Full Answer
Is the ColoGuard test covered by Medicare?
Cologuard is covered by Medicare and Medicare Advantage with no co-pay or deductible for eligible patients ages 50-85. 80% Currently, >80% of Cologuard patients 45-49 have had no out-of-pocket cost for screening.*
Does Aetna Medicare cover Cologuard?
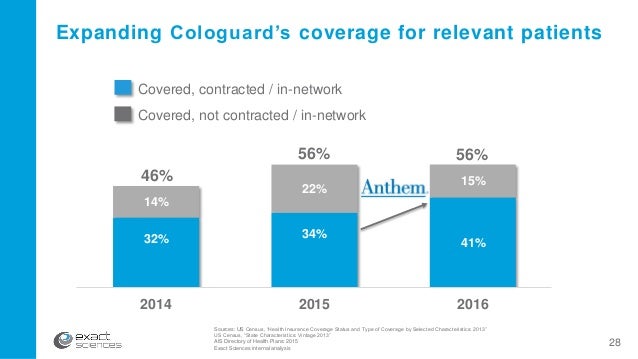
MADISON, Wis. — (BUSINESS WIRE) — Exact Sciences Corp. (NASDAQ:EXAS) today announced that Aetna, one of the country's leading health plans, will cover Cologuard under its Medicare Advantage plan, reaching 967,000 members across the country. The three year agreement will go into effect on April 1, 2015. Cologuard is the first and only FDA approved noninvasive stool-based DNA (sDNA) screening test for colon cancer.
What does insurances cover Cologuard?
What colorectal cancer screening tests does Medicare cover?
- Once every 2 years for those at high risk (regardless of age)
- Once every 10 years for those who are at average risk
- 4 years after a flexible sigmoidoscopy for those who are at average risk
Does insurance cover colonoscopy after Cologuard?
However, while the frequent TV ads do note that the Cologuard cost itself is covered by most insurance policies, they do not mention that a follow-up colonoscopy may not be covered. Conroy defended the messaging in the advertisements, calling them "appropriate."

Does Medicare pay for cologuard testing?
Medicare Part B covers the Cologuard™ test once every 3 years for people with Medicare who meet all of these conditions: Between 50 and 85 years old.
Does Medicare pay for both cologuard and colonoscopy?
Flexible sigmoidoscopy — once every four years (48 months) if you are age 50+ and at high risk, or once every 10 years after a colonoscopy if you are age 50+ and not at high risk. Cologuard — Medicare includes coverage for a Cologuard kit under specific circumstances.
How much is cologuard out-of-pocket?
The cost of Cologuard is around $500. Part of that cost may be covered by some insurances depending on your plan, co-pay, and deductible. Diagnostic testing is subject to deductibles and coinsurance. Screening colonoscopies are not subject to copays and deductibles and usually have no out-of-pocket costs for patients.
What is the total cost of cologuard?
Cologuard: The cost for the test ranges from $581 to $681, depending on when you pay. A call to the toll-free number, 844-870-8870, can get you a $100 discount if you pay in full upfront.
Does Medicare pay for colonoscopy after age 70?
Colonoscopies. Medicare covers screening colonoscopies once every 24 months if you're at high risk for colorectal cancer. If you aren't at high risk, Medicare covers the test once every 120 months, or 48 months after a previous flexible sigmoidoscopy. There's no minimum age requirement.
How Much Does Medicare pay towards a colonoscopy?
Original Medicare pays the full cost of a colonoscopy if a medical provider who accepts Medicare rates does the procedure. However, if a polyp is found and removed during the colonoscopy, the procedure is considered diagnostic rather than preventive and you likely will owe 20 percent of the Medicare-approved fee.
Why are colonoscopies not recommended after age 75?
“There are risks involved with colonoscopy, such as bleeding and perforation of the colon, and also risks involved with the preparation, especially in older people,” Dr.
At what age is Cologuard covered by insurance?
Stool DNA test (Cologuard): Covered at no cost* for those age 50 to 85 as long as they are not at increased risk of colorectal cancer and don't have symptoms of colorectal cancer (no co-insurance or Part B deductible).
Which is better colonoscopy or Cologuard?
Cologuard Test: Detection Not Prevention Cologuard can only detect 42% of large polyps, while a colonoscopy can detect 95% of large polyps. When polyps are detected during a colonoscopy they are removed at the same time.
Is Cologuard worth doing?
Cologuard's accuracy rate for detecting colorectal cancers and precancerous polyps is touted to be 92%. While that is impressive for a stool-based test, it still means that 8% of lesions will go undetected, leaving those patients with a false sense of security. Cologuard has a 14% false-positive rate.
Does Cologuard detect polyps?
Although the Cologuard test can detect signs of colorectal cancer or advanced colon polyps, it can't detect polyps in their earliest stages when they can be easily removed.
Is Cologuard cost effective?
The analysis found that Cologuard was cost effective and demonstrated the greatest reduction in CRC incidence and mortality versus FIT and FOBT. The results from the analysis were also published online in the Journal of Medical Economics.
Is colonoscopy covered after Cologuard?
The Affordable Care Act requires insurance companies to cover routine screening for colorectal cancer. However, most policies don't cover a Cologuard test and a colonoscopy.
Does Medicare cover colonoscopy prep?
Getting right to it, yes, Medicare pays for colonoscopies. Coverage includes a broad range of preventive care services, including screenings. Medicare Part B pays for colonoscopy coverage for screening services like colorectal cancer testing.
Will Cologuard replace colonoscopy?
Cologuard is not intended to replace diagnostic colonoscopy or surveillance colonoscopy in high-risk patients, including those with inflammatory bowel disease (IBD).
What is the cut off age for Cologuard?
Cologuard® Gains FDA Approval for Use in Younger Americans, Ages 45 to 49 | Exact Sciences.
How often does Part B cover Cologuard?
Part B will cover the Cologuard test once every three years if you meet the following criteria: At average risk. Age 50-85. Asymptomatic. You should have a good understanding of what will affect your screening for colorectal cancer. The Affordable Care Act requires insurance companies to abide by the USPSTF recommendations for coverage.
How much does a blood test cost?
The price of the test can range from $400-$600. Although, talking with your insurance provider can help; you can request fees for the test and laboratory be covered. You don’t know unless you ask. More than 92% of all patients have a $0 out-of-pocket cost for testing.
What is the best test for colorectal cancer?
All of which, suggest stool DNA tests (like Cologuard) for the detection of colorectal cancer.
What to do if you don't see your state on Cologuard?
If you don’t see your state, don’t worry because Cologuard is adding new states and plans all the time. Check back often, and if you’re considering canceling your test, call their Customer Care Center first. You can request more information about the financial assistance program that Exact Sciences offers.
Does exact sciences have Medicaid?
For the creators of Cologuard to submit claims to your state Medicaid plan for payment purposes, Exact Sciences Laboratories must be a Medicaid provider in your state. They’re not on contract with Medicare in every state; for instance, in New York, Cologuard is a preventative service for Medicaid members. Then, some states will allow Exact Sciences to contact directly Medicaid plans in the states they’re not participating.
Does Medicare cover colorectal screening?
Medicare is exempt from this requirement; beneficiaries might be responsible for paying coinsurance or co-payments. Look over your plan, make sure you have a good understanding of what type of insurance you have, and what service options your plan covers for colorectal screening, including Cologuard.
Can you get co-insurance with Medicare?
Most people with Medicare won’t be responsible for co-insurance if they get a Cologuard kit. Reaching the next stage of life presents new screenings that you should talk to your doctor about. One of several options is Cologuard; however, your doctor or healthcare provider must give you a prescription.
How often does Medicare pay for Cologuard?
Typically, Medicare Part B does pay for Cologuard tests every three years if you meet all of the following conditions: You have no personal history of colorectal cancer, inflammatory bowel disease or adenomatous polyps. You have no family history of hereditary nonpolyposis colorectal cancer, familial adenomatous polyposis, ...
How often is a barium enema covered by Medicare?
Barium enema. This test is covered by Medicare every 48 months if you are age 50 or older and every 24 months if you are at a high risk for colorectal cancer. Colonoscopy. This test is covered every 24 months if you are at a high risk for colorectal cancer. Fecal occult blood test.
How many Medigap plans are there?
In most states, there are 10 standardized Medigap plans to choose from, with a range of available basic benefits.
Can you get Cologuard if you have a family history?
You have no family history of hereditary nonpolyposis colorectal cancer, familial adenomatous polyposis, colorectal cancers or adenomatous polyps. Typically, you pay nothing for Cologuard (if it is prescribed by a doctor who accepts Medicare assignment).
Types Of Colorectal Cancer Screening
Because colon cancer begins as growths called polyps, finding and removingpolyps is the best way to prevent colon cancer. There are three types of CRC screening:
Colorectal Cancer Screening In Patients With Cystic Fibrosis
An UpToDate review on Cystic fibrosis: Overview of gastrointestinal disease states that The Cystic Fibrosis Foundation has developed Guidelines for Colorectal Cancer Screening for adults with CF. The guideline recommends colonoscopy for screening, beginning at age 40 years, or at 30 years for those who have had an organ transplant.
What Colonoscopy Costs Does Medicare Cover
Medicare covers all costs associated with a colonoscopy screening for colorectal cancer so long as the doctor who does it accepts Medicare.
The Affordable Care Act
Regardless of the insurance you are having, the Affordable Care Act mandates the insurance providers to follow the guidelines of the U.S. Preventive Services Task Force for coverage. If the screening test has received an A or B rating by this agency, private insurance companies would cover the cost of the test without charging a co-pay.
What Are The Screening Guidelines For Cologuard Under Medicare
The U.S. Preventative Services Task Force guidelines for screening for colorectal cancer do NOT include the testing of stool DNA. On the other hand, several agencies and societies do review these tests.
Medicaid Coverage For Colorectal Cancer Screening
States are authorized to cover colorectal screening under their Medicaid programs. But unlike Medicare, theres no federal assurance that all state Medicaid programs must cover colorectal cancer screening in people without symptoms. Medicaid coverage for colorectal cancer screening varies by state.
Who Needs A Colonoscopy
The U.S. Preventive Services Task Force recommends that people at average risk of colorectal cancer should have regular colonoscopies starting at age 50. The American Cancer Society recommends people start screening at 45.
How to contact insurance for colonoscopy?
If you receive a bill for a follow-up colonoscopy, please call our Customer Care Center 24/7 at 1-844-870-8870 or visit our appeals page to create a customized letter to send to your insurance company.
How to find out what is covered by my insurance?
It can vary based on your insurer’s medical policy, your specific benefits, deductibles and amounts you may have already incurred against a deductible, and other factors. The best way to find out is to call your insurer directly, but here is some information as of March 2021 about major plans and relevant state laws:
Does Medicare cover colonoscopy?
People with Medicare Advantage may receive a bill for a follow-up colonoscopy that includes co-insurance (in varying amounts, depending on the plan) and a deductible.
Does Cologuard cost out of pocket?
Currently, 80% of Cologuard patients 45-49 have had no out-of-pocket cost for screening.*. Special Topic: Insurance for Follow-up Colonoscopy. It is important that you fully complete your colon cancer screening. If you have a positive Cologuard test result, you should discuss it with your healthcare provider and have a follow-up colonoscopy.
Can you use Cologuard with Medicaid?
Eligible patients who are actively enrolled in any State Medicaid program can access Cologuard. No payment will be expected from the patient unless the plan requires a co-pay.*
Does Exact Sciences pay for colon cancer screening?
Many national and regional insurers have begun paying for colon cancer screening at 45. Exact Sciences continues to work with payers to expand coverage and access for patients 45-49.
Is Cologuard covered by Medicare?
Cologuard is covered by Medicare and Medicare Advantage with no co-pay or deductible for eligible patients ages 50-85. Payor. State. Traditional Medicare. National. Medicare Advantage. National. Medicaid | See details. Eligible patients who are actively enrolled in any State Medicaid program can access Cologuard.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. of your doctor’s services and a.
How to find out how much a test is?
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like: 1 Other insurance you may have 2 How much your doctor charges 3 Whether your doctor accepts assignment 4 The type of facility 5 Where you get your test, item, or service
What is assignment in colonoscopy?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. . However, if a polyp or other tissue is found and removed during the colonoscopy, you may pay 20% of the.
What is a copayment?
of your doctor’s services and a. copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage.
How often does Medicare pay for stool test?
Medicare starts paying for screenings at the age of 50 until 85 years or older. Stool DNA tests are otherwise known as Cologuard. Those showing no colorectal cancer symptoms or increased risks may get one Cologuard check every three years.
How much does a colonoscopy cost?
The bill following a colonoscopy for an uninsured person can range from as low as $600 to more than $5,000. Out-of-pocket costs are different depending on location, CPT codes, and how long it takes. Self-pay patients should consider all the fees and compare rates before shelling out hundreds or thousands of dollars.
How much does Medicare pay?
Medicare pays 80% of the allowable costs, and you’re going to pay the remaining 20%. Part C offers similar or better coverage when using in-network doctors.
What percentage of Medicare pays for outpatient services?
Those with Parts A and B insurance typically pay 20% of the price for each service allowable by Medicare. The other 80% is under either Part A or B. Inpatient, and hospital services fall under Part A insurance; Part B pays for diagnostic and outpatient services. Medicare Advantage plans may help with some out of pocket costs.
How often do you get a colonoscopy?
After reaching one of Medicare’s requirements, at-risk patients are covered for one colonoscopy every two years, with zero out-of-pocket costs.
Does Medicare pay for colonoscopy?
Getting right to it, yes, Medicare pays for colonoscopies. Coverage includes a broad range of preventive care services, including screenings. Part B pays for colonoscopy coverage for screening services like colorectal cancer testing. Doctors use preventive tests to help expose diseases during their earliest stages.
Does Part B deductible apply to cancer?
However, coverage is only when your doctor accepts the assignment. Meaning, the Part B deductible doesn’t apply. Over 4,500 Americans get cancer diagnosis every day, and the risk grows with age. Screenings and cancer treatments are part ...
How much does a Cologuard DNA test cost?
The cost of the Cologuard DNA Test is $599. This includes cost of shipping the kit to your home and the return shipping of back costs.
What is a cologuard?
Cologuard is a laboratory test where the specimens are collected in the comfort of your home. A kit with instructions is mailed to you upon submission of an order. ColonoscopyAssist currently accepts orders from all 50 states.
What does a positive colonoguard mean?
Positive Result : A positive result means that there is a high chance of Colorectal Cancer or precancer being present. You will be asked to follow up with a diagnostic colonoscopy.
How long does it take to get lab results from a lab?
Reports are available within 2 weeks after the lab receives the specimen. On average, you receive results approximately 1 month after placing your order .
Is Cologuard a noninvasive test?
Cologuard is an easy noninvasive colon cancer screening test that can be used at home. The advanced DNA test was FDA approved in 2014 after the most extensive study ever conducted and was quickly approved by Medicare, and was put on American Cancer Societies list of approved colorectal cancer screening tests ( Link ).
Is Cologuard a replacement for colonoscopy?
That being said, Cologuard is not for everyone. It is not a replacement for diagnostic or surveillance colonoscopy in patients at high risk for colorectal cancer .
Can you order Cologuard with a physician?
Yes. Cologuard can only be ordered with a physician referral. You will need to provide either a referral or your providers information.