
In this case, the most the provider is permitted to charge the patient is 115% of the allowable fee. At the current Medicare reimbursement rate of $96.01 for a 99214 visit and $63.73 for a 99213 visit, a physician who undercodes just one level 4 visit per day could lose as much as $8,393 over the course of a year.
Full Answer
How do I request Medicare reimbursement for a doctor's visit?
If this happens, contact the doctor and find out if they accept Medicare assignment and if and when they plan to submit the claim to Medicare. If they do not intend to submit the claim, request an itemized receipt so you can file a request for reimbursement. Medicare Reimbursement for Physicians Doctor visits fall under Part B.
What percentage of Medicare reimbursement goes to specialty care?
For example, clinical nurse specialists are reimbursed at 85% for most services, while clinical social workers receive 75%. 1 Medicare uses a coded number system to identify health care services and items for reimbursement.
What is the reimbursement rate for Medicare and Medicaid?
According to the Centers for Medicare & Medicaid Services (CMS), Medicare’s reimbursement rate on average is roughly 80 percent of the total bill. 1 Not all types of health care providers are reimbursed at the same rate.
How many Medicare payments are still tied to face-to-face visits?
"Based on the current average frequency with which Medicare beneficiaries make primary care office visits, this means that more than 40% of a typical practice's payments would still be tied to face-to-face visits.
What is the average Medicare reimbursement rate?
roughly 80 percentAccording to the Centers for Medicare & Medicaid Services (CMS), Medicare's reimbursement rate on average is roughly 80 percent of the total bill. Not all types of health care providers are reimbursed at the same rate.
How much does Medicare reimburse for a 99213?
The most common codes a doctor will use for follow up office visits are 99213 (follow up office visit, low complexity) and 99214 (follow up office visit, moderate complexity). A 99213 pays $83.08 in this region ($66.46 from Medicare and $16.62 from the patient).
How do I find Medicare reimbursement rates?
You can search the MPFS on the federal Medicare website to find out the Medicare reimbursement rate for specific services, treatments or devices. Simply enter the HCPCS code and click “Search fees” to view Medicare's reimbursement rate for the given service or item.
How Much Does Medicare pay for 99214 in 2021?
$132.94By Christine Frey posted 12-09-2020 15:122021 Final Physician Fee Schedule (CMS-1734-F)Payment Rates for Medicare Physician Services - Evaluation and Management99213Office/outpatient visit est$93.5199214Office/outpatient visit est$132.9499215Office/outpatient visit est$185.9815 more rows•Dec 9, 2020
What is a reimbursement rate?
Reimbursement rates means the formulae to calculate the dollar allowed amounts under a value-based or other alternative payment arrangement, dollar amounts, or fee schedules payable for a service or set of services.
What is the RVU for 99213 in 2021?
0.97 1.3How the E/M code RVU increases could affect family physicians' payCode2020 work RVUs2021 work RVUs992120.480.7992130.971.3992141.51.92992152.12.86 more rows•Jan 18, 2021
How much is a 99214 visit?
Prices for Standard Primary Care ServicesCPT CodeCostDescription99212$70Standard 5-10 Minute Office Visit99213$95Standard 10-15 Minute Office Visit99214$130Standard 20-25 Minute Office Visit99215$180Standard 30-45 Minute Office Visit
Did Medicare reimbursement go up in 2021?
On December 27, the Consolidated Appropriations Act, 2021 modified the Calendar Year (CY) 2021 Medicare Physician Fee Schedule (MPFS): Provided a 3.75% increase in MPFS payments for CY 2021.
How much does Medicare reimburse for 99204?
CPT Code 99204 Reimbursement Rate (Medicare, 2022): $185.26 In the past years, this E/m code has been paid $169.93 by Medicare in 2021.
What is the reimbursement for 99204?
Internists selected the 99204 code for 51.93% of these encounters in 2019. The 2021 Medicare allowable reimbursement for this level of care is $169.93 and it is worth 2.6 work RVUs. This level of care requires moderate complexity MDM or a total of 45 - 59 minutes devoted to the encounter on the date of the visit.
Did Medicare reimbursement go up in 2022?
This represents a 0.82% cut from the 2021 conversion factor of $34.8931. However, it also reflects an increase from the initial 2022 conversion factor of $33.5983 announced in the 2022 Medicare physician fee schedule final rule.
What is Medicare Reimbursement?
If you’re on Medicare, your doctors will usually bill Medicare for any care you obtain. Medicare will then pay its rate directly to your doctor. Your doctor will only charge you for any copay, deductible, or coinsurance you owe.
How to get reimbursement for health insurance?
To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out. You can print it and fill it out by hand. The form asks for information about you, your claim, and other health insurance you have.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
What if my doctor doesn't bill Medicare?
If your doctor doesn’t bill Medicare directly, you can file a claim asking Medicare to reimburse you for costs that you had to pay.
What happens if you see a doctor in your insurance network?
If you see a doctor in your plan’s network, your doctor will handle the claims process. Your doctor will only charge you for deductibles, copayments, or coinsurance. However, the situation is different if you see a doctor who is not in your plan’s network.
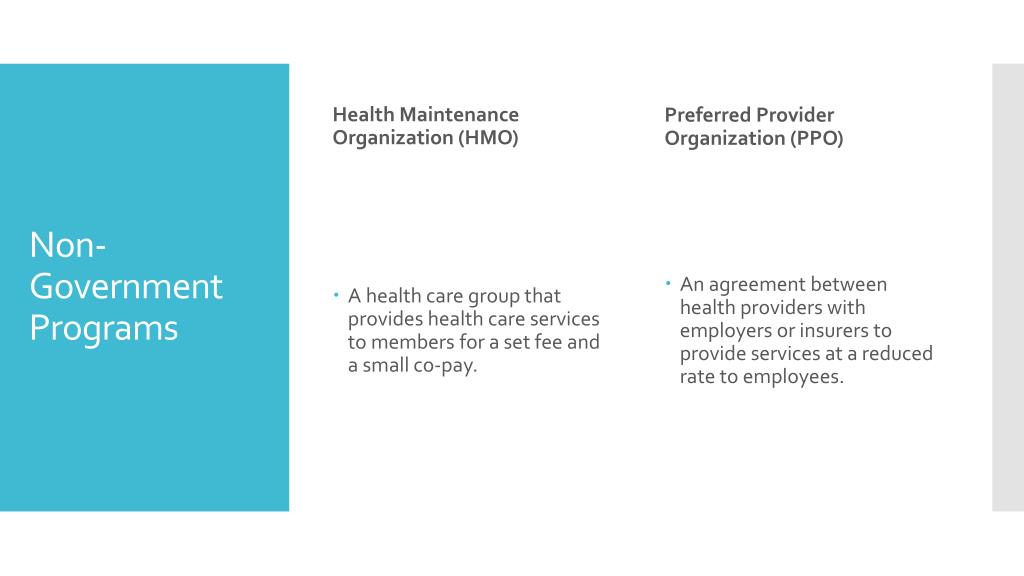
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Who will get the biggest Medicare cut?
Anesthesiologists, critical care and emergency medicine providers, respiratory specialists, radiologists and lab pathologists will be among the practitioners facing the biggest Medicare payment cuts under the policy, according to the American Hospital Association (AHA).
What is CMS 2020?
For performance year 2020, CMS will provide automatic full credit for CAHPS patient-experience-of-care surveys.
Does Medicare shift payments to primary care physicians?
Medicare shifts payments toward primary care physicians in PFS final rule. Many specialty physicians — and the hospitals that employ them — will see big Medicare payment cuts in January under a newly finalized payment rule.
What is the new code for home blood pressure?
The two new codes—99473 and 99474 —support home blood-pressure monitoring, which provides useful information physicians can use to better diagnose and manage hypertension. Home BP monitoring also helps patients to take an active role in the process.
How many readings are required for a 99474?
99474: separate self-measurements of two readings one minute apart, twice daily over a 30-day period (minimum of 12 reading s), collection of data reported by the patient and/or caregiver to the physician or other qualified health care professional, with the report of average systolic and diastolic pressures and subsequent communication of a treatment plan to the patient.
What is CPT code?
The technique by which Current Procedural Terminology (CPT) codes are developed with the goal that physicians can get paid for the services and procedures they give is an extremely entangled procedure, one that deserves some explaining. Furthermore, Medical Billers and Coders (MBC) is effectively occupied with this procedure and advocates for the eventual benefits of its clients, which incorporates improved payment for primary care and subspecialists under Medicare.
What is G2064 in healthcare?
G2064: Comprehensive care management services for a single high-risk disease, e.g., Principal Care Management, at least 30 minutes of physician or other qualified health care professional time per calendar month with the following elements: One complex chronic condition lasting at least 3 months;
What is a 99457?
99457: Remote physiologic monitoring treatment management services, clinical staff/physician/other qualified health care professional time in a calendar month requiring interactive communication with the patient/caregiver during the month; first 20 minutes;
What is primary care first?
The Primary Care First program, which was announced April 22 by the Centers for Medicare & Medicaid Services (CMS), has two models, both of which would let primary care clinicians move away from fee-for-service and allow them to stop worrying about up-and-down Medicare revenue, according to the CMS.
How can primary care be improved?
For starters, "rather than creating a whole new set of office visit payments, what primary care practices have asked for is to get all or most of their payments as a flexible monthly payment so it's not tied to office visits."
What is the second model of hospice?
One of the models focuses on a more general population, while the second model is for advanced primary care practices that typically provide hospice or palliative care services and want to take responsibility for high-need, seriously ill beneficiaries who currently lack a primary care practitioner and/or effective care coordination, according to a CMS fact sheet on the models .
Is Medicare revenue neutral?
And in addition to those issues, since Medicare payment programs are expected to be revenue-neutral compared with the current budget, "the payment is intended to be the same as what the practice is currently getting," although the practice will be expected to provide more services than before, including 24/7 patient access and integrated behavioral healthcare, Miller said.
Does Medicare pay for office visits?
WASHINGTON -- Medicare's new " Primary Care First " program for paying primary care doctors who see Medicare patients maintains a fee for office visits while also paying a monthly per-beneficiary amount for care coordination and other "behind the scenes" work that doctors do. So what's not to like?
Should the monthly payment be higher for patients?
"The way that happens today is more office visits ... but we don't want to pay more only if they come to the office."
Does primary care receive the same monthly payment?
Another problem with the program is that a primary care practice would receive the exact same monthly payment for a patient regardless of how sick or healthy they are , Miller said. "Since an individual patient who has higher needs will require more time and resources from the practice than other patients, a practice that is caring for that patient will have to reduce the time and resources it devotes to other patients if the payment is the same."
