Medicare Part B does cover diagnostic X-rays if your doctor or another health care provider determines they are medically necessary. After you meet your yearly Medicare Part B deductible ( $198 in 2020), you will typically pay 20 percent of the Medicare-approved amount for the X-ray.
Full Answer
Is Xtrac Therapy covered by insurance?
A: The XTRAC Therapy is covered by all major insurance companies and Medicare. If you are covered by insurance, typically your costs will be your standard co-pay or deductible costs. If you do not have insurance coverage, an XTRAC physician can discuss a cash payment plan.
Why choose Xtrac?
WHY CHOOSE XTRAC? Unlike conventional light therapies, the XTRAC excimer laser delivers a highly targeted therapeutic beam of UVB light to areas of the skin affected by psoriasis, vitiligo and atopic dermatitis without harming the surrounding skin so you can LIVE CLEAR. LIVE FREE.
How long does Xtrac therapy last?
A: Each patient is unique, but psoriasis sufferers who have experienced the XTRAC Therapy have found that relief can last for extended periods of time, typically 4 to 6 months or longer than other psoriasis treatments. Q: IS THE XTRAC THERAPY COVERED BY MY INSURANCE COMPANY?
Who is a candidate for the Xtrac therapy?
A: Almost all patients with plaque psoriasis are candidates for the XTRAC Therapy. If you have mild, moderate or severe psoriasis, you should consider the XTRAC Therapy. Q: ON WHICH AREAS OF THE BODY CAN THE XTRAC THERAPY BE USED? A: The XTRAC Therapy can be used on any plaque psoriasis regardless of location on the body.

Is xtrac covered by Medicare?
A: The XTRAC Therapy is covered by all major insurance companies and Medicare. If you are covered by insurance, typically your costs will be your standard co-pay or deductible costs.
Does Medicare pay for psoriasis treatment?
Does Medicare Cover Psoriasis Treatment? Yes, your Part B will cover biologics for psoriasis. This includes coverage for any medications and costs for treatments administered by infusion.
Is excimer laser covered by insurance?
Excimer laser therapy is considered cosmetic and not medically necessary for the treatment of alopecia areata in any setting. Services that are cosmetic are not covered under most benefit plans.
Is PUVA therapy covered by Medicare?
PUVA therapy is covered for treatment of intractable, disabling psoriasis, but only after the psoriasis has not responded to more conventional treatment. The Medicare Administrative Contractor should document this before paying for PUVA therapy.
Is treating psoriasis expensive?
“Typical treatments with biologics are quite costly, ranging anywhere from $10,000 to $25,000 per year. Other therapies for psoriasis are much less costly,” Dr.
How much are injections for psoriasis?
Biologic drugs are effective at treating psoriasis, but they come at a steep cost. According to a 2014 study , a year of treatment with adalimumab (Humira) can cost more than $39,000. Etanercept (Enbrel) can cost more than $46,000 per year, and ustekinumab (Stelara) can cost over $53,000 each year.
How do you bill an excimer laser?
In an example given for a patient who receives vitiligo Excimer laser treatment, the AMA states that CPT code 96900 is the correct code to report the service. It further states that CPT codes 96920-96922 are specifically indicated for psoriasis treatment.
Is vitiligo treatment covered by Medicare?
Narrow band phototherapy is fully covered in the United States by Medicare with no additional costs to the patient, plus a Medicare rebate applies to a percentage of the consultation cost. Most of private health insurance companies initially reject claims for reimbursement.
How effective is excimer laser treatment for vitiligo?
After 10 weeks of treatment repigmentation of more than 75% was found in 25% (7/28) of lesions of the high-responder location group versus 2% (1/43) of lesions of the low-responder location group. In most cases, laser-induced repigmentation was persistent, as determined 12 months after the end of treatment.
Does Medicare pay for infrared light therapy?
Transmittal Information. 10/2006 - The Centers for Medicare & Medicaid Services announced a National Coverage Determination stating the use of infrared and/or near-infrared light and/or heat, including monochromatic infrared energy, is non-covered.
Is home phototherapy covered by insurance?
Experience has shown that most health insurance companies will cover some or all of the cost of home phototherapy equipment; however, often this requires considerable persistence by the applicant.
Does insurance pay for light therapy?
Most major insurance companies now authorize or reimburse the purchase of light therapy equipment for Seasonal Affective Disorder (SAD).
What is XTRAC laser?
Unlike conventional light therapies, the XTRAC excimer laser delivers a highly targeted therapeutic beam of UVB light to areas of the skin affected by psoriasis, vitiligo and atopic dermatitis without harming the surrounding skin so you can LIVE CLEAR. LIVE FREE.
Is XTRAC FDA approved?
XTRAC has been cleared by the FDA and cited in over 45 clinical studies and research programs with findings published in peer-reviewed medical journals around the world. XTRAC is also endorsed by the National Psoriasis Foundation and the technology is part of the approved clinical protocols recommended by the American Academy of Dermatology.
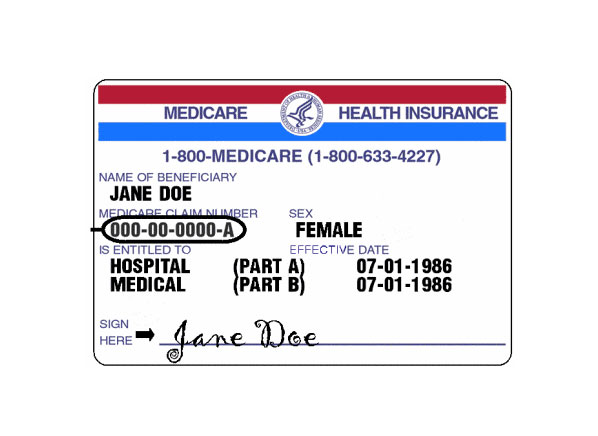
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What does Medicare Part B cover?
X-rays. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers. medically necessary. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
How much does Medicare pay for X-rays?
As mentioned above, if your X-ray is determined to be medically necessary, you will pay 20 percent of the Medicare-approved amount. Medically necessary. If your doctor or another health care provider determine that your X-rays are medically necessary, ...
What does it mean when a provider accepts a Medicare approved amount?
If the health care provider agrees to accept the Medicare-approved amount as full payment, this means that they accept Medicare assignment.
How often does Medicare cover bone mass?
Medicare Part B covers bone mass measurements. Part B will cover bone mass measurements once every 24 months ( or more often if necessary) if you have an increased risk of osteoporosis. If your X-rays show that you have possible osteoporosis, vertebral fractures or osteopenia, Medicare Part B will cover your bone mass measurements in full, ...
What is Medicare Part B excess charge?
If they choose not to accept the Medicare-approved amount as full payment, they may charge up to 15 percent more than the Medicare-approved amount . This is known as a Medicare Part B excess charge. Medicare Part B may help cover some additional services related to your bone health and other health conditions that result in an X-ray.
Does Medicare cover X-rays?
Medicare does not cover X-rays ordered by a chiropractor. Medicare Part B does not cover X-rays if they are ordered by a chiropractor. Your X-rays are only covered by Medicare when they are ordered by a medical doctor or other health care provider for diagnostic purposes.
Does Medicare cover chiropractic?
Medicare Part B does cover some chiropractic services. Specifically, Medicare will help cover manual manipulation of your spine if it is medically necessary in treatment of a subluxation (when a bone or bones in your spine are out of position).
How to get oxygen for Medicare?
For Medicare to cover oxygen equipment and supplies, beneficiaries must have the following: 1 Have a prescription from your doctor 2 Have documentation from your doctor showing you have a lung disorder preventing you from receiving enough oxygen and that other measures have not been successful in improving your condition 3 Proof of gas levels in your blood from your doctor
How long does DME have to supply oxygen?
Your rental payments will be paid up to 3 years. After that, the supplier will still own the equipment. However, they must still supply oxygen to you for an additional 24 months.
How much does canned oxygen cost?
Typically, canned oxygen with a concentration of around 95%, runs at about $50 per unit. Canned oxygen could be costly if you were to rely on the constant use of an oxygen machine. Costs could quickly escalate to more than $1,160 per day and more than $426,000 per year!
Does Medicare cover oxygen?
Medicare coverage for oxygen therapy is available when your doctor prescribes it to treat a lung or respiratory condition. Oxygen therapy can serve as a source of relief for those with severe asthma, COPD, emphysema, or other respiratory diseases. Medicare covers oxygen therapy in a hospital or at home when you meet specific criteria. Below we discuss the requirements necessary to qualify for oxygen supplies.
Does Medicare Supplement cover coinsurance?
Yes, supplement plans help cover the 20% coinsurance that Medicare doesn’t cover. It also covers other cost-sharing in the form of deductibles Choosing Medigap means you choose peace of mind. For those wanting to protect retirement savings, a Medicare Supplement plan will do just that.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. and. coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
How to find out how much a test is?
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like: 1 Other insurance you may have 2 How much your doctor charges 3 Whether your doctor accepts assignment 4 The type of facility 5 Where you get your test, item, or service
What is an outpatient copayment?
An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage.
How much is the maximum out of pocket for a coinsurance plan?
Many plans have 20 percent coinsurance costs until you reach the out-of-pocket maximum (the highest possible is $6,700 ). After you hit that amount, 100 percent coverage should kick in. Remember, these costs all depend on what kind of plan you have.
What is Medicare Supplemental Insurance?
Medigap (Medicare supplemental insurance) is a type of private insurance plan that helps cover your share of Medicare costs if you have parts A and B. Parts A and B together are known as original Medicare.
What is Medicare Part B?
Medicare Part B. Your Medicare Part B plan covers costs for cancer treatments and visits at outpatient medical centers like doctors’ offices and freestanding clinics. Services and treatments for cancer that may be covered under Part B include: cancer screening and prevention services. radiation therapy. medications to manage side effects ...
How much is Medicare Part A 2020?
The deductible amount for Medicare Part A is $1,408 per benefit period in 2020. A benefit period starts the day after you’re admitted to a hospital. It ends after you haven’t had any inpatient care for 60 days following that hospital stay. You may have more than one benefit period within a calendar year.
How much is coinsurance for 2020?
If you’re in the hospital for longer than 60 days, you’ll owe a coinsurance amount. The coinsurance amounts for 2020 are: $352 per day for hospital stays lasting 61 through 90 days. $704 per day for hospital stays that are 91 days and longer (for up to 60 extra lifetime reserve days)
Is Medigap more expensive than Part C?
A Medigap plan is generally a little more expensive than a Part C plan and doesn’t include prescription drugs. But it may be the most stress-free way to ensure that all cancer treatment costs are handled through your coverage.
Does Medicare cover radiation?
Medicare covers radiation treatments, but you’ll be responsible for any out-of-pocket costs after your plan has paid its share. Medigap plans can reduce or eliminate out-of-pocket costs for your treatments. Cancer treatments can get expensive quickly, especially when you need regular chemotherapy or radiation therapy.
Why is Physical Therapy Valuable?
According to the American Physical Therapy Association (APTA), physical therapy can help you regain or maintain your ability to move and function after injury or illness. Physical therapy can also help you manage your pain or overcome a disability.
Does Medicare Cover Physical Therapy?
Medicare covers physical therapy as a skilled service. Whether you receive physical therapy (PT) at home, in a facility or hospital, or a therapist’s office, the following conditions must be met:
What Parts of Medicare Cover Physical Therapy?
Part A (hospital insurance) covers physical therapy as an inpatient service in a hospital or skilled nursing facility (SNF) if it’s a Medicare-covered stay, or as part of your home health care benefit.
Does Medicare Cover In-home Physical Therapy?
Medicare Part A covers in-home physical therapy as a home health benefit under the following conditions:
What Are the Medicare Caps for Physical Therapy Coverage?
Medicare no longer caps medically necessary physical therapy coverage. For outpatient therapy in 2021, if you exceed $2,150 with physical therapy and speech-language pathology services combined, your therapy provider must add a modifier to their billing to show Medicare that you continue to need and benefit from therapy.
How does extracapsular surgery work?
The surgeries include: Extracapsular – This surgery works to remove the cloudy lens in one piece. Once the surgeon removes the lens, they’ll insert an intraocular lens to replace the lens they removed. Phacoemulsification – Your surgeon will use an ultrasound to break up the clouds lens before they remove it.
Do you have to pay for cataract surgery if you don't have Medicare?
Still, you will have a small percentage leftover that you’ll have to pay if you don’t have a supplementary insurance plan or are enrolled in a Medicare Advantage plan that offers additional coverage. Most people have cataract surgery in either an Ambulatory Surgical Center or Hospital Outpatient Department.
Does Medicare cover cataract surgery?
Medicare Insurance and Aftercare. Additionally, Medicare may cover some expenses as long as they’re a result of your cataract surgery. Most of the time, Medicare won’t pay for contact lenses or glasses. However, this changes if your cataract surgery involves implanting an IOL.