 1 The share of people age 65 to 74 in the workforce is projected to reach 30.2% in 2026, up from 26.8% in 2016 and 17.5% in 1996. 2 If you work at a company with more than 20 employees, you generally have the choice of sticking with your group health insurance or dropping the company option to go with Medicare. 3 If you delay picking up Medicare, be aware of various deadlines you’ll face when you lose your coverage at work (i.e., you retire).
What happens if you delay picking up Medicare?
It’s becoming a common scenario: You’re creeping closer to your 65th birthday, which means you’ll be eligible for Medicare, yet you already have health insurance through work.
How many employees can you delay signing up for Medicare?
If you work at a large company. The general rule for workers at companies with at least 20 employees is that you can delay signing up for Medicare until you lose your group insurance (i.e., you retire). At that point, you’d be subject to various deadlines to sign up or else face late-enrollment penalties.
What is your 2018 income used for?
In other words, your 2018 income is used for your 2020 premiums. (There’s a form you can fill out to request a reduction in that income-related amount due to a life-changing event, such as retirement.) Roughly a third of Medicare enrollees choose to get their Parts A and B delivered through an Advantage Plan.
Can you continue taking a specialty drug under Medicare?
On the other hand, if you take a specialty drug that is covered by your group plan, it might be wise to continue with it if that drug would be more expensive under Medicare. Some 65-year-olds with younger spouses also might want to keep their group plan.
What percentage of Medicare is spending?
Key Facts. Medicare spending was 15 percent of total federal spending in 2018, and is projected to rise to 18 percent by 2029. Based on the latest projections in the 2019 Medicare Trustees report, the Medicare Hospital Insurance (Part A) trust fund is projected to be depleted in 2026, the same as the 2018 projection.
How much does Medicare cost?
In 2018, Medicare spending (net of income from premiums and other offsetting receipts) totaled $605 billion, accounting for 15 percent of the federal budget (Figure 1).
How is Medicare Part D funded?
Part D is financed by general revenues (71 percent), beneficiary premiums (17 percent), and state payments for beneficiaries dually eligible for Medicare and Medicaid (12 percent). Higher-income enrollees pay a larger share of the cost of Part D coverage, as they do for Part B.
How fast will Medicare spending grow?
On a per capita basis, Medicare spending is also projected to grow at a faster rate between 2018 and 2028 (5.1 percent) than between 2010 and 2018 (1.7 percent), and slightly faster than the average annual growth in per capita private health insurance spending over the next 10 years (4.6 percent).
Why is Medicare spending so high?
Over the longer term (that is, beyond the next 10 years), both CBO and OACT expect Medicare spending to rise more rapidly than GDP due to a number of factors, including the aging of the population and faster growth in health care costs than growth in the economy on a per capita basis.
What has changed in Medicare spending in the past 10 years?
Another notable change in Medicare spending in the past 10 years is the increase in payments to Medicare Advantage plans , which are private health plans that cover all Part A and Part B benefits, and typically also Part D benefits.
How is Medicare's solvency measured?
The solvency of Medicare in this context is measured by the level of assets in the Part A trust fund. In years when annual income to the trust fund exceeds benefits spending, the asset level increases, and when annual spending exceeds income, the asset level decreases.
Why is Medicare Advantage so popular?
Medicare Advantage — Medicare Advantage (MA) plans are popular because they tend to have much lower, or even zero premiums. In addition, many MA plans offer drug coverage. These plans may have deductibles, and charge co-pays for most services, leaving you at risk of more in out-of-pocket costs when you use services.
How much did Medicare cost in 2011?
Plans often charge a deductible and in 2011 you would need to spend a total of $4,550 out-of-pocket (not including premiums) before reaching catastrophic coverage. 6. Uncovered healthcare costs — In planning your budget, include costs that Medicare doesn’t cover — dental care, eye exams and eyeglasses, for example.
What is the biggest share of healthcare costs?
Spending on Medicare and health insurance premiums comprise the biggest share of healthcare costs, nearly two-thirds of overall senior healthcare spending. Premiums and coverage details can vary enormously, but here are a few things to consider: 1. Compare plans!
When do you have to enroll in Medicare Part B?
That period starts three months before you turn 65, includes the month you turn 65 and ends 3 months after the month you turn 65.
Why is the analysis focusing on Medicare beneficiaries over age 65 rather than younger adults who qualify for Medicare?
The analysis focuses on Medicare beneficiaries over age 65 rather than younger adults who qualify for Medicare because of a permanent disability to develop a better understanding of the relationship between Medicare spending and advancing age. This study examines patterns of Medicare spending among beneficiaries in traditional Medicare rather ...
How much did Medicare spend in 2011?
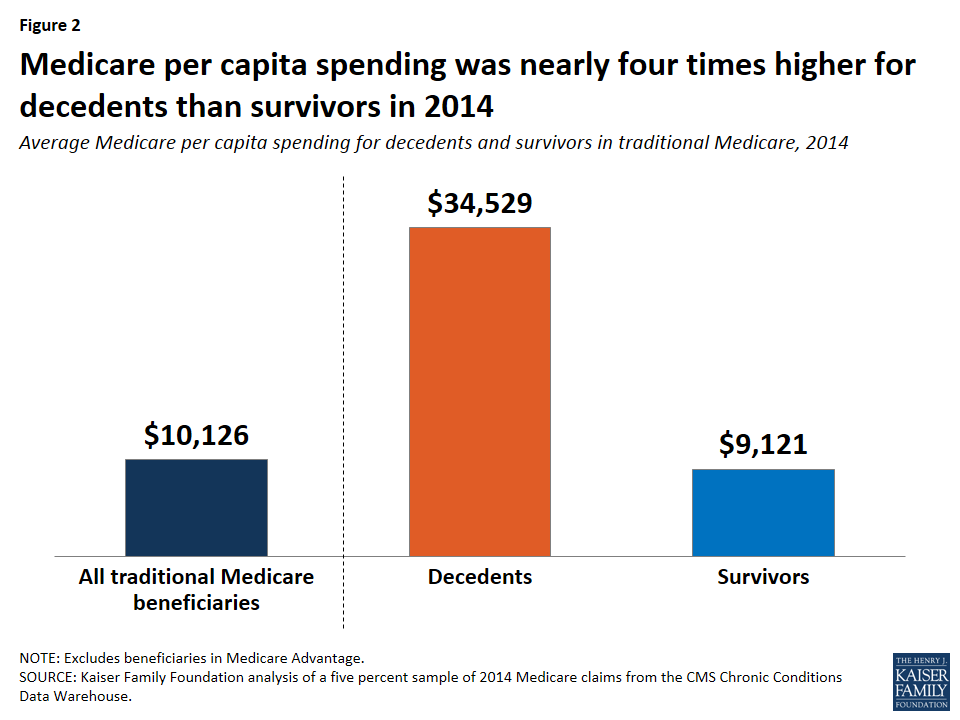
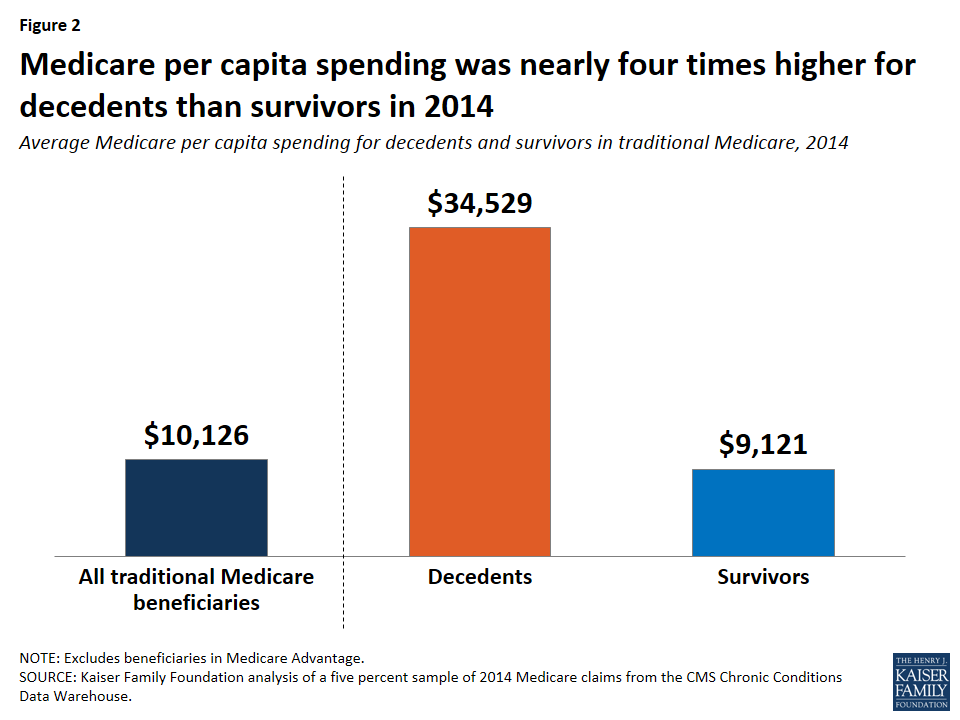
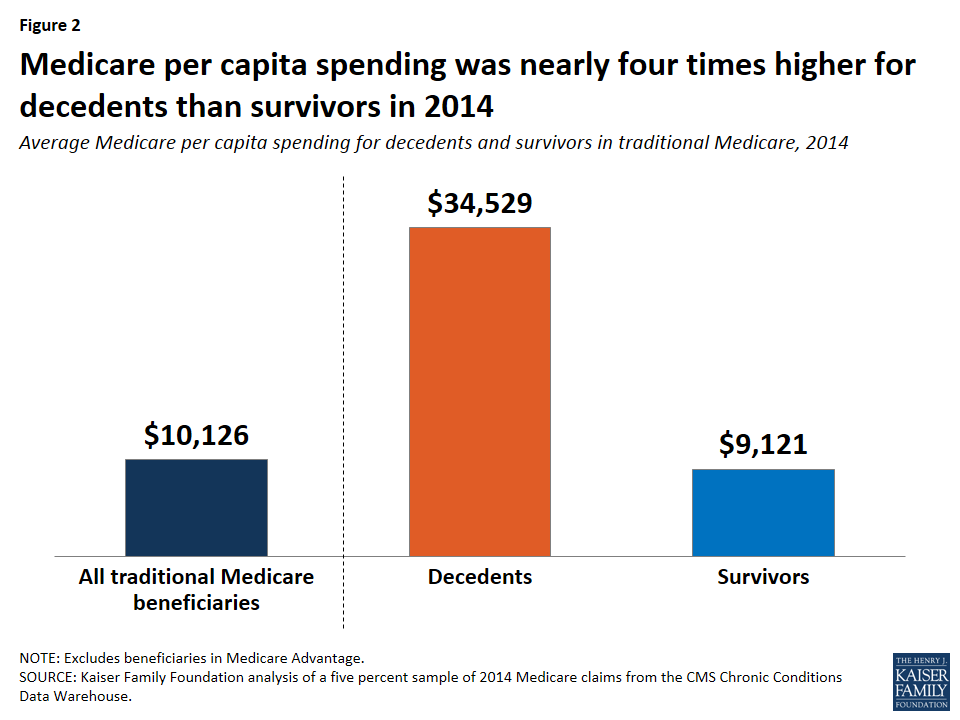
Average Medicare per capita spending in 2011 more than doubled between age 70 ($7,566) and age 96 ($16,145). The increase in Medicare per capita spending as beneficiaries age can be partially, but not completely, explained by the high cost of end-of-life care.
What percentage of Medicare beneficiaries were enrolled in 2011?
Because we lack comparable data for the 25 percent of beneficiaries enrolled in Medicare Advantage in 2011, it is not possible to assess whether patterns of service use and spending in traditional Medicare apply to the Medicare population overall. More information about the data, methods, and limitations can be found in the Methodology.
When did Medicare per capita increase?
Between 2000 and 2011, Medicare per capita spending grew faster for beneficiaries ages 90 and older than for younger beneficiaries over age 65, both including and excluding spending on the Part D prescription drug benefit beginning in 2006.
Is Medicare spending data available for all people?
The analysis excludes beneficiaries who are age 65 because some of these beneficiaries are enrolled for less than a full year; therefore, a full year of Medicare spending data is not available for all people at this year of age. The analysis focuses on Medicare beneficiaries over age 65 rather than younger adults who qualify for Medicare because ...
Will population aging affect health care?
According to the Congressional Budget Office, population aging is expected to account for a larger share of spending growth on the nation’s major health care programs through 2039 than either “excess spending growth” or subsidies for the coverage expansions provided under the Affordable Care Act. 2. To inform discussions about Medicare’s role in ...
Does Medicare increase as you age?
As the U.S. population ages, the increase in the number of people on Medicare and the aging of the Medicare population are expected to increase both total and per capita Medicare spending. The increase in per capita spending by age not only affects Medicare, but other payers as well.