Does Medicare require a copay?
After you meet the Part B deductible , you also pay 20% of the Medicare-Approved Amount for your doctor's services. If your doctor admits you to the same hospital for a related condition within 3 days of your emergency department visit, you don't pay the copayment because your visit is considered part of your inpatient stay.
Will Medicare/medicade Cover my copay?
Jan 14, 2022 · In most cases, if you receive care in a hospital emergency department and are covered by Medicare Part B, you'll also be responsible for: An annual Part B deductible of $233 (in 2022). A coinsurance payment of 20% of the Medicare-approved amount for most doctor’s services and medical equipment. How You Pay For Outpatient Services
What does the 'emergency room copay' mean?
Sep 20, 2018 · When Medicare covers emergency room (ER) visit costs, you typically pay: A copayment for the visit itself A copayment for each hospital service you receive there A coinsurance amount of 20% for the Medicare-approved cost for doctor services. The Part B deductible applies.
Do you have to pay copay for emergency room visit?
May 04, 2022 · In addition to these copays, you will pay a coinsurance for doctor services you receive in the ER. Medicare Part B typically pays 80 percent of the Medicare-approved amount for doctor services, and you are responsible for the remaining 20 percent of the cost. The Part B deductible also applies.

Does Medicare Part A cover an emergency room visit?
What is your copay with Medicare?
What is the copay on Medicare Part B?
Does Medicare cover 100% of hospital costs?
What is the Medicare deductible for 2021 Part B?
The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.Nov 12, 2021
What is the Medicare deductible for 2020?
How do I get my $144 back from Medicare?
Do you have a deductible with Medicare?
How does the Medicare Part B deductible work?
What is the Medicare 2 midnight rule?
What is not covered under Medicare Part A?
What is a copay for emergency room?
What is the Copay for Medicare Emergency Room Coverage? A copay is the fixed amount that you pay for covered health services after your deductible is met. In most cases, a copay is required for doctor’s visits, hospital outpatient visits, doctor’s and hospital outpatients services, and prescription drugs. Medicare copays differ from coinsurance in ...
Does Medicare cover emergency room visits?
Medicare does cover emergency room visits. You'll pay a Medicare emergency room copay for the visit itself and a copay for each hospital service. It is important to remember, however, that your actual Medicare urgent care copay amount can vary widely, depending on the services you require and where you receive care.
What are the services covered by Medicare?
Most ER services are considered hospital outpatient services, which are covered by Medicare Part B. They include, but are not limited to: 1 Emergency and observation services, including overnight stays in a hospital 2 Diagnostic and laboratory tests 3 X-rays and other radiology services 4 Some medically necessary surgical procedures 5 Medical supplies and equipment, like splints, crutches and casts 6 Preventive and screening services 7 Certain drugs that you wouldn't administer yourself
Does Medicare cover hospital stays?
If you are admitted for inpatient hospital services after an emergency room visit, Medicare Part A does help cover costs for your hospital stay. Medicare Part A does not cover emergency room visits that don't result in admission for an inpatient hospital stay.
How much is the deductible for Medicare Part B?
In most cases, if you receive care in a hospital emergency department and are covered by Medicare Part B, you'll also be responsible for: An annual Part B deductible of $203 (in 2021). A coinsurance payment of 20% of the Medicare-approved amount for most doctor’s services and medical equipment.
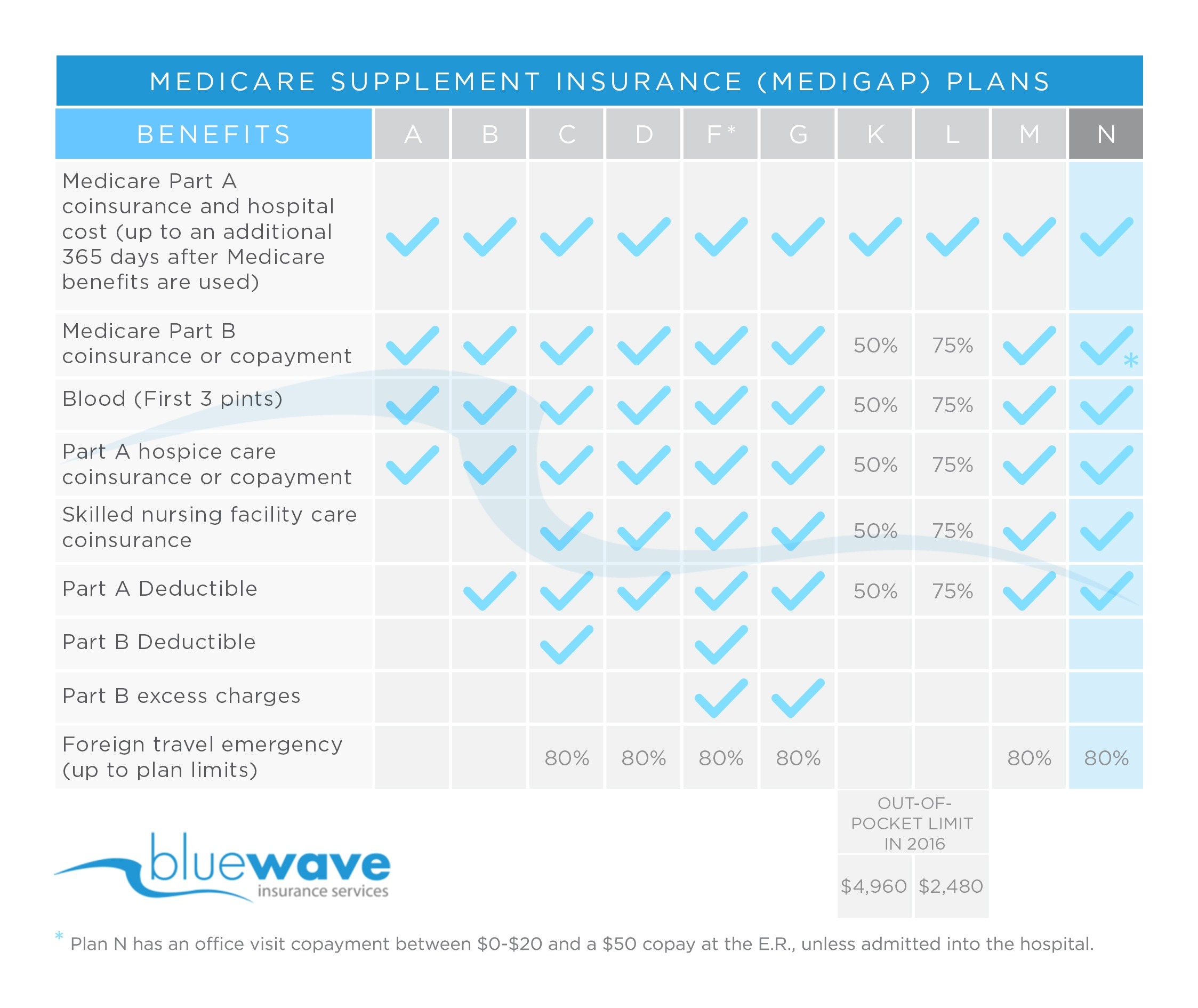
What is a Medigap plan?
Medigap is private health insurance that Medicare beneficiaries can buy to cover costs that Medicare doesn't, including some copays. All Medigap plans cover at least a percentage of your Medicare Part B coinsurance or ER copay costs.
What is the OPPS payment?
The OPPS pays hospitals a set amount of money (or payment rate) for the services they provide to Medicare beneficiaries. The payment rate varies from hospital to hospital based on the costs associated with providing services in that area, and are adjusted for geographic wage variations.
Does Medicare cover ER visits?
Medicare coverage of emergency room costs. If you have a situation such as a heart attack, stroke, or sudden illness, Medicare Part B might cover some of your emergency room costs. When Medicare covers emergency room (ER) visit costs, you typically pay: A copayment for the visit itself.
Is an emergency room visit more expensive than a doctor?
That means that if you’re in the 65-and-over age group, your chances of an emergency room visit are something to consider. And emergency room visit costs are generally higher than a visit to your doctor, reported the U.S. Agency for Healthcare Research and Quality (AHRQ).
Does Medicare Supplement cover emergency care?
In fact, some Medicare Supplement plans may help cover emergency medical care when you’re out of the country (80% of covered services up to plan limits).
Do you pay copays for ER visits?
For example, you may pay copays or coinsurance for an ER visit and for services you receive while in the ER. Some plans also have deductibles. It’s important to check each plan’s details for information about coverage for ER visits.
Does Medicare cover ER visits?
Yes, Medicare covers emergency room visits for injuries, sudden illnesses or an illness that gets worse quickly. Specifically, Medicare Part B will cover ER visits. And, since emergencies may occur anytime and anywhere, Medicare coverage for ER visits applies to any ER or hospital in the country. Note though, Medicare only covers emergency services ...
What percentage of Medicare Part B is paid for doctor services?
In addition to these copays, you will pay a coinsurance for doctor services you receive in the ER. Medicare Part B typically pays 80 percent of the Medicare-approved amount for doctor services, and you are responsible for the remaining 20 percent of the cost. The Part B deductible also applies.
Does Medicare Advantage cover out of network providers?
So, though Medicare Advantage plans typically have provider networks, they must cover emergency care from both network and out-of-network providers. In other words, Medicare Advantage plans cover ER visits anywhere in the U.S. Each Medicare Advantage plan sets its own cost terms for ER visits and other covered services.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
Do you have to pay for copay for emergency room?
Tip: If you happen to be admitted into the hospital within three days of your emergency room visit, your visit will be considered as part of your inpatient stay. You won’t have to pay the copayment for the emergency room.
Does Medicare Advantage cover emergency room visits?
Does Medicare Advantage Cover the Costs of an Emergency Room Visit? Since Advantage plans are required to cover the same costs as Original Medicare, they also cover emergency room visits. The only difference between Advantage plans and Original Medicare is your out of pocket costs are different and less predictable.
Does Part A cover all expenses?
As stated above, Part A doesn’t cover all your costs in the emergency room. You’ll have to pay the deductible before your coverage kicks in. After you met the deductible, Part A will cover 100% of the costs for 60 days. After 60 days, you’ll have coinsurance to pay for each day you stay in the hospital.
How long does Part A cover hospital expenses?
You’ll have to pay the deductible before your coverage kicks in. After you met the deductible, Part A will cover 100% of the costs for 60 days. After 60 days, you’ll have coinsurance to pay for each day you stay in the hospital.
Does Medigap cover coinsurance?
Medigap plans will cover any services that Original Medicare covers. Medigap plans cover the gaps in coverage with Medicare. Depending on the letter plan you choose, your Part A deductible and all cost-sharing could be covered at 100%. This includes coverage for any coinsurance for hospital stays after 60 days.
What does Part B cover?
Part B typically covers emergency services when you have an injury, a sudden illness, or illnesses that get significantly worse in a short period of time. This will also cover your physician follow-up appointments after receiving treatment from the emergency room or urgent care center.
Does Medicare cover emergency care?
Medicare Supplement, or Medigap. Medicare supplement, or Medigap, policies may provide emergency health coverage if a person is traveling outside the United States. Traditional Medicare does not traditionally cover costs for emergency care if a person is traveling outside the country.
Does Medicare cover ER visits?
Medicare Part B usually covers emergency room (ER) visits, unless a doctor admits a person to the hospital for a certain length of time. For inpatient admissions, Medicare Part A may cover the ER visit and subsequent hospital stay if the length of admission into hospital spans at least 2 midnights. In this article, we break down how Medicare ...
What does Medicare Part A cover?
Medicare Part A provides hospital coverage. If a doctor admits an individual into the hospital for at least 2 midnights, Medicare Part A covers hospital services, such as accommodation costs and testing, while a person stays in the facility.
How long does it take to go back to the ER?
A person goes to the ER, and the doctor discharges them. The health problem returns, and the individual needs to go back to the ER within 3 days. The doctor admits the person. In this example, Medicare Part A would pay for the hospital stay.
Do you pay for an emergency room visit with Medicare?
Typically, you pay a Medicare emergency room copayment for the visit itself and a copayment for each hospital service. How you are charged depends on several factors, including which part of Medicare covers your visit (Medicare Part A, Medicare Part B or both) and whether or not you have met your Part A and Part B deductibles.
Does Medicare cover emergency room visits?
Learn more and find the Medicare plan that offers the coverage you need. Yes, emergency room visits are typically covered by Medicare. Most outpatient emergency room services are covered by Medicare Part B, and inpatient hospital stays are covered by Medicare Part A.
Does Medicare cover inpatients?
If you go to the emergency room and are admitted as an inpatient, Medicare Part A helps cover some of the costs related to your hospital stay once your Part A deductible is met.
Is hospice a Medicare Part A?
Hospice care. Some home health care services . Medicare Part A is typically premium-free, as long as you or your spouse paid sufficient Medicare taxes while working. If you go to the emergency room and are admitted as an inpatient, Medicare Part A helps cover some of the costs related to your hospital stay once your Part A deductible is met.
Is Medicare Part A premium free?
Some home health care services. Medicare Part A is typically premium-free, as long as you or your spouse paid sufficient Medicare taxes while working . If you go to the emergency room and are admitted as an inpatient, Medicare Part A helps cover some of the costs related to your hospital stay once your Part A deductible is met.
How much is Medicare Part A deductible for 2021?
In 2021, the Medicare Part A deductible is $1,484 per benefit period.
Does Medicare Part B cover medical expenses?
If you go to the emergency room and receive care from a doctor but are not admitted as an inpatient, Medicare Part B will typically cover a portion of your medical costs.
What Does Part A of Medicare Cover?
Part A of Medicare covers inpatient care in a hospital. If you have a hospital stay that doesn't involve receiving inpatient care, it will not be covered by Medicare Part A. Part A also covers skilled nursing facility care, hospice care, some in-home health care, and nursing home care.
What Is the Difference Between Inpatient and Outpatient Care?
Understanding the difference between inpatient and outpatient care is important because this often determines which part of Medicare will cover your medical fees. Inpatient care involves receiving medical care overnight and specifically requires the length of your stay to be directly related to your medical care.
Lengthy Outpatient Stays and MOON Forms
If you are staying at an emergency room or hospital setting for over 24 hours but are not receiving inpatient care, then the hospital will be required to give you a Medicare Outpatient Observation Notice, or MOON form.
The Two-Midnight Rule
A general rule that determines inpatient designation is known colloquially as the “two-midnight rule”. If your doctor expects you to stay in the hospital for a time period that crosses two midnights, then you will be admitted as an inpatient.
When Will Part A Cover Emergency Room Visits?
Although Part A doesn’t always cover emergency room visits, there are situations where it will. Specifically, if you are admitted to the same hospital within three days of your initial emergency room visit.
Part B Coverage: Emergency Room Visits With No Hospital Admission
If you go to the emergency room and are treated as an outpatient, then you will receive Medicare coverage under Part B, not Part A. In this scenario, your coverage will function the same way as if you were at your normal doctor’s office.
Medicare Part B: Additional Fees
You will be responsible for a copayment for each visit, as well as 20 percent of the Medicare-approved amount. Your Part B deductible will also apply for outpatient visits to emergency rooms. If you receive a MOON form, that is one way to know that you will be responsible for these fees.