| How Much You'll Pay for Medicare Part B in 2016 | ||
|---|---|---|
| Single Filer Income | Joint Filer Income | 2016 Monthly Premium |
| Up to $85,000 | Up to $170,000 | $121.80 or $104.90* |
| $85,001 - $107,000 | $170,001 - $214,000 | $170.50 |
| $107,001 - $160,000 | $214,001 - $320,000 | $243.60 |
How much does Medicare cost at age 65?
Nov 10, 2015 · The Medicare Part A annual deductible that beneficiaries pay when admitted to the hospital will be $1,288.00 in 2016, a small increase from $1,260.00 in 2015. The Part A deductible covers beneficiaries' share of costs for the first 60 days of Medicare-covered inpatient hospital care in a benefit period.
How much does Medicare cost per month?
Aug 25, 2016 · If you were enrolled in Medicare Part B prior to 2016, your 2016 monthly premium is generally $104.90. Your 2016 monthly premium is typically $121.80 if any of the following is true for you: You enrolled in Medicare Part B in 2016 for the first time. You don’t receive Social Security benefits. You get a bill for the Part B premium.
What is the monthly premium for Medicare Part B?
Dec 16, 2020 · The Medicare Part B premium will remain the same at $104.90 per month for most individuals. The Social Security Administration recently announced that there will be no cost of living increase for 2016. Due to this, most Part B beneficiaries will be “held harmless” from premium increases in 2016, according to the CMS release.
Who is eligible for Medicare Part B reimbursement?
Jun 07, 2015 · Here are some important highlights for this first chart, showing payment increases and other differences between 2015 and 2016: Initial deductible – For 2016, this will increase by $40 to $360 Initial coverage limit – In 2015, this was $2,960; in 2016, it increases to $3,310

What was the monthly cost of Medicare in 2016?
What was the monthly cost of Medicare in 2017?
What was the cost of Medicare in 2018?
What was the Medicare Part D premium for 2017?
What are Medicare premiums for 2020?
How much are Medicare premiums for 2019?
What is the Medicare deductible for 2021?
How Medicare premiums are calculated?
What are the Medicare income limits for 2022?
| If your yearly income in 2020 (for what you pay in 2022) was | You pay each month (in 2022) | |
|---|---|---|
| File individual tax return | File joint tax return | |
| $91,000 or less | $182,000 or less | $170.10 |
| above $91,000 up to $114,000 | above $182,000 up to $228,000 | $238.10 |
| above $114,000 up to $142,000 | above $228,000 up to $284,000 | $340.20 |
What was Medicare Part B premium in 2015?
What is the Medicare Part B deductible 2018?
What are the Irmaa brackets for 2019?
| IRMAA Table | 2019 |
|---|---|
| More than $267,000 but less than or equal to $320,000 | $352.20 |
| More than $320,000 but less than $750,000 More than $750,000 | $433.40 $460.50 |
| Married filing separately | |
| More than $85,000 but less than $415,000 More than $415,000 | $433.40 $460.50 |
How much did Medicare pay in 2016?
In 2016, you pay: $0 for the first 20 days of each benefit period. $161 per day for days 21-100 of each benefit period. All costs for each day after day 100 of the benefit period. If you don’t qualify for premium-free Medicare Part A, you can enroll in Part A for $226 per month if you’ve worked and paid Social Security taxes for 30 to 39 quarters, ...
Do you have to pay for Medicare Part A?
Most people don’t have to pay a premium for Medicare Part A. They do, however, have to factor in the following Medicare Part A costs for inpatient hospital stays for each benefit period. Medicare considers a benefit period to start the day that a hospital or skilled nursing facility (SNF) admits you as an inpatient.
How long is a benefit period for Medicare?
Medicare considers a benefit period to start the day that a hospital or skilled nursing facility (SNF) admits you as an inpatient. The end of the benefit period occurs when you haven’t received any inpatient hospital care (or skilled care in an SNF) for 60 consecutive days. Deductible: $1,288.
What is Medicare Supplement Plan?
Costs for Medicare Supplement (Medigap) Those who need help paying for such health-care costs as deductibles, premiums, and other Original Medicare expenses may want to purchase a Medicare Supplement plan, also known as Medigap plan.
How to contact Medicare directly?
To learn about Medicare plans you may be eligible for, you can: Contact the Medicare plan directly. Call 1-800 -MEDICARE (1-800-633-4227) , TTY users 1-877-486-2048; 24 hours a day, 7 days a week.
Is Medicare dual eligible?
You quality for both Medicare and Medicaid benefits, and Medicaid pays for your premiums. This is called being “dual-eligible.”. Your income exceeds a certain dollar amount. Your premium could be higher than the amount listed above, as there are different premiums for different income levels.
Will Medicare increase in 2016?
Medicare beneficiar ies will face higher Medicare costs in 2016. Several costs, including the Part A deductible, the Part A inpatient hospital stay co-insurance, and the Part B deductible will increase in 2016, according to a Centers for Medicare & Medicaid Services (CMS) news release .
How much is Medicare Part B?
The Medicare Part B premium will remain the same at $104.90 per month for most individuals. The Social Security Administration recently announced that there will be no cost of living increase for 2016.
See Also -- CALCULATOR: How Much You'll Pay for Medicare in 2016
Medicare beneficiaries who have Part B premiums withheld from their Social Security checks--about 70% of beneficiaries--will continue to pay $104.90 per month for Part B. If you aren't collecting Social Security yet or will enroll in Medicare in 2016, you will have to pay $121.80 per month in 2016.
See Also: 10 Things You Must Know About Medicare
Your income is usually based on your last tax return on file, which would be your 2014 return, for 2016 premiums. But you may be able to get the high-income surcharge reduced or eliminated if your income has decreased since then because of certain life-changing events, such as the death of a spouse, divorce, retirement or reduced work hours.
Medicare costs increased in 2016 and are set to rise further in 2017
Matt is a Certified Financial Planner based in South Carolina who has been writing for The Motley Fool since 2012. Matt specializes in writing about bank stocks, REITs, and personal finance, but he loves any investment at the right price. Follow him on Twitter to keep up with his latest work! Follow @TMFMathGuy
Medicare got more expensive in 2016
Medicare got more expensive in 2016, in terms of both premiums and deductibles, although some of the changes didn't affect all beneficiaries.
What cost increases are taking effect in 2017?
Since Social Security beneficiaries received a COLA for 2017, albeit a small one, Medicare Part B premiums are increasing for everyone. The 70% of beneficiaries who pay their premiums from Social Security will see an increase to $109, about $4 more than the current level. The other 30% can expect a 10% increase in their Part B premiums to $134.
What could change under the Trump administration?
The changes that could be made to Medicare during 2017 (if any) depend on who gets their way -- President-elect Donald Trump or the Republican-controlled Congress. It's no secret that Medicare isn't in the best financial shape, and both parties have different ideas of how the problem should be fixed.
How much money did Medicare spend in 2016?
In FY 2016, the Office of the Actuary has estimated that gross current law spending on Medicare benefits will total $672.6 billion. Medicare will provide health insurance to 57 million individuals who are 65 or older, disabled, or have end-stage renal disease.
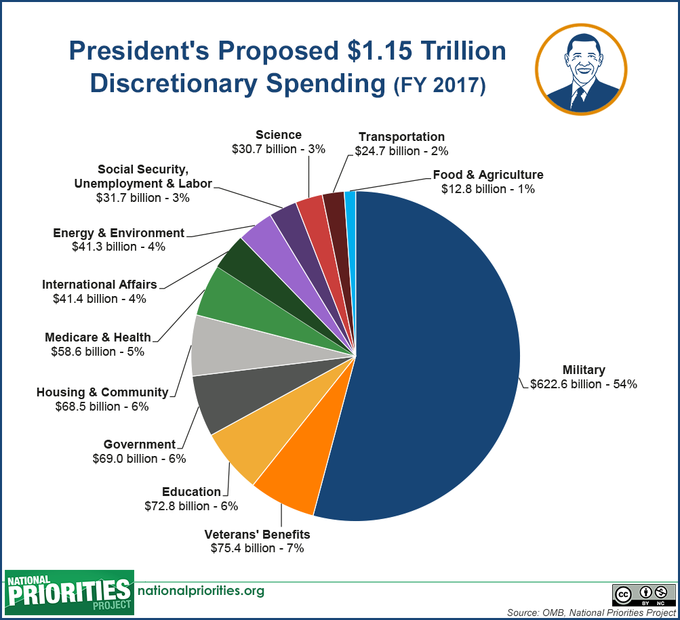
What is the Medicare budget for 2016?
The FY 2016 Budget includes a package of Medicare legislative proposals that will save a net $423.1 billion over 10 years. The proposals are scored off the President’s Budget adjusted baseline, which assumes a zero percent update to Medicare physician payments. These reforms will strengthen Medicare by more closely aligning payments with the costs of providing care, encouraging health care providers to deliver better care and better outcomes for their patients, and improving access to care for beneficiaries. The Budget includes investments to reform Medicare physician payments and accelerate physician participation in high-quality and efficient healthcare delivery systems. Finally, it makes structural changes in program financing that will reduce Federal subsidies to high income beneficiaries and create incentives for beneficiaries to seek high value services. Together, these measures will extend the Hospital Insurance Trust Fund solvency by approximately five years.
What is Medicare Part C?
Part C ($198.0 billion gross spending in 2016): Medicare Part C, the Medicare Advantage program, pays plans a capitated monthly payment to provide all Part A and B services, and Part D services, if offered by the plan.
Does the hold harmless provision apply to Medicare Part B?
Clarify Calculation of the Late Enrollment Penalty for Medicare Part B Premiums: This proposal would clarify that the cap on increases to the Part B premium, commonly referred to as the hold harmless provision, does not apply to the calculation of the Part B late enrollment penalty, but applies only to the annual increase to the basic Part B premium. The hold harmless provision imposes a cap on increases to the basic Part B premium based on the amount of the cost-of-living adjustment increase in a beneficiary’s Social Security benefits. This clarification is consistent with current CMS practice. [No budget impact]
What are the goals of CMS for FY 2016?
Clinical Quality Improvement: The key goals for FY 2016 are improving the health status of communities; delivering patient-centered, reliable, accessible, and safe care; and better care at lower costs. Through improving cardiac health, reducing disparities in diabetic care, using immunization information systems and meaningful use of health IT to improve prevention coordination, CMS aims to improve the health status ofbeneficiaries. These goals will also be achieved by efforts to reduce healthcare‑associated infections, healthcare‑associated conditions in nursing homes, and hospital readmissions and adverse drug events.
What is the 190 day limit for psychiatric services?
Eliminate the 190-day Lifetime Limit on Inpatient Psychiatric Facility Services: The 190-day lifetime limit on inpatient services delivered in specialized psychiatric hospitals is one of the last obstacles to behavioral health parity in the Medicare benefit. Beginning in FY 2016, this proposal would eliminate the 190-day limit and more closely align the Medicare mental health care benefit with the current inpatient physical health care benefit. Many beneficiaries who utilize psychiatric services are eligible for Medicare due to a disability, which means they are often younger beneficiaries who can easily reach the 190-day limit over their lifetimes. Therefore, this proposal would expand the psychiatric benefit and bring parity to the sites of service, while also containing the additional costs of removing the 190-day limit.
5.0 billion in costs over 10 years]
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Do you have to pay late enrollment penalty for Medicare?
In general, you'll have to pay this penalty for as long as you have a Medicare drug plan. The cost of the late enrollment penalty depends on how long you went without Part D or creditable prescription drug coverage. Learn more about the Part D late enrollment penalty.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.