
How much did a hospital charge for trauma activation?
Two years later, the bill finally arrived at their home: They owed the hospital $18,836 for a visit lasting three hours and 22 minutes, the bulk of which was for a mysterious fee for $15,666 labeled “trauma activation,” also known as “a trauma response fee.”
How much does Medicare pay for trauma care?
On average, Medicare pays just $957.50 for the fee. According to Medicare guidelines, the fee can be charged only when the patient receives at least 30 minutes of critical care provided by a trauma team — but hospitals do not appear to be following that rule when billing non-Medicare patients. At the turn of the century such fees didn’t even exist.
What is the CPT code for trauma activation for Medicare?
Trauma activation for Medicare has to meet the criteria based on CMS guidelines. The code used for trauma activation with critical care is G0390. Not all payors take this code, but Medicare does. There needs to be at least 31 minutes of facility-based critical care in order to qualify for the G0390.
What is a trauma fee?
A trauma fee is the price a trauma center charges when it activates and assembles a team of medical professionals that can meet a patient with potentially serious injuries in the ER. It is billed on top of the hospital’s emergency room physician charge and procedures, equipment and facility fees.
What is trauma activation fee?
What is the revenue code for trauma hospitals?
How many trauma centers are there in Connecticut?
What are the factors that affect trauma care?
When did hospitals become trauma centers?
What is ASC in trauma?
See 3 more topics
About this website
Does Medicare pay for trauma activation?
Trauma activation for Medicare has to meet the criteria based on CMS guidelines. The code used for trauma activation with critical care is G0390. Not all payors take this code, but Medicare does. There needs to be at least 31 minutes of facility-based critical care in order to qualify for the G0390.
What is trauma activation?
Trauma Team Activation and Evaluation Criteria Purpose. To identify those patients with actual or potential serious injuries based on physiological changes altered anatomy, mechanism of injury and risk factors.
Can you bill trauma activation without critical care?
A trauma team must provide at least 30 minutes of critical care before the hospital can bill for a trauma activation, so failure to capture critical care charges will reduce trauma program revenue dramatically.
What is a level 2 trauma activation?
Second-Level Trauma Activations – Urgent. The second level of response, defined in hospital policy, may include a partial team response and typically is based on anatomic criteria, mechanism of injury and/ or special considerations. In-house response is within 15 minutes of notification.
What is a Level 1 trauma activation?
In Level I and II trauma centers, the highest level of activation requires the response of the full trauma team within 15 minutes of arrival of the patient, and the criteria should include physiologic criteria and some or several of the anatomic criteria (CD 5–14).
What are the 3 levels of trauma?
Trauma centers vary in their specific capabilities and are identified by "Level" designation: Level I (Level-1) being the highest and Level III (Level-3) being the lowest (some states have five designated levels, in which case Level V (Level-5) is the lowest).
What is the CPT code for trauma Response Level 2?
The established trauma revenue codes are: 0681 for Level I. 0682 for Level II.
What are trauma CPT codes?
When critical care services are provided without trauma activation, the hospital may bill CPT code 99291, Critical care, evaluation and management of the critically ill or critically injured patient; first 30-74 minutes (and 99292, if appropriate).
What is a code 2 trauma?
A Level II Trauma Center is able to initiate definitive care for all injured patients. Elements of Level II Trauma Centers Include: 24-hour immediate coverage by general surgeons, as well as coverage by the specialties of orthopedic surgery, neurosurgery, anesthesiology, emergency medicine, radiology and critical care.
What is the difference between a Level 1 and Level 2 trauma center?
There are several minor differences between a level I and II trauma center but the main difference is that the level II trauma center does not have the research and publication requirements of a level I trauma center.
What is a Category 1 trauma?
Patients with the most serious injuries are designated a level 1 trauma, indicating a need for a larger trauma team and faster response time. The determination of trauma code criteria varies between hospitals and is based on elements such as physiologic data, types of injury, and mechanism of injury.
What is the best trauma hospital in the United States?
Baylor Scott & White Medical Center—Temple Trauma Center Recognized among the Best in North America.
Billing and Coding Guidelines - CMS
inpatient (see Pub. 100-02, Medicare Benefit Policy Manual, Chapter 1, §10 “Covered Inpatient Hospital Services Covered Under Part A. C. Notification of Beneficiary All hospital observation services, regardless of the duration of the observation care, that are medically reasonable and necessary are covered by Medicare, and
Trauma System Activation – Trauma Code Criteria
CLINICAL MANUAL Policy Number: CM T -28 Approved by: Executive Leadership Team Issue Date: 09/1999 Applies to: Downtown Value(s): Respect, Integrity, Innovation Page(s): 1 of 5 Trauma System Activation – Trauma Code Criteria Review Date: Change Description: 02/26/2018
CPT/HC Provider Chronic Revenue Major Category General Psychiatric PC ...
X: X X: 253 Pharmacy - Take home drugs (LARCs only) X X; 254 Pharmacy - Drugs Incident to other Diagnostic Serv X; X 255; Pharmacy - Drugs Incident to Radiology X
CMS Manual System Department of Health & Human Services (DHHS) Pub. 100 ...
Attachment - Business Requirements Pub. 100-04 Transmittal: 36 Date: November 28, 2003 Change Request 2995 SUBJECT: Revenue Code 068X I. GENERAL INFORMATION
Why do hospitals charge for trauma activations?
I can understand hospitals charging a fee for trauma activations to help recover some of the costs of having a trauma service. The staff may require some special training. Managing the service, collecting data, and other incidentals may increase costs. However, nearly all of the personnel involved in a trauma activation are already in the hospital and receive their salaries whether trauma activations occur or not. In the above examples, I would guess most members of the team spent 0 to 5 minutes at the patient’s bedside.
What is trauma activation?
A trauma activation involves paging a number of hospital staff to go to the emergency department as quickly as possible. Those paged may include an attending surgeon, two or three surgical residents, an anesthesiologist or anesthesia resident, a respiratory therapist, a critical care nurse, and operating room nurse, and x-ray technician, ...
What is the over triage rate for a cut on the head?
The American College of Surgeons told Vox that to avoid missing a seriously injured patient a 25-35% over triage rate is acceptable. I agree with that, but it doesn’t mean a five-figure trauma activation fee is warranted for a patient with a cut on his head requiring two staples.
What is trauma team?
The trauma team assesses the patient and if serious injuries are present, expeditiously diagnoses and treats the problem. But in cases like the one described above, the team quickly disperses and returns to their usual duties.
How much does Medicare pay for trauma?
On average, Medicare pays just $957.50 for the fee. According to Medicare guidelines, the fee can be charged only when the patient receives at least 30 minutes of critical care provided by a trauma team — but hospitals do not appear to be following that rule when billing non-Medicare patients.
What is trauma fee?
A trauma fee is the price a trauma center charges when it activates and assembles a team of medical professionals that can meet a patient with potentially serious injuries in the ER. It is billed on top of the hospital’s emergency room physician charge and procedures, equipment and facility fees.
What are multiplying fees in hospitals?
American hospital bills are today littered with multiplying fees, many of which don’t even exist in other countries: fees for blood draws, fees for checking the blood oxygen level with a skin probe, fees for putting on a cast, minute-by-minute fees for lying in the recovery room.
How much does a hospital cost for trauma?
Comprehensive data from the Health Care Cost Institute shows that the average price that health insurers paid hospitals for trauma response (which is often lower than what the hospital charges) was $3,968 in 2016. But hospitals in the lowest 10 percent of prices received an average of $725 — while hospitals in the most expensive 10 percent were paid $13,525.
When was the trauma response fee first approved?
Trauma response fees were first approved by the National Uniform Billing Committee in January 2002 , following a push by a national consulting firm specializing in trauma care. The high costs of staffing a trauma team available at all hours, the firm argued, threatened to shut down trauma centers across the country.
Did fees exist at the turn of the century?
At the turn of the century such fees didn’t even exist.
Why is trauma activation important?
And knowing how to handle the different types of trauma activations will be essential in contracting with payors, and ultimately, in price transparency as we move forward.
What is the trauma level in a hospital?
Every hospital is assigned a trauma level sub-code from 4 to 1 , with 1 being the highest level of trauma capability – there are usually only two or three such facilities per state.
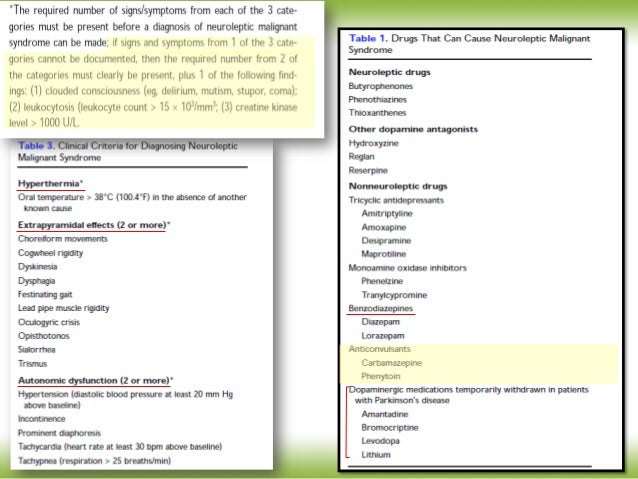
What are the requirements for Medicare?
Most payors follow Medicare activation requirements. One consistent requirement beyond Medicare’s requirements for private payors is to use the American College of Surgeons standard as documented in the Resources for the Optimal Care of the Injured Patient (2006). This document specifies that the minimum criteria for the definition of a major trauma patient include one of the following (documented) conditions: 1 Confirmed systolic blood pressure of <90mmHg in adults and age-specific hypotension in children 2 Respiratory compromise, obstruction or intubation 3 Use of blood products to maintain vital signs in patients transferred from other hospitals 4 Discretion of the emergency physician 5 Gunshot wounds to abdomen, neck, or chest 6 Glasgow Coma Score less than 8 with mechanism attributed to trauma
How many minutes of critical care is required for a G0390?
There needs to be at least 31 minutes of facility-based critical care in order to qualify for the G0390. This means face-to-face care with resources belonging to the facility, not the physician. While it may not match exactly with physician timing, it does include face-to-face time with nursing and ancillary care.
Do trauma activations need to be prehospital?
We’ve bolded the statement about prehospital notification, as this is a must for a trauma activation. Our auditors sometimes see activations with patients who have walked into the ER on their own power, or activations documented in peculiar circumstances. For example, we’ve seen activations take place in an elevator on the way to surgery.
Does Medicare require activation?
Most payors follow Medicare activation requirements. One consistent requirement beyond Medicare’s requirements for private payors is to use the American College of Surgeons standard as documented in the Resources for the Optimal Care of the Injured Patient (2006). This document specifies that the minimum criteria for the definition of a major trauma patient include one of the following (documented) conditions:
Is trauma activation expensive?
With the ever-increasing attention to price transparency as a backdrop, charges for trauma activation — which can be quite expensive — are increasingly subject to public scrutiny and questioning. ( This article in Vox is a good example.) Every hospital needs to know its trauma activation policies and protocols, but as you will see, it’s also a topic well worth exploring from a revenue cycle perspective.
How often do hospitals charge trauma alert fees?
Tens of thousands of times a year, hospitals charge enormously expensive trauma alert fees for injuries so minor the patient is never admitted. In Florida alone, where the number of trauma centers has exploded, hospitals charged such fees more than 13,000 times in 2019 even though the patient went home the same day, ...
When did hospitals start billing trauma teams?
Hospitals began billing trauma team fees to insurers of all kinds after Medicare authorized them starting in 2008 for cases in which hospitals are notified of severe injuries before a patient arrives.
How long do you have to give a trauma team?
Under rules established by Medicare and a committee of insurers and health care providers, emergency departments must give 30 minutes of critical care after a trauma alert to be paid for activating the team. For inpatients, the trauma team fee is sometimes folded into other charges, billing consultants say.
What was the patient's lawsuit in the Sutter case?
In the Sutter case in Modesto, the patient sued a driver who struck his vehicle, seeking damages from the driver and her insurer. Patient “looks good,” an emergency doctor wrote in the records, which were part of the trial evidence. He prescribed Tylenol with hydrocodone for pain.
How are insurance charges passed on?
The charges are passed on through higher insurance premiums and expenses paid not just by health insurers but also auto insurers, who often are first in line to pay for the care of a crash victim. Audits are uncommon and often the system is geared to paying claims with little or no scrutiny, billing specialists say.
Can hospitals charge for trauma activation?
Hospitals can charge trauma activation fees when a crack squad of doctors and nurses assembles after an ambulance crew says it’s approaching with a patient who needs trauma care. The idea is that life-threatening injuries need immediate attention and that designated trauma centers should be able to recoup the cost of having a team ready — even if it never swings into action.
Do hospitals release trauma alerts the same day?
At some hospitals , few patients whose cases generate trauma alerts are treated and released the same day.
How many times do trauma centers charge fees in Florida?
In Florida alone, where the number of trauma centers has exploded, hospitals charged such fees more than 13,000 times in 2019 even though the patient went home the same day, according to a KHN analysis of state data provided by Etienne Pracht, an economist at the University of South Florida. Those cases accounted for more than a quarter ...
How often do hospitals charge trauma alert fees?
Tens of thousands of times a year, hospitals charge enormously expensive trauma alert fees for injuries so minor the patient is never admitted. The emergency entrance of a hospital in Philadelphia in 2019. In Florida alone, where the number of trauma centers has exploded, hospitals charged such fees more than 13,000 times in 2019 ...
How long do you have to give a trauma team?
Under rules established by Medicare and a committee of insurers and health care providers, emergency departments must give 30 minutes of critical care after a trauma alert to be paid for activating the team. For inpatients, the trauma team fee is sometimes folded into other charges, billing consultants say.
When did hospitals start billing for trauma?
Hospitals began billing trauma team fees to insurers of all kinds after Medicare authorized them starting in 2008 for cases in which hospitals are notified of severe injuries before a patient arrives. Instead of leaving trauma team alerts to the paramedics, hospitals often call trauma activations themselves based on information from the field, trauma surgeons say.
How are insurance charges passed on?
The charges are passed on through higher insurance premiums and expenses paid not just by health insurers but also auto insurers, who often are first in line to pay for the care of a crash victim. Audits are uncommon and often the system is geared to paying claims with little or no scrutiny, billing specialists say.
Can trauma activation charges hit patients directly?
And trauma activation charges also can hit patients directly.
Can a hospital declare a trauma alert in Florida?
Florida regulations allow hospitals themselves to declare an “in-hospital trauma alert” for “patients not identified as a trauma alert” in the field, according to standards published by the Florida Department of Health. At some hospitals, few patients whose cases generate trauma alerts are treated and released the same day.
What happens during trauma team activation?
Think about what happens during a trauma team activation. The patient arrives with a high index of suspicion for critical injury. The trauma team provides continuous, face-to-face care to determine whether the patient has any hidden injuries or needs immediate intervention. Ultimately, the patient may prove not to have a critical need, but from a billing perspective that is beside the point. The time spent evaluating the patient is considered critical care.
How much time does a trauma team need to be on a critical care team?
According to the Centers for Medicare & Medicaid Services (CMS), a trauma team must provide at least 30 minutes of critical care in order to bill for a trauma team activation. Many billers think this means 30 minutes of physician time. In fact, CMS regulations state that critical care time can include care delivered by either physicians or hospital staff.
How long is CPT 99291?
CPT 99291 for the first 30 to 74 minutes of critical care (and CPT 99292 for each additional 30 minutes)
How long does a trauma team have to be in the hospital?
A trauma team must provide at least 30 minutes of critical care before the hospital can bill for a trauma activation, so failure to capture critical care charges will reduce trauma program revenue dramatically.
Is critical care billing misunderstood?
Unfortunately, critical care billing is widely misunderstood by both trauma program leaders and hospital finance departments. As a result, many trauma programs fail to capture a significant percentage of critical care charges. That leads to lost trauma response fees.
Can a trauma surgeon charge for critical care?
If a trauma surgeon spends only 20 minutes with a patient during an activation but the trauma team as a whole spends 45 minutes providing care: The surgeon cannot submit a professional charge for critical care . However, the hospital can submit a facility charge for critical care.
Can a hospital charge for trauma response fee?
If the team fulfills the requirements listed above, the hospital can submit a charge for the trauma response fee. When submitting this charge under revenue code 68x, the bill must also report:
What is trauma activation fee?
It is a one-time occurrence in association with deployment of the hospital’s specialized trauma response team. The related reimbursement for this occurrence is commonly known as a “trauma activation fee.” A primary purpose of the CMS trauma team activation codes and related fees payment system is to help trauma centers remain financially viable, given the significant cost burden associated with professional and administrative resources needed to achieve and maintain the advanced level of readiness and capability of their critical care services.
What is the revenue code for trauma hospitals?
Revenue code series 68x can be used only by trauma hospitals designated by the state or local government. Different subcategory revenue codes are reported by designated Level 1-4 hospital trauma hospitals. CMS created G0390, Trauma response team activation associated with hospital critical care service, effective January 1, 2007, which is assigned to APC 0618, and Critical Care with Trauma Response.
How many trauma centers are there in Connecticut?
Connecticut has 12 adult and/or pediatric trauma centers designated and licensed by the Department of Public Health The American College of Surgeons. The very rigorous trauma center re-verification process by the ACS takes place every three years.
What are the factors that affect trauma care?
A trauma center’s policies also may use other factors to optimize trauma care, including patient’s age, bleeding disorders, burns, end-stage renal disease, advanced pregnancy, time-sensitive extremity injuries, CPR, blunt force or penetrating trauma, and other similar elements.
When did hospitals become trauma centers?
Beginning in 2007, the Centers for Medicare and Medicaid Services (CMS) authorized hospitals designated as “trauma centers” to bill and receive payments for critical care services using specific codes and charges that capture the level of expertise and resources used in the triage and care of individual trauma patients.
What is ASC in trauma?
States designate and license trauma centers and the American College of Surgeons (ASC) verify if the designated centers have the resources listed in the Resources for Optimal Care of the Injured Patient on-site. Each center achieves and maintains its designation through a self-funded rigorous verification process administered by ACS.
