Full Answer
How do you calculate Medicare penalty?
Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these:
- Social Security
- Railroad Retirement Board
- Office of Personnel Management
Why is there a late enrollment penalty for Medicare?
medicare beneficiaries may incur a late enrollment penalty (lep) if there is a continuous period of 63 days or more at any time after the end of the individual's part d initial enrollment period during which the individual was eligible to enroll, but was not enrolled in a medicare part d plan and was not covered under any creditable prescription …
How do you calculate Medicare late enrollment penalty?
- A Part D plan
- Prescription coverage through a Medicare Advantage plan
- Any other Medicare plan that includes Medicare PDP coverage
- Another healthcare plan that includes prescription drug coverage that is at least as good as the coverage provided by Medicare.
What is the penalty for not taking part B Medicare?
Those who do not sign up for Medicare Part B when they’re first eligible and don’t qualify for a Special Enrollment Period may be subject to a late enrollment penalty. This could mean paying a 10% higher monthly premium for every 12-month period that you were eligible for Part B but didn’t enroll.

How is Medicare penalty calculated?
Medicare calculates the penalty by multiplying 1% of the "national base beneficiary premium" ($33.37 in 2022) times the number of full, uncovered months you didn't have Part D or creditable coverage. The monthly premium is rounded to the nearest $. 10 and added to your monthly Part D premium.
Is there a cap on Medicare Part B penalty?
As of now, there is no cap when calculating the Medicare Part B late enrollment penalty. However, legislation has been introduced to cap the Medicare Part B penalty at 15% of the current premium, regardless of how many 12-month periods the beneficiary goes without coverage.
How long does Medicare Part D penalty last?
Since the monthly penalty is always rounded to the nearest $0.10, she will pay $9.70 each month in addition to her plan's monthly premium. Generally, once Medicare determines a person's penalty amount, the person will continue to owe a penalty for as long as they're enrolled in Medicare drug coverage.
How do I avoid Medicare Part B penalty?
If you don't qualify to delay Part B, you'll need to enroll during your Initial Enrollment Period to avoid paying the penalty. You may refuse Part B without penalty if you have creditable coverage, but you have to do it before your coverage start date.
How is Medicare Part B penalty calculated?
Calculating Lifetime Penalty Fees Calculating your Part B penalty is fairly straightforward. You simply add 10% to the cost of your monthly premium for each year-long period you didn't have Medicare. It's simple to get a snapshot of what you will have to pay each month.
Can Medicare penalties be waived?
You may qualify to have your penalty waived if you were advised by an employee or agent of the federal government – for example by Social Security or 1-800-MEDICARE – to delay Part B. Asking for the correction is known as requesting equitable relief.
How do I get rid of Part D Penalty?
3 ways to avoid the Part D late enrollment penaltyEnroll in Medicare drug coverage when you're first eligible. ... Enroll in Medicare drug coverage if you lose other creditable coverage. ... Keep records showing when you had other creditable drug coverage, and tell your plan when they ask about it.
What is the maximum Part D Penalty?
The Part D penalty has no cap. For example: The national average premium is $33.37 a month in 2022. If you went 29 months without creditable coverage, your penalty would be $9.70.
What is the cost of Part D Medicare for 2022?
$33Part D. The average monthly premium for Part coverage in 2022 will be $33, up from $31.47 this year. As with Part B premiums, higher earners pay extra (see chart below). While not everyone pays a deductible for Part D coverage — some plans don't have one — the maximum it can be is $480 in 2022 up from $445.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
What is the Medicare Part B premium for 2022?
$170.102022. The standard Part B premium amount in 2022 is $170.10. Most people pay the standard Part B premium amount.
At what income level do Medicare premiums increase?
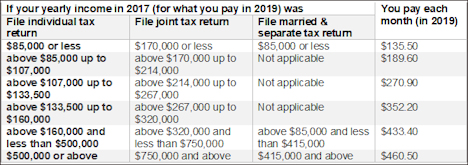
For example, when you apply for Medicare coverage for 2022, the IRS will provide Medicare with your income from your 2020 tax return. You may pay more depending on your income. In 2022, higher premium amounts start when individuals make more than $91,000 per year, and it goes up from there.
What happens if Medicare decides the penalty is wrong?
What happens if Medicare's contractor decides the penalty is wrong? If Medicare’s contractor decides that all or part of your late enrollment penalty is wrong, the Medicare contractor will send you and your drug plan a letter explaining its decision. Your Medicare drug plan will remove or reduce your late enrollment penalty. ...
What is the late enrollment penalty for Medicare?
Part D late enrollment penalty. The late enrollment penalty is an amount that's permanently added to your Medicare drug coverage (Part D) premium. You may owe a late enrollment penalty if at any time after your Initial Enrollment Period is over, there's a period of 63 or more days in a row when you don't have Medicare drug coverage or other.
What happens if Medicare pays late enrollment?
If Medicare’s contractor decides that your late enrollment penalty is correct, the Medicare contractor will send you a letter explaining the decision, and you must pay the penalty.
What is creditable prescription drug coverage?
creditable prescription drug coverage. Prescription drug coverage (for example, from an employer or union) that's expected to pay, on average, at least as much as Medicare's standard prescription drug coverage. People who have this kind of coverage when they become eligible for Medicare can generally keep that coverage without paying a penalty, ...
How long do you have to pay late enrollment penalty?
You must do this within 60 days from the date on the letter telling you that you owe a late enrollment penalty. Also send any proof that supports your case, like a copy of your notice of creditable prescription drug coverage from an employer or union plan.
How long does it take for Medicare to reconsider?
In general, Medicare’s contractor makes reconsideration decisions within 90 days. The contractor will try to make a decision as quickly as possible. However, you may request an extension. Or, for good cause, Medicare’s contractor may take an additional 14 days to resolve your case.
Do you have to pay a penalty on Medicare?
After you join a Medicare drug plan, the plan will tell you if you owe a penalty and what your premium will be. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
Why is Medicare charging late fees?
Charging late fees helps to reduce these costs overall and encourage people to enroll on time.
What happens if you delay Medicare enrollment?
Delaying enrollment in Medicare can subject you to long-lasting financial penalties added to your premiums each month. A late enrollment penalty can significantly increase the amount of money you’re required to pay for each part of Medicare for years. Share on Pinterest.
How long does it take to enroll in Medicare Part D?
You can enroll in Medicare Part D without incurring a late enrollment penalty during the 3-month period that begins when your Medicare parts A and B become active. If you wait past this window to enroll, a late enrollment penalty for Medicare Part D will be added to your monthly premium. This fee is 1 percent of the average monthly prescription ...
What happens if you don't sign up for Medicare?
If you’re not automatically enrolled and don’t sign up for Medicare Part A during your initial enrollment period, you’ll incur a late enrollment penalty when you do sign up. The late enrollment penalty amount is 10 percent of the cost of the monthly premium. You’ll have to pay this additional cost each month for twice the number ...
How long does Medigap last?
This period starts on the first day of the month you turn 65 and lasts for 6 months from that date. If you miss open enrollment, you may pay a much higher premium for Medigap.
How long does Medicare Part B take to enroll?
Part B late enrollment penalty. You’re eligible for Medicare Part B starting 3 months before your 65th birthday until 3 months after it occurs. This period of time is known as the initial enrollment period.
How long do you have to enroll in Medicare?
make sure to enroll during the 8-month period when your current coverage ends, known as a special enrollment period.
How much is Part A late penalty?
Part A late penalties amount to an extra 10 percent of your current Part A premium added to the premium. Part A premiums are expensive — in 2020, they are $252 a month if you’ve earned 30 to 39 work credits, or $458 a month if you have fewer than 30 credits. However, unlike Part B late penalties, that 10 percent is not multiplied by the number ...
How long can you delay Medicare enrollment?
For example, if you delayed enrollment for three years, you’d pay penalties for six years. There are some exceptions: If you receive health care coverage from an employer for which you or your spouse actively works, you have the right to delay Part A as well as Part B enrollment until the employment ends. By that time, if you or your spouse has ...
Do you pay Medicare payroll taxes if you have 40 credits?
En español | If you or your spouse has earned at least 40 credits through paying Medicare payroll taxes at work, you are automatically entitled to Part A benefits (which cover stays in the hospital, home health services and hospice care) and you do not pay premiums for them.
How much is the penalty for Medicare Part B?
For each 12-month period you delay enrollment in Medicare Part B, you will have to pay a 10% Part B premium penalty, unless you have insurance based on your or your spouse’s current work (job-based insurance) or are eligible for a Medicare Savings Program (MSP) .
How much is the Part B penalty for 2021?
Since the base Part B premium in 2021 is $148.50, your monthly premium with the penalty will be $252.45 ($148.50 x 0.7 + $148.50). Note: Although your Part B premium amount is based on your income, your penalty is calculated based on the base Part B premium. The penalty is then added to your actual premium amount.
Do you have to pay Medicare premium penalty every month?
In most cases, you will have to pay that penalty every month for as long as you have Medicare. If you are enrolled in Medicare because of a disability and currently pay premium penalties, once you turn 65 you will no longer have to pay the premium penalty.
Medicare Advantage Plan (Part C)
Monthly premiums vary based on which plan you join. The amount can change each year.
Medicare Supplement Insurance (Medigap)
Monthly premiums vary based on which policy you buy, where you live, and other factors. The amount can change each year.
How much is Medicare Part B 2021?
For Part B coverage, you’ll pay a premium each year. Most people will pay the standard premium amount. In 2021, the standard premium is $148.50. However, if you make more than the preset income limits, you’ll pay more for your premium.
What is Medicare Part B?
Medicare Part B. This is medical insurance and covers visits to doctors and specialists, as well as ambulance rides, vaccines, medical supplies, and other necessities.
What is the Medicare Part D premium for 2021?
Part D plans have their own separate premiums. The national base beneficiary premium amount for Medicare Part D in 2021 is $33.06, but costs vary. Your Part D Premium will depend on the plan you choose.
How does Social Security determine IRMAA?
The Social Security Administration (SSA) determines your IRMAA based on the gross income on your tax return. Medicare uses your tax return from 2 years ago. For example, when you apply for Medicare coverage for 2021, the IRS will provide Medicare with your income from your 2019 tax return. You may pay more depending on your income.
How many types of Medicare savings programs are there?
Medicare savings programs. There are four types of Medicare savings programs, which are discussed in more detail in the following sections. As of November 9, 2020, Medicare has not announced the new income and resource thresholds to qualify for the following Medicare savings programs.
How much do you need to make to qualify for SLMB?
If you make less than $1,296 a month and have less than $7,860 in resources, you can qualify for SLMB. Married couples need to make less than $1,744 and have less than $11,800 in resources to qualify. This program covers your Part B premiums.
Does Medicare change if you make a higher income?
If you make a higher income, you’ll pay more for your premiums, even though your Medicare benefits won’t change.
