The lowest cost option is Mavyret at $26,400 for 8-weeks and $39,600 for 12-weeks. In a population such as Medicare eligible adults in the US, which is suspected to contain the majority of HCV infections, we should expect to see all of these treatments made available.
How much does Mavyret cost?
Sep 10, 2021 · For patients on Medicare Part D, the cost can range from $660.00 – 2,847.00 per month, based on your coverage phase. Patients with Low-Income Subsidy for Medicare will pay $8.95 per month. Compared to other approved oral HCV treatments, Mavyret tablets are priced very competitively and may be your lowest-cost option.
Is Mavyret covered by Medicare?
$660.00 – 2,847.00 per month, depending on coverage phase Monthly out-of-pocket cost for MAVYRET may vary depending on patient's other medication costs. Most Medicare patients have Standard Part D prescription coverage, which has different …
How can I lower my copay for Mavyret?
Copay Range$38 – $15180. After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. Copay Range. $68 – $15180.
What is the difference between Mavyret available and preferred formulary status?
May 31, 2020 · Whether or not you have commercial insurance, Medicaid, Medicare—or even if you don't have insurance—MAVYRET Patient Support is ready and waiting to help. Call 1-877-628-9738 to learn more. Beside above, how much does Mavyret cost? Abbvie has priced Mavyret at $13,200 per month, or $26,400 per treatment course, before discounts. Although this is still …
Does Medicare pay for Mavyret?
Yes. 78% of Medicare prescription drug plans cover this drug.
How much does maverick for hep C cost?
Abbvie has priced Mavyret at $13,200 per month, or $26,400 per treatment course, before discounts. Although this is still expensive, Macyret is priced significantly lower than other hepatitis C treatments.Aug 23, 2017
Does Medicaid pay for Mavyret?
MAVYRET has preferred formulary status on the majority of2: Patients on Medicaid can have out-of-pocket costs of $20 or less depending on state plan. Most patients with commercial insurance will pay as little as $5 per month with their MAVYRET copay card.
How much does Mavyret cost without insurance?
How much does Mavyret cost without insurance? Without insurance, the customers pay an average of $3,168.19 for a refill of Mavyret. However, when you claim your SingleCare savings, you pay a discounted retail price of $2,634.56 for this prescription drug at your neighborhood pharmacy.
What is the generic for MAVYRET?
No. There is currently no therapeutically equivalent version of Mavyret available in the United States. Note: Fraudulent online pharmacies may attempt to sell an illegal generic version of Mavyret. These medications may be counterfeit and potentially unsafe.
Is MAVYRET or Epclusa better?
If you have liver disease, Epclusa may be a better treatment choice for you. Severe scarring of your liver. Mavyret isn't used for treating hepatitis C if you have severe cirrhosis. However, Epclusa can be used with the drug ribavirin for this purpose.Feb 19, 2021
What is the success rate of Mavyret?
Yes, Mavyret is a treatment that can clinically cure hepatitis C viral infection (HCV). The success rate for curing hepatitis C with Mavyret ranges from 95 to 99%.Jul 22, 2020
How do you get Mavyret without insurance?
You may be eligible to receive free MAVYRET if you:Have been prescribed MAVYRET.Have limited or no health insurance coverage.Live in the United States.Are being treated by a licensed U.S. health care provider on an outpatient basis.
What are the side effects of Mavyret?
Common side effects of Mavyret include nausea, headache, fatigue (lack of energy), and diarrhea. These side effects could make you feel unwell. While taking Mavyret, talk with your doctor if you feel sick or have side effects that become severe or don't go away.Jan 22, 2021
When is the best time to take MAVYRET?
For Hepatitis C: “I started the Mavyret, 7 days ago. I feel GREAT, I have found out that to keep the nausea away, it is best taken at night with food a few hours before bed. Drink plenty of liquids and eat your meals , do not skip eating.
What drugs affect MAVYRET?
Coadministration of MAVYRET with drugs that induce P-gp/CYP3A may decrease glecaprevir and pibrentasvir plasma concentrations. Carbamazepine, phenytoin, efavirenz, and St. John's wort may significantly decrease plasma concentrations of glecaprevir and pibrentasvir, leading to reduced therapeutic effect of MAVYRET.
Can you drink alcohol while taking MAVYRET?
Mavyret doesn't have any known interactions with alcohol. However, you shouldn't drink alcohol if you have hepatitis C virus (HCV). Alcohol makes HCV worse, which can lead to severe scarring (cirrhosis) in your liver. If you drink alcohol, and you're concerned about how to stop drinking, talk with your doctor.Aug 18, 2019
What tier is Mavyret?
Tier 5. Medicare prescription drug plans typically list Mavyret on Tier 5 of their formulary. Generally, the higher the tier, the more you have to pay for the medication. Most plans have 5 tiers.
How much does Medicare cover in the donut hole?
Therefore, you may pay more for your drug. Copay Range. $7 – $15180. In the Post-Donut Hole (also called Catastrophic Coverage) stage, Medicare should cover most of the cost of your drug.
What is prior authorization for Medicare?
Most Medicare prescription drug plans have prior authorization rules that will require your prescriber to contact your plan before you can get your medication. This is to show that the drug is medically necessary.
What is the post deductible stage?
After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug.
Manufacturer Coupon Visit Manufacturer Site
Many manufacturers offer programs that will reduce your out-of-pocket costs for this prescription. These programs are free but may have some rules or restrictions, so you’ll want to review carefully. When you’re ready to use this coupon, simply present the coupon to your pharmacist with a valid prescription for your medication.
FDA Approves Mavyret for Hepatitis C
GoodRx‘s cash prices are based on multiple sources, including published price lists, purchases, claims records, and data provided by pharmacies. Most of our discount and coupon prices are based on contracts between a pharmacy (or pharmacy purchasing group) and a Pharmacy Benefit Manager (PBM), who provides prices to us.
What is a mavyret?
MAVYRET is indicated for the treatment of adult and pediatric patients 12 years and older or weighing at least 45 kg with chronic hepatitis C virus (HCV) genotype 1, 2, 3, 4, 5, or 6 infection without cirrhosis or with compensated cirrhosis (Child-Pugh A). MAVYRET is indicated for the treatment of adult and pediatric patients 12 years and older or weighing at least 45 kg with HCV genotype 1 infection, who previously have been treated with a regimen containing an HCV NS5A inhibitor or an NS3/4A protease inhibitor (PI), but not both.
What is the hepatitis C genotype for mavyret?
MAVYRET is indicated for the treatment of adult and pediatric patients 12 years and older or weighing at least 45 kg with chronic hepatitis C virus (HCV) genotype 1, 2, 3, 4, 5, or 6 infection without cirrhosis or with.
What tests are performed for cirrhosis?
In patients with compensated cirrhosis or evidence of advanced liver disease, perform hepatic laboratory testing as clinically indicated; and monitor for signs and symptoms of hepatic decompensation such as the presence of jaundice, ascites, hepatic encephalopathy, and variceal hemorrhage.
What is preferred plan?
Preferred means the product is placed on the plan’s preferred formulary. Non-preferred products require a higher out-of-pocket cost or step edit, or are placed on a higher tier. *Terms and Conditions apply.
Can you get reimbursement for a mavyret card?
Patients may not seek reimbursement for value received from MA VYRET Patient Support including the copay card from any third-party payers. Offer subject to change or discontinuance without notice. Restrictions, including monthly maximums, may apply. This is not health insurance.
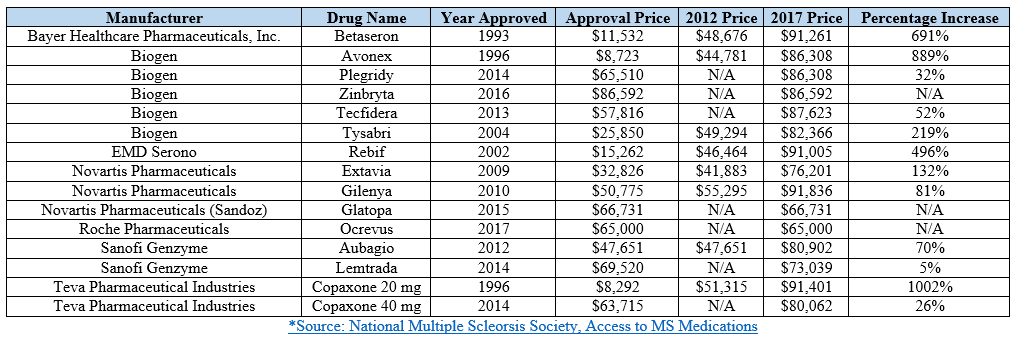
How much does a drug cost in 2019?
Expected annual out-of-pocket costs in 2019 average $8,109 across the 28 specialty tier drugs covered by some or all plans in this analysis. For 28 of the 30 studied specialty drugs used to treat four health conditions—cancer, hepatitis C, multiple sclerosis (MS), and rheumatoid arthritis (RA)—expected annual out-of-pocket costs for a single drug in 2019 range from $2,622 for Zepatier, a treatment for hepatitis C, to $16,551 for Idhifa, a leukemia drug. Two of the 30 drugs are not covered by any plan in our analysis. (See Tables 1 and 2 for drug-specific cost and coverage information.)
How much does a zepatier cost?
For 28 of the 30 studied specialty drugs used to treat four health conditions—cancer, hepatitis C, multiple sclerosis (MS), and rheumatoid arthritis (RA)—expected annual out-of-pocket costs for a single drug in 2019 range from $2,622 for Zepatier, a treatment for hepatitis C, to $16,551 for Idhifa, a leukemia drug.
Does Medicare cover Gleevec?
One of the 15 cancer drugs, Gleevec, is not covered by any plan in our analysis in 2019, but the generic equivalent, imatinib mesylate, is covered by all plans, which is sufficient to meet the formulary coverage requirement that plans cover all or substantially all drugs in six so-called “protected” classes, including cancer drugs.
Does Medicare Part D cover out of pocket costs?
Discussion. This analysis shows that Medicare Part D enrollees who do not receive low-income subsidies can expect to pay thousands of dollars in out-of-pocket costs for a single specialty tier drug in 2019, even though the Part D coverage gap for brands is now fully closed. Although Part D offers catastrophic coverage for high drug costs, ...
Does Part D cover cancer?
Although Part D offers catastrophic coverage for high drug costs, beneficiaries can still face substantial out-of-pocket costs for expensive medications, including many drugs for cancer, hepatitis C, multiple sclerosis, and rheumatoid arthritis, because there is no hard cap on spending in the Part D benefit.
Does Medicare cover specialty drugs?
Figure 5: Medicare Part D plans vary in whether they cover specialty tier drugs that are not in a protected class. Some plans cover a larger number of specialty drugs to treat each condition than other plans (outside of the protected-class cancer drugs).
Is glatiramer acetate higher than copaxone?
Expected annual out-of-pocket costs for glatiramer acetate are actually higher than costs for the brand Copaxone in 2019 —and higher than out-of-pocket costs for the other branded MS drugs—while the share of out-of-pocket costs above the catastrophic threshold is lower.